Abstract
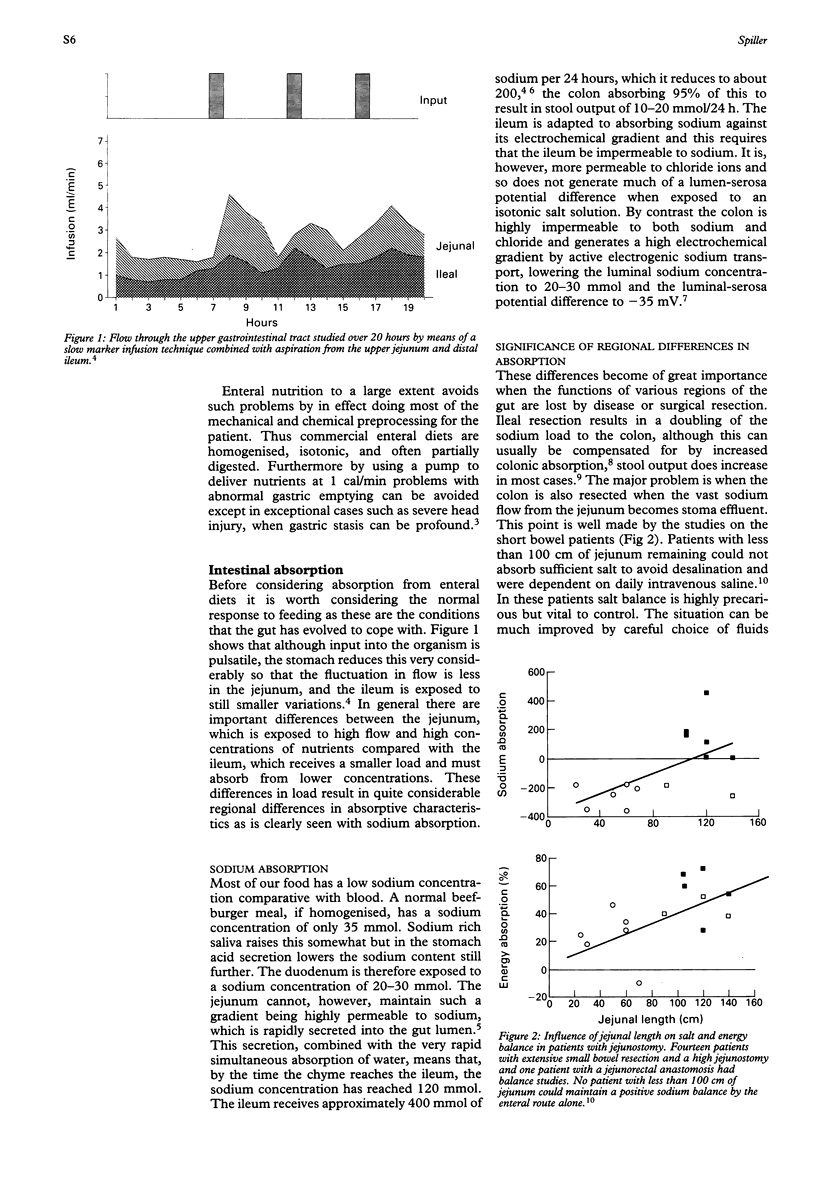
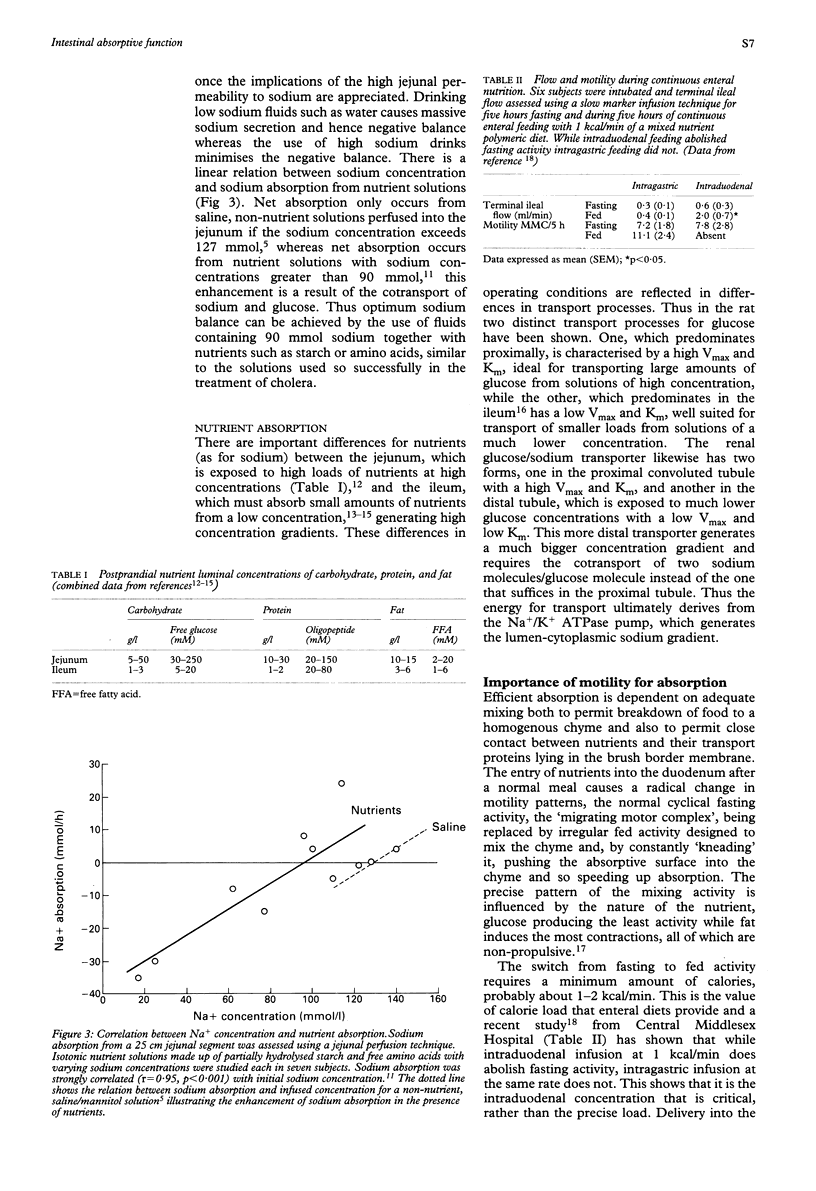
The normal gut is adapted to intermittent feeding with complex macromolecular substrates of low sodium content. The high permeability of the upper small intestine to sodium, together with sodium rich saliva and pancreaticobiliary secretions results in large sodium fluxes into the lumen. These substantial sodium influxes are matched by equally large effluxes from the ileum and proximal colon, which are comparatively impermeable to sodium and capable of active sodium absorption. Resection of these distal, sodium absorbing regions of the intestine, lead to problems with sodium depletion. Controlled transit of chyme is essential to permit time for optimum digestion and absorption and a range of feedback control mechanisms exist. Partially digested nutrients, both in the duodenum and ileum, exert inhibitory feedback to delay delivery of further nutrients and here again surgery may compromise these reflexes. Brush border hydrolase values are strongly influenced by luminal nutrient concentrations, being impaired by malnutrition and total parenteral nutrition, but restored by enteral feeding. Viscous fibre slows absorption and may delay transit through mechanisms that are as yet uncertain. Whether and how novel substrates activate normal control mechanisms will be important factors determining their effectiveness and patient acceptability.
Full text
PDF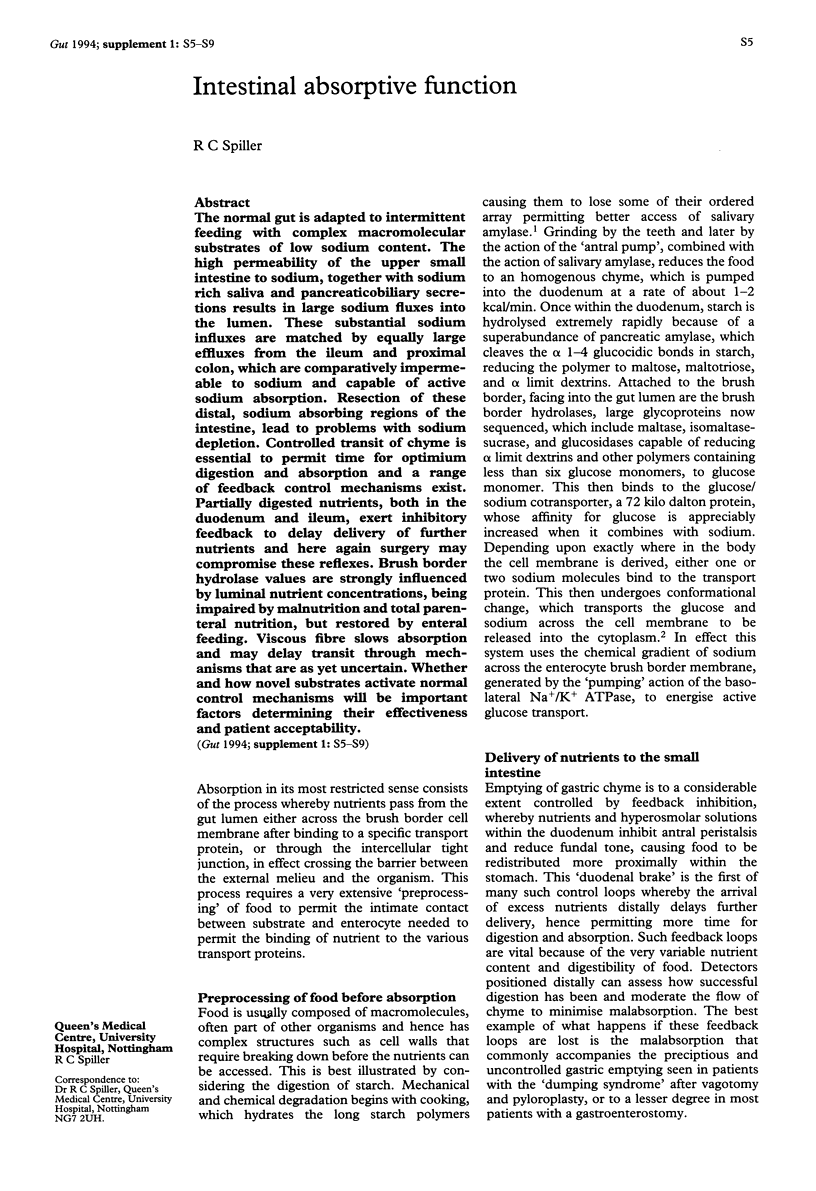

Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Adibi S. A., Mercer D. W. Protein digestion in human intestine as reflected in luminal, mucosal, and plasma amino acid concentrations after meals. J Clin Invest. 1973 Jul;52(7):1586–1594. doi: 10.1172/JCI107335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arrambide K. A., Santa Ana C. A., Schiller L. R., Little K. H., Santangelo W. C., Fordtran J. S. Loss of absorptive capacity for sodium chloride as a cause of diarrhea following partial ileal and right colon resection. Dig Dis Sci. 1989 Feb;34(2):193–201. doi: 10.1007/BF01536050. [DOI] [PubMed] [Google Scholar]
- BORGSTROM B., DAHLQVIST A., LUNDH G., SJOVALL J. Studies of intestinal digestion and absorption in the human. J Clin Invest. 1957 Oct;36(10):1521–1536. doi: 10.1172/JCI103549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baly D. L., Horuk R. The biology and biochemistry of the glucose transporter. Biochim Biophys Acta. 1988 Oct 11;947(3):571–590. doi: 10.1016/0304-4157(88)90008-1. [DOI] [PubMed] [Google Scholar]
- Blackburn N. A., Redfern J. S., Jarjis H., Holgate A. M., Hanning I., Scarpello J. H., Johnson I. T., Read N. W. The mechanism of action of guar gum in improving glucose tolerance in man. Clin Sci (Lond) 1984 Mar;66(3):329–336. doi: 10.1042/cs0660329. [DOI] [PubMed] [Google Scholar]
- Brown N. J., Read N. W., Richardson A., Rumsey R. D., Bogentoft C. Characteristics of lipid substances activating the ileal brake in the rat. Gut. 1990 Oct;31(10):1126–1129. doi: 10.1136/gut.31.10.1126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cortot A., Phillips S. F., Malagelada J. R. Parallel gastric emptying of nonhydrolyzable fat and water after a solid-liquid meal in humans. Gastroenterology. 1982 May;82(5 Pt 1):877–881. [PubMed] [Google Scholar]
- Cosnes J., Parquet M., Gendre J. P., Le Quintrec Y., Lévy E., Raizman A., Infante R., Loygue J. L'alimentation entérale continue réduit la diarrhée et la stéatorrhée des résections iléales. Gastroenterol Clin Biol. 1980 Oct;4(10):695–699. [PubMed] [Google Scholar]
- Davis G. R., Santa Ana C. A., Morawski S. G., Fordtran J. S. Permeability characteristics of human jejunum, ileum, proximal colon and distal colon: results of potential difference measurements and unidirectional fluxes. Gastroenterology. 1982 Oct;83(4):844–850. [PubMed] [Google Scholar]
- Debongnie J. C., Phillips S. F. Capacity of the human colon to absorb fluid. Gastroenterology. 1978 Apr;74(4):698–703. [PubMed] [Google Scholar]
- Dreznik Z., Brocksmith D., Meininger T. A., Soper N. J. Inhibitory effect of ileal oleate on postprandial motility of the upper gut. Am J Physiol. 1991 Sep;261(3 Pt 1):G458–G463. doi: 10.1152/ajpgi.1991.261.3.G458. [DOI] [PubMed] [Google Scholar]
- Emonts P., Vidon N., Bernier J. J., Rambaud J. C. Etude sur 24 heures des flux liquidiens intestinaux chez l'homme normal par la technique de la perfusion lente d'un marqueur non asorbable. Gastroenterol Clin Biol. 1979 Feb;3(2):139–146. [PubMed] [Google Scholar]
- Fleming S. E., Vose J. R. Digestibility of raw and cooked starches from legume seeds using the laboratory rat. J Nutr. 1979 Dec;109(12):2067–2075. doi: 10.1093/jn/109.12.2067. [DOI] [PubMed] [Google Scholar]
- Fone D. R., Horowitz M., Read N. W., Dent J., Maddox A. The effect of terminal ileal triglyceride infusion on gastroduodenal motility and the intragastric distribution of a solid meal. Gastroenterology. 1990 Mar;98(3):568–575. doi: 10.1016/0016-5085(90)90275-6. [DOI] [PubMed] [Google Scholar]
- Freeman H. J., Quamme G. A. Age-related changes in sodium-dependent glucose transport in rat small intestine. Am J Physiol. 1986 Aug;251(2 Pt 1):G208–G217. doi: 10.1152/ajpgi.1986.251.2.G208. [DOI] [PubMed] [Google Scholar]
- Guedon C., Schmitz J., Lerebours E., Metayer J., Audran E., Hemet J., Colin R. Decreased brush border hydrolase activities without gross morphologic changes in human intestinal mucosa after prolonged total parenteral nutrition of adults. Gastroenterology. 1986 Feb;90(2):373–378. doi: 10.1016/0016-5085(86)90935-2. [DOI] [PubMed] [Google Scholar]
- Holgate A. M., Read N. W. Effect of ileal infusion of intralipid on gastrointestinal transit, ileal flow rate, and carbohydrate absorption in humans after ingestion of a liquid meal. Gastroenterology. 1985 Apr;88(4):1005–1011. doi: 10.1016/s0016-5085(85)80021-4. [DOI] [PubMed] [Google Scholar]
- Jenkins D. J., Wolever T. M., Leeds A. R., Gassull M. A., Haisman P., Dilawari J., Goff D. V., Metz G. L., Alberti K. G. Dietary fibres, fibre analogues, and glucose tolerance: importance of viscosity. Br Med J. 1978 May 27;1(6124):1392–1394. doi: 10.1136/bmj.1.6124.1392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kotler D. P., Levine G. M., Shiau Y. F. Effects of nutrients, endogenous secretions, and fasting on in vitro glucose uptake. Am J Physiol. 1980 Mar;238(3):G219–G227. doi: 10.1152/ajpgi.1980.238.3.G219. [DOI] [PubMed] [Google Scholar]
- Layer P., Zinsmeister A. R., DiMagno E. P. Effects of decreasing intraluminal amylase activity on starch digestion and postprandial gastrointestinal function in humans. Gastroenterology. 1986 Jul;91(1):41–48. doi: 10.1016/0016-5085(86)90436-1. [DOI] [PubMed] [Google Scholar]
- Mansbach C. M., 2nd, Cohen R. S., Leff P. B. Isolation and properties of the mixed lipid micelles present in intestinal content during fat digestion in man. J Clin Invest. 1975 Oct;56(4):781–791. doi: 10.1172/JCI108156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller L. J., Malagelada J. R., Go V. L. Postprandial duodenal function in man. Gut. 1978 Aug;19(8):699–706. doi: 10.1136/gut.19.8.699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nightingale J. M., Lennard-Jones J. E., Walker E. R., Farthing M. J. Jejunal efflux in short bowel syndrome. Lancet. 1990 Sep 29;336(8718):765–768. doi: 10.1016/0140-6736(90)93238-k. [DOI] [PubMed] [Google Scholar]
- Ott L., Young B., Phillips R., McClain C., Adams L., Dempsey R., Tibbs P., Ryo U. Y. Altered gastric emptying in the head-injured patient: relationship to feeding intolerance. J Neurosurg. 1991 May;74(5):738–742. doi: 10.3171/jns.1991.74.5.0738. [DOI] [PubMed] [Google Scholar]
- Phillips S. F., Giller J. The contribution of the colon to electrolyte and water conservation in man. J Lab Clin Med. 1973 May;81(5):733–746. [PubMed] [Google Scholar]
- Schemann M., Ehrlein H. J. Postprandial patterns of canine jejunal motility and transit of luminal content. Gastroenterology. 1986 Apr;90(4):991–1000. doi: 10.1016/0016-5085(86)90878-4. [DOI] [PubMed] [Google Scholar]
- Shinnick F. L., Hess R. L., Fischer M. H., Marlett J. Apparent nutrient absorption and upper gastrointestinal transit with fiber-containing enteral feedings. Am J Clin Nutr. 1989 Mar;49(3):471–475. doi: 10.1093/ajcn/49.3.471. [DOI] [PubMed] [Google Scholar]
- Spiller R. C., Jones B. J., Silk D. B. Jejunal water and electrolyte absorption from two proprietary enteral feeds in man: importance of sodium content. Gut. 1987 Jun;28(6):681–687. doi: 10.1136/gut.28.6.681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spiller R. C., Trotman I. F., Adrian T. E., Bloom S. R., Misiewicz J. J., Silk D. B. Further characterisation of the 'ileal brake' reflex in man--effect of ileal infusion of partial digests of fat, protein, and starch on jejunal motility and release of neurotensin, enteroglucagon, and peptide YY. Gut. 1988 Aug;29(8):1042–1051. doi: 10.1136/gut.29.8.1042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spiller R. C., Trotman I. F., Higgins B. E., Ghatei M. A., Grimble G. K., Lee Y. C., Bloom S. R., Misiewicz J. J., Silk D. B. The ileal brake--inhibition of jejunal motility after ileal fat perfusion in man. Gut. 1984 Apr;25(4):365–374. doi: 10.1136/gut.25.4.365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Welch I. M., Davison P. A., Worlding J., Read N. W. Effect of ileal infusion of lipid on jejunal motor patterns after a nutrient and nonnutrient meal. Am J Physiol. 1988 Dec;255(6 Pt 1):G800–G806. doi: 10.1152/ajpgi.1988.255.6.G800. [DOI] [PubMed] [Google Scholar]


