Abstract
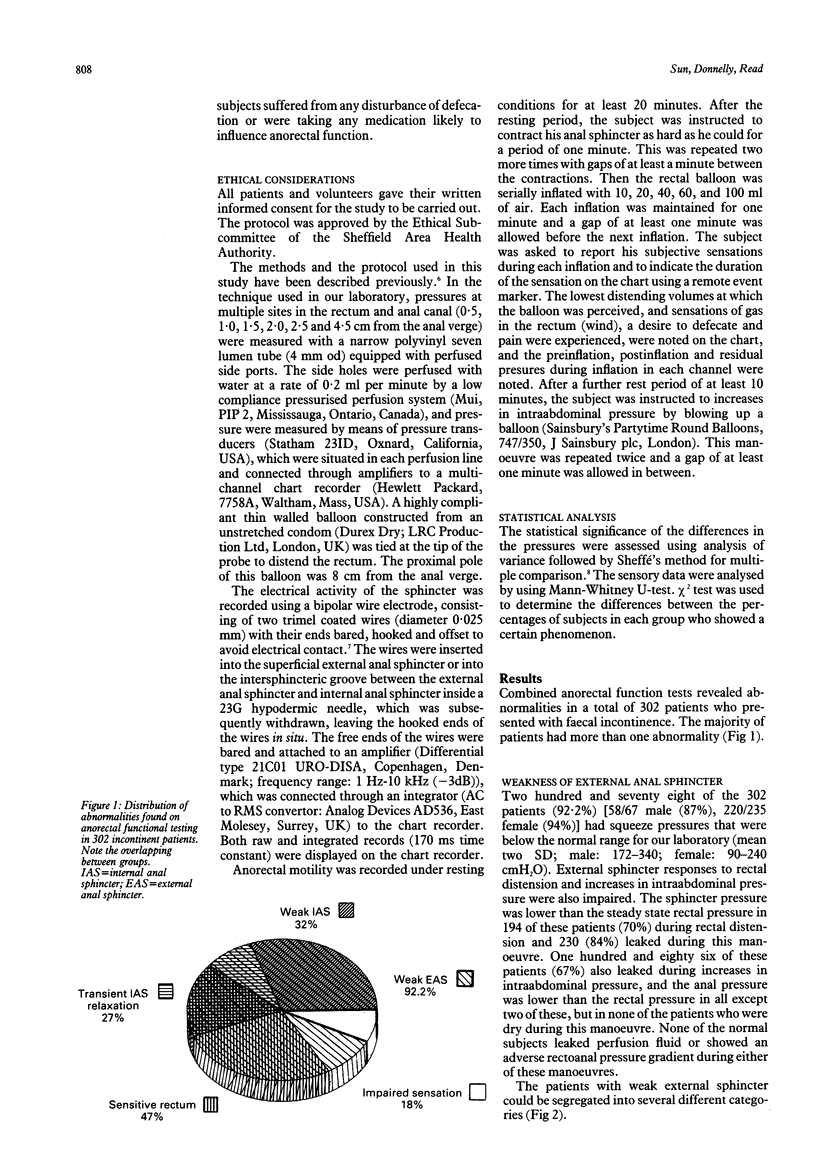
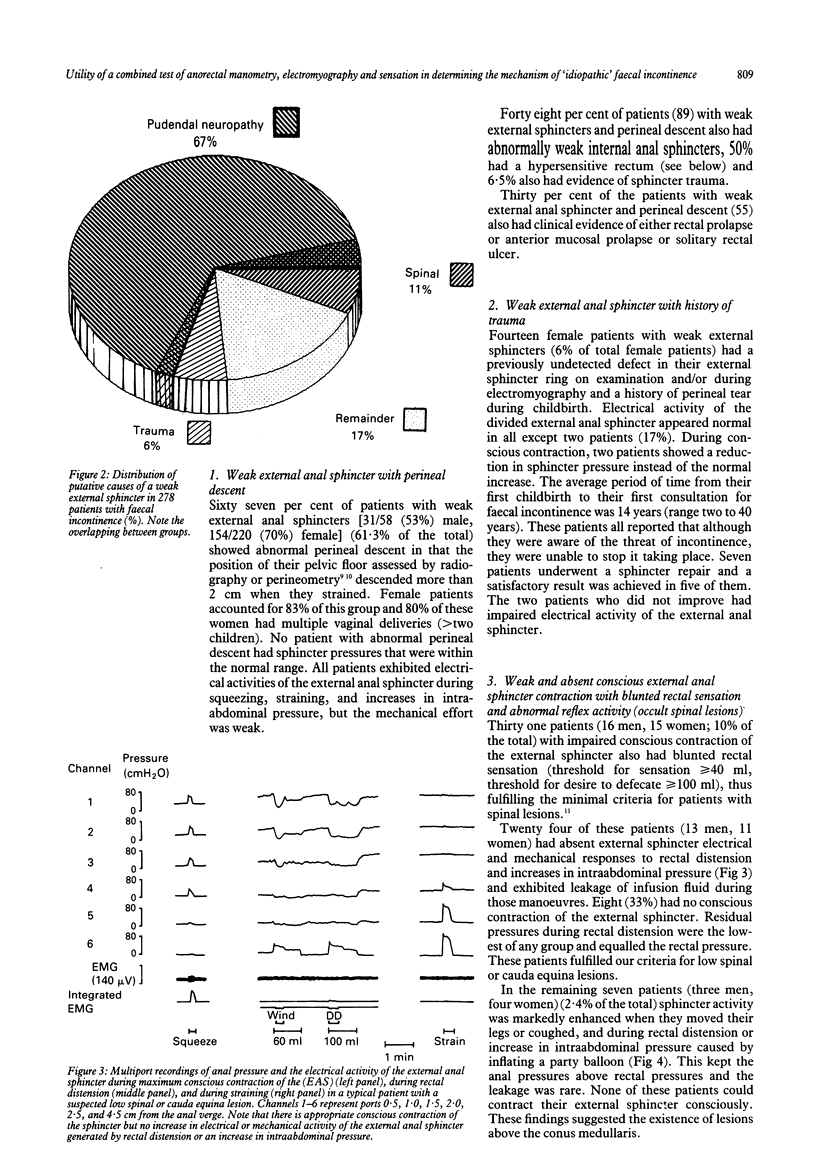
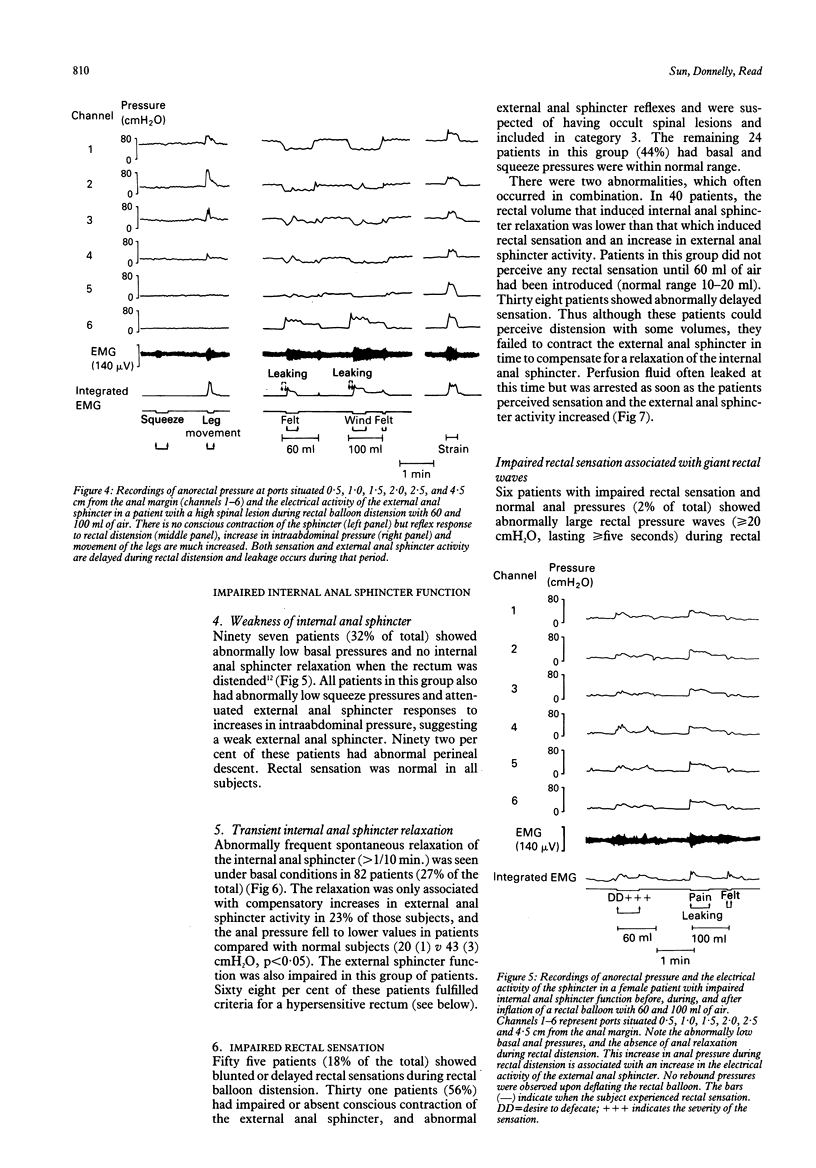
Combined tests of anorectal manometry, sphincter electromyography and rectal sensation were carried out in 302 patients with faecal incontinence (235 women, 67 men). The results obtained were compared with 65 normal subjects (35 women, 30 men). A mechanism for incontinence was identified in all and the majority of patients had more than one abnormality. Two hundred and seventy eight patients (92%) had a weak external anal sphincter, 185 of these (67%, mostly women) also showed abnormal perineal descent, and 14 women showed clinical evidence of sphincter damage as a result of obstetric trauma. Ten per cent of patients with impaired external anal sphincter contraction showed associated evidence of spinal disease (impaired rectal sensation plus attenuated or enhanced reflex external anal sphincter activity). Unlike the other groups, the 'spinal' group contained equal numbers of men and women. Ninety seven patients (32%) had evidence of a weak internal anal sphincter. The external sphincter was also very weak and 92% of these patients also had perineal descent. Eighty two patients (27%) showed an unstable internal sphincter, characterised by prolonged 'spontaneous' anal relaxation under resting conditions and an abnormal reduction in anal pressure after conscious contraction of the sphincter or an increase in intraabdominal pressure. One hundred and forty two patients (47%) had a hypersensitive rectum associated with enhanced anorectal responses to rectal distension. All these patients had an abnormally weak external sphincter, suggesting that the hypersensitive or 'irritable' rectum should not be regarded as a cause of faecal incontinence unless accompanied by external sphincter weakness. Twenty four patients (8%) showed a normal basal and squeeze pressures and impaired rectal sensation; six showed giant rectal contractions during rectal distension. The results show that idiopathic faecal incontinence is not caused by a single abnormality, and it is suggested that combined anorectal manometry, electromyography, and sensory testing is a useful technique to identify the causes of faecal incontinence and provide a basis for appropriate treatment.
Full text
PDF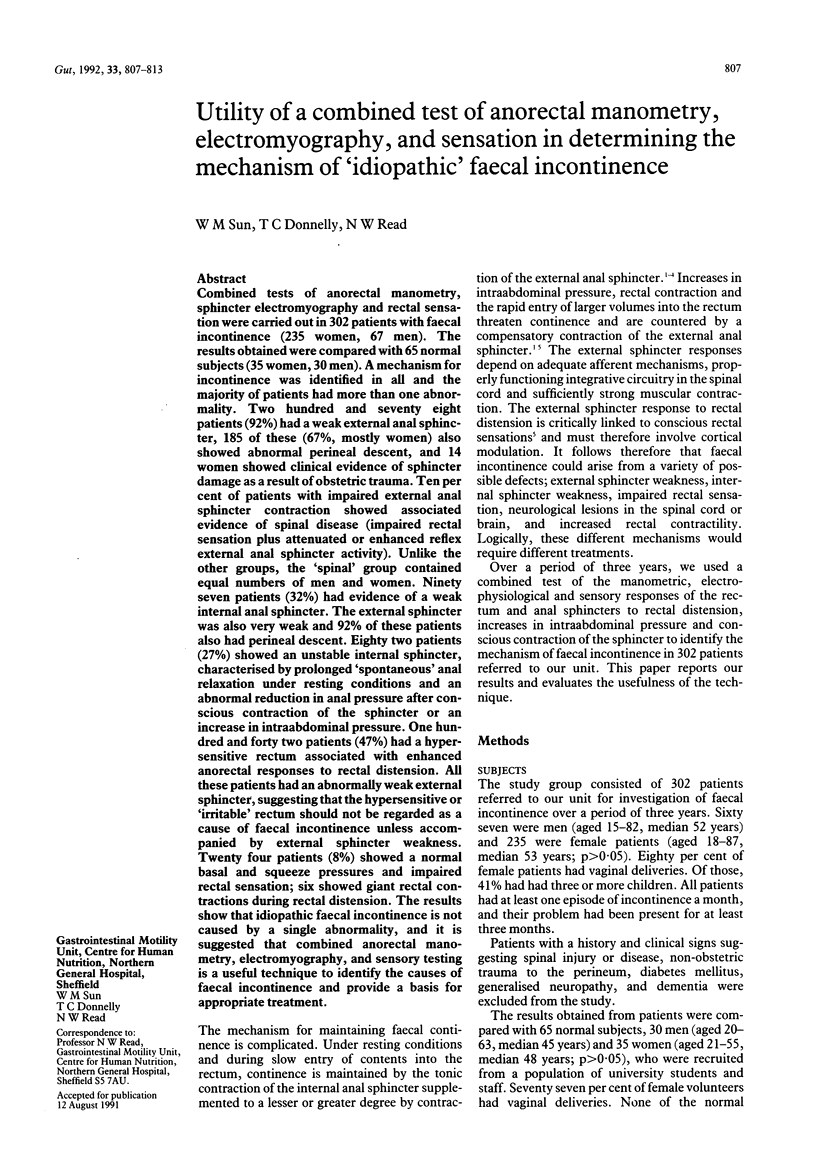
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- BENNETT R. C., DUTHIE H. L. THE FUNCTIONAL IMPORTANCE OF THE INTERNAL ANAL SPHINCTER. Br J Surg. 1964 May;51:355–357. doi: 10.1002/bjs.1800510514. [DOI] [PubMed] [Google Scholar]
- Bartolo D. C., Jarratt J. A., Read M. G., Donnelly T. C., Read N. W. The role of partial denervation of the puborectalis in idiopathic faecal incontinence. Br J Surg. 1983 Nov;70(11):664–667. doi: 10.1002/bjs.1800701108. [DOI] [PubMed] [Google Scholar]
- Bartolo D. C., Read N. W., Jarratt J. A., Read M. G., Donnelly T. C., Johnson A. G. Differences in anal sphincter function and clinical presentation in patients with pelvic floor descent. Gastroenterology. 1983 Jul;85(1):68–75. [PubMed] [Google Scholar]
- Bouvier M., Gonella J. Nervous control of the internal anal sphincter of the cat. J Physiol. 1981 Jan;310:457–469. doi: 10.1113/jphysiol.1981.sp013561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Christensen J., Rick G. A. Distribution of myelinated nerves in ascending nerves and myenteric plexus of cat colon. Am J Anat. 1987 Mar;178(3):250–258. doi: 10.1002/aja.1001780306. [DOI] [PubMed] [Google Scholar]
- Frenckner B., Euler C. V. Influence of pudendal block on the function of the anal sphincters. Gut. 1975 Jun;16(6):482–489. doi: 10.1136/gut.16.6.482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Henry M. M., Parks A. G., Swash M. The pelvic floor musculature in the descending perineum syndrome. Br J Surg. 1982 Aug;69(8):470–472. doi: 10.1002/bjs.1800690813. [DOI] [PubMed] [Google Scholar]
- Kiff E. S., Swash M. Slowed conduction in the pudendal nerves in idiopathic (neurogenic) faecal incontinence. Br J Surg. 1984 Aug;71(8):614–616. doi: 10.1002/bjs.1800710817. [DOI] [PubMed] [Google Scholar]
- Lestar B., Penninckx F., Kerremans R. The composition of anal basal pressure. An in vivo and in vitro study in man. Int J Colorectal Dis. 1989;4(2):118–122. doi: 10.1007/BF01646870. [DOI] [PubMed] [Google Scholar]
- Prior A., Maxton D. G., Whorwell P. J. Anorectal manometry in irritable bowel syndrome: differences between diarrhoea and constipation predominant subjects. Gut. 1990 Apr;31(4):458–462. doi: 10.1136/gut.31.4.458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Read N. W., Bartolo D. C., Read M. G. Differences in anal function in patients with incontinence to solids and in patients with incontinence to liquids. Br J Surg. 1984 Jan;71(1):39–42. doi: 10.1002/bjs.1800710112. [DOI] [PubMed] [Google Scholar]
- Ritchie J. Pain from distension of the pelvic colon by inflating a balloon in the irritable colon syndrome. Gut. 1973 Feb;14(2):125–132. doi: 10.1136/gut.14.2.125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schuster M. M. The riddle of the sphincters. Gastroenterology. 1975 Jul;69(1):249–262. [PubMed] [Google Scholar]
- Snooks S. J., Setchell M., Swash M., Henry M. M. Injury to innervation of pelvic floor sphincter musculature in childbirth. Lancet. 1984 Sep 8;2(8402):546–550. doi: 10.1016/s0140-6736(84)90766-9. [DOI] [PubMed] [Google Scholar]
- Sun W. M., Read N. W. Anorectal function in normal human subjects: effect of gender. Int J Colorectal Dis. 1989 Aug;4(3):188–196. doi: 10.1007/BF01649702. [DOI] [PubMed] [Google Scholar]
- Sun W. M., Read N. W., Donnelly T. C. Anorectal function in incontinent patients with cerebrospinal disease. Gastroenterology. 1990 Nov;99(5):1372–1379. doi: 10.1016/0016-5085(90)91164-2. [DOI] [PubMed] [Google Scholar]
- Sun W. M., Read N. W., Donnelly T. C., Bannister J. J., Shorthouse A. J. A common pathophysiology for full thickness rectal prolapse, anterior mucosal prolapse and solitary rectal ulcer. Br J Surg. 1989 Mar;76(3):290–295. doi: 10.1002/bjs.1800760323. [DOI] [PubMed] [Google Scholar]
- Sun W. M., Read N. W., Donnelly T. C. Impaired internal anal sphincter in a subgroup of patients with idiopathic fecal incontinence. Gastroenterology. 1989 Jul;97(1):130–135. doi: 10.1016/0016-5085(89)91425-x. [DOI] [PubMed] [Google Scholar]
- Sun W. M., Read N. W., Miner P. B. Relation between rectal sensation and anal function in normal subjects and patients with faecal incontinence. Gut. 1990 Sep;31(9):1056–1061. doi: 10.1136/gut.31.9.1056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sun W. M., Read N. W. Occult spinal lesions: a common undetected cause of faecal incontinence. Lancet. 1990 Jan 20;335(8682):166–166. doi: 10.1016/0140-6736(90)90037-6. [DOI] [PubMed] [Google Scholar]
- Sun W. M., Read N. W., Prior A., Daly J. A., Cheah S. K., Grundy D. Sensory and motor responses to rectal distention vary according to rate and pattern of balloon inflation. Gastroenterology. 1990 Oct;99(4):1008–1015. doi: 10.1016/0016-5085(90)90620-g. [DOI] [PubMed] [Google Scholar]
- Whitehead W. E., Engel B. T., Schuster M. M. Irritable bowel syndrome: physiological and psychological differences between diarrhea-predominant and constipation-predominant patients. Dig Dis Sci. 1980 Jun;25(6):404–413. doi: 10.1007/BF01395503. [DOI] [PubMed] [Google Scholar]


