Abstract
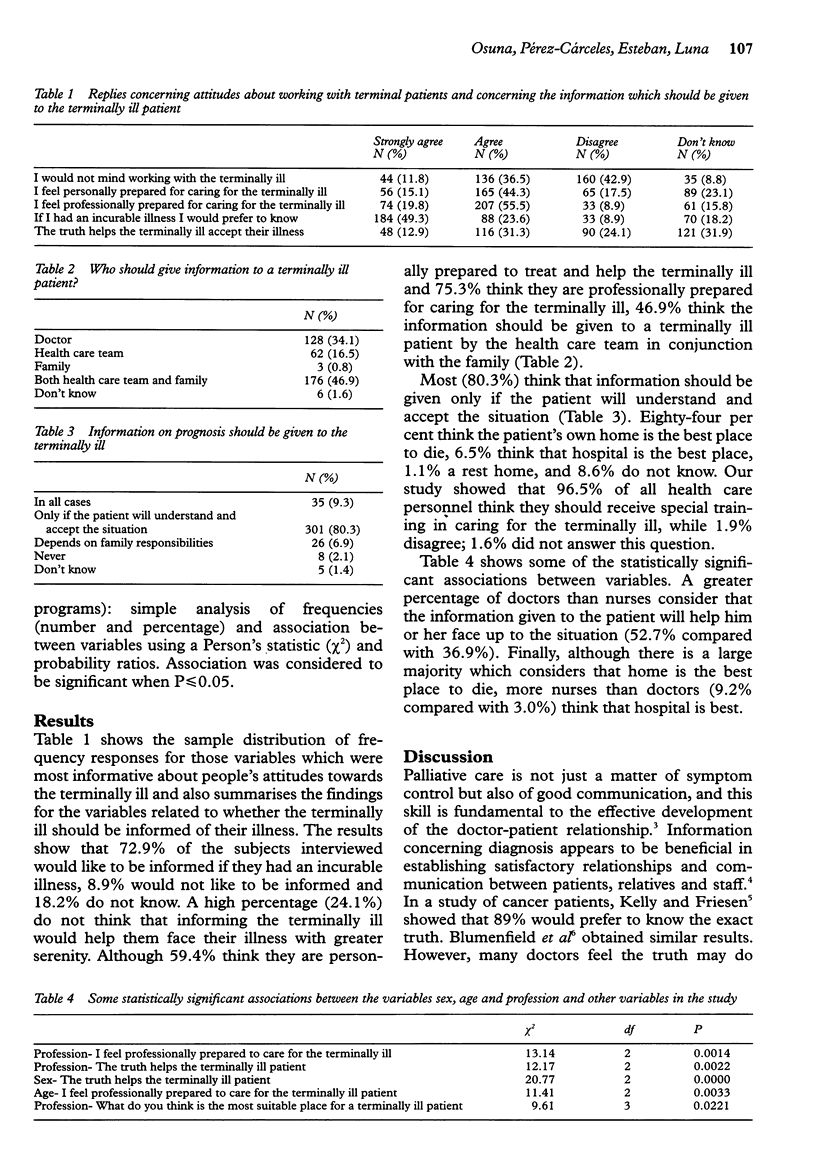
OBJECTIVES: To analyse the attitudes of medical personnel towards terminally ill patients and their right to be fully informed. DESIGN: Self-administered questionnaire composed of 56 closed questions. SETTING: Three general hospitals and eleven health centres in Granada (Spain). The sample comprised 168 doctors and 207 nurses. RESULTS: A high percentage of medical personnel (24.1%) do not think that informing the terminally ill would help them face their illness with greater serenity. Eighty-four per cent think the patient's own home is the best place to die: 8.9% of the subjects questioned state that the would not like to be informed of an incurable illness. CONCLUSION: In our opinion any information given should depend on the patient's personality, the stage of the illness and family circumstances. Our study confirms that a hospital is not the ideal environment for attending to the needs of the terminally ill and their families.
Full text
PDF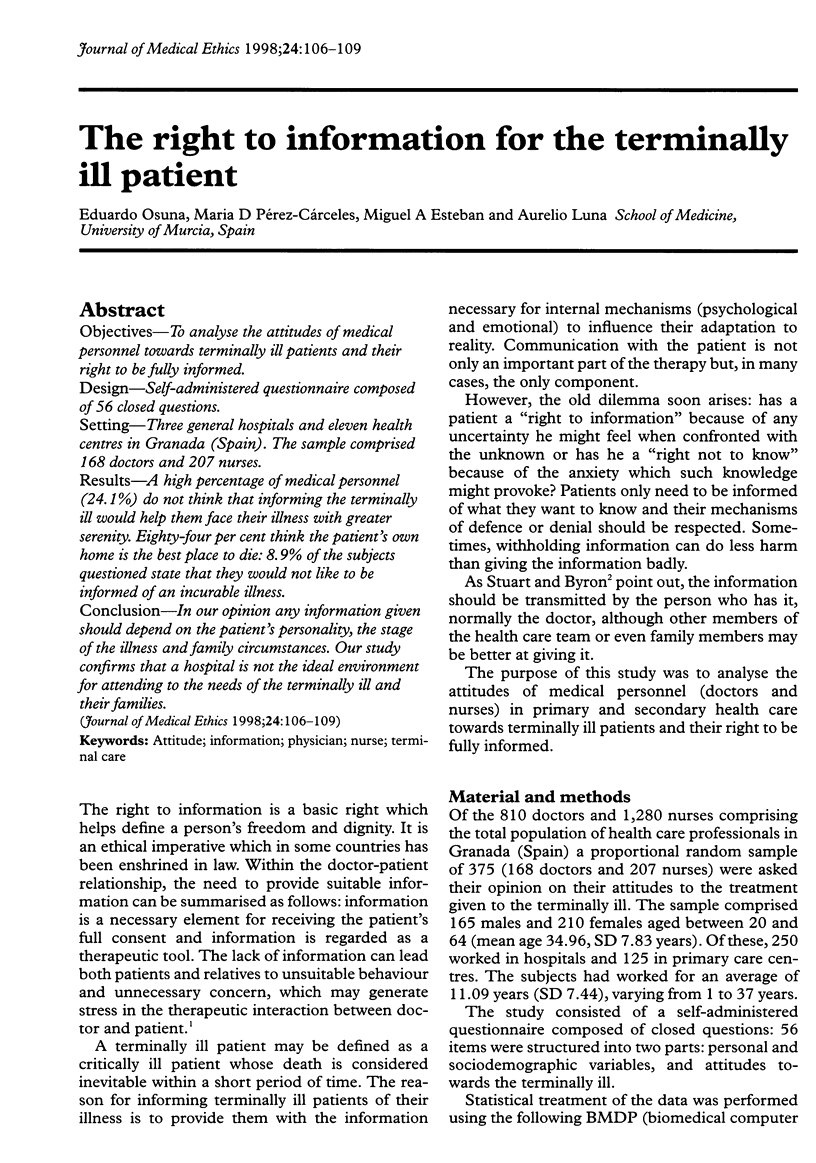

Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Blackhall L. J., Murphy S. T., Frank G., Michel V., Azen S. Ethnicity and attitudes toward patient autonomy. JAMA. 1995 Sep 13;274(10):820–825. [PubMed] [Google Scholar]
- Blumenfield M., Levy N. B., Kaufman D. Do patients want to be told? N Engl J Med. 1978 Nov 16;299(20):1138–1138. doi: 10.1056/NEJM197811162992024. [DOI] [PubMed] [Google Scholar]
- Bulkin W., Lukashok H. Training physicians to care for the dying. Am J Hosp Palliat Care. 1991 Mar-Apr;8(2):10–15. doi: 10.1177/104990919100800213. [DOI] [PubMed] [Google Scholar]
- Centeno-Cortés C., Núez-Olarte J. M. Questioning diagnosis disclosure in terminal cancer patients: a prospective study evaluating patients' responses. Palliat Med. 1994;8(1):39–44. doi: 10.1177/026921639400800107. [DOI] [PubMed] [Google Scholar]
- Charlton R. C. Using role-plays to teach palliative medicine. Med Teach. 1993;15(2-3):187–193. doi: 10.3109/01421599309006713. [DOI] [PubMed] [Google Scholar]
- Charlton R. Education about death and dying at Otago University Medical School. N Z Med J. 1993 Oct 27;106(966):447–449. [PubMed] [Google Scholar]
- Charlton R., Ford E. Education needs in palliative care. Fam Pract. 1995 Mar;12(1):70–74. doi: 10.1093/fampra/12.1.70. [DOI] [PubMed] [Google Scholar]
- Dent T. H., Gillard J. H., Aarons E. J., Crimlisk H. L., Smyth-Pigott P. J. Preregistration house officers in the four Thames regions: I. Survey of education and workload. BMJ. 1990 Mar 17;300(6726):713–716. doi: 10.1136/bmj.300.6726.713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eve A., Smith A. M., Tebbit P. Hospice and palliative care in the UK 1994-5, including a summary of trends 1990-5. Palliat Med. 1997 Jan;11(1):31–43. doi: 10.1177/026921639701100104. [DOI] [PubMed] [Google Scholar]
- Fitch M. I. How much should I say to whom? J Palliat Care. 1994 Autumn;10(3):90–100. [PubMed] [Google Scholar]
- KELLY W. D., FRIESEN S. R. Do cancer patients want to be told? Surgery. 1950 Jun;27(6):822–826. [PubMed] [Google Scholar]
- Lind S. E., DelVecchio Good M. J., Seidel S., Csordas T., Good B. J. Telling the diagnosis of cancer. J Clin Oncol. 1989 May;7(5):583–589. doi: 10.1200/JCO.1989.7.5.583. [DOI] [PubMed] [Google Scholar]
- MacAdam D. B. Teaching palliative medicine. Med J Aust. 1992 Feb 3;156(3):192-3, 196. doi: 10.5694/j.1326-5377.1992.tb139706.x. [DOI] [PubMed] [Google Scholar]
- Moore M. K. Dying at home: a way of maintaining control for the person with ALS/MND. Palliat Med. 1993;7(4 Suppl):65–68. doi: 10.1177/0269216393007004S10. [DOI] [PubMed] [Google Scholar]
- Pfeifer M. P., Sidorov J. E., Smith A. C., Boero J. F., Evans A. T., Settle M. B. The discussion of end-of-life medical care by primary care patients and physicians: a multicenter study using structured qualitative interviews. The EOL Study Group. J Gen Intern Med. 1994 Feb;9(2):82–88. doi: 10.1007/BF02600206. [DOI] [PubMed] [Google Scholar]
- Pijnenborg L., van Delden J. J., Kardaun J. W., Glerum J. J., van der Maas P. J. Nationwide study of decisions concerning the end of life in general practice in The Netherlands. BMJ. 1994 Nov 5;309(6963):1209–1212. doi: 10.1136/bmj.309.6963.1209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rea M. Priscilla, Greenspoon Shirley, Spilka Bernard. Physicians and the terminal patient: some selected attitudes and behavior. Omega (Westport) 1975;6(4):291–302. doi: 10.2190/wraw-xv2x-xdre-ucdd. [DOI] [PubMed] [Google Scholar]


