Abstract
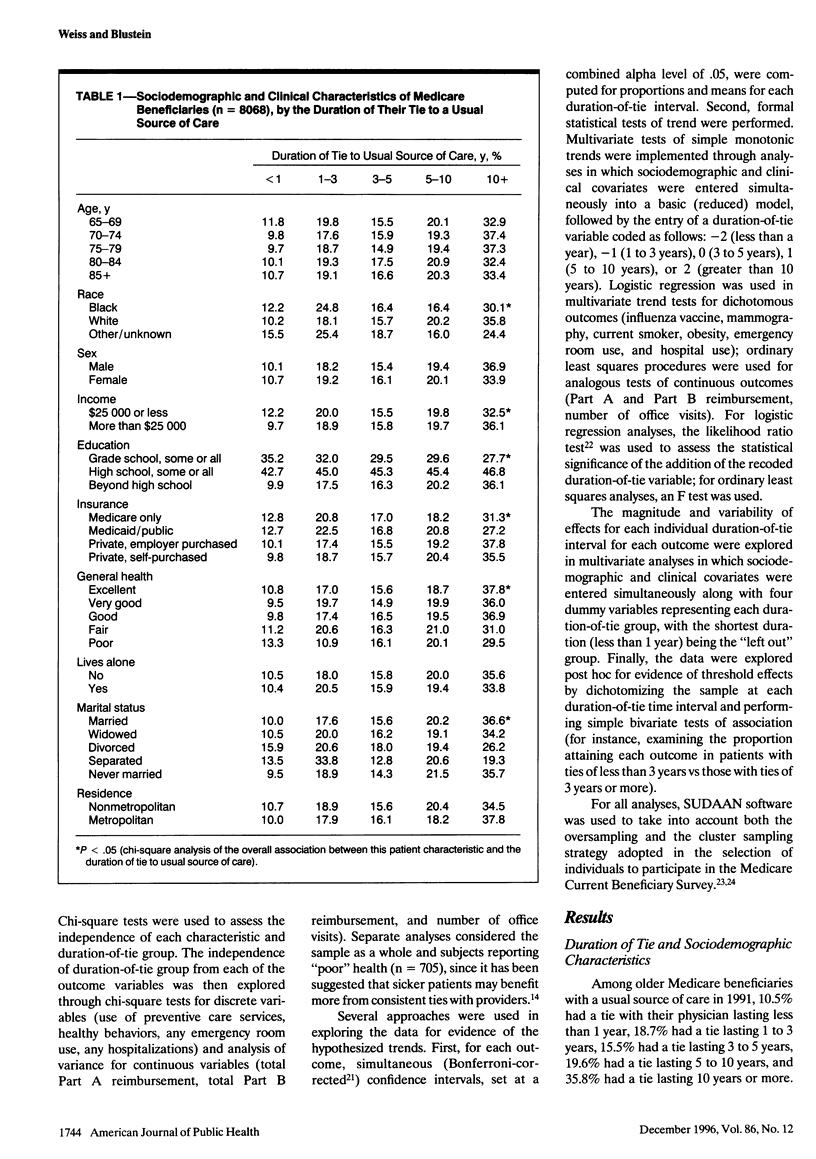
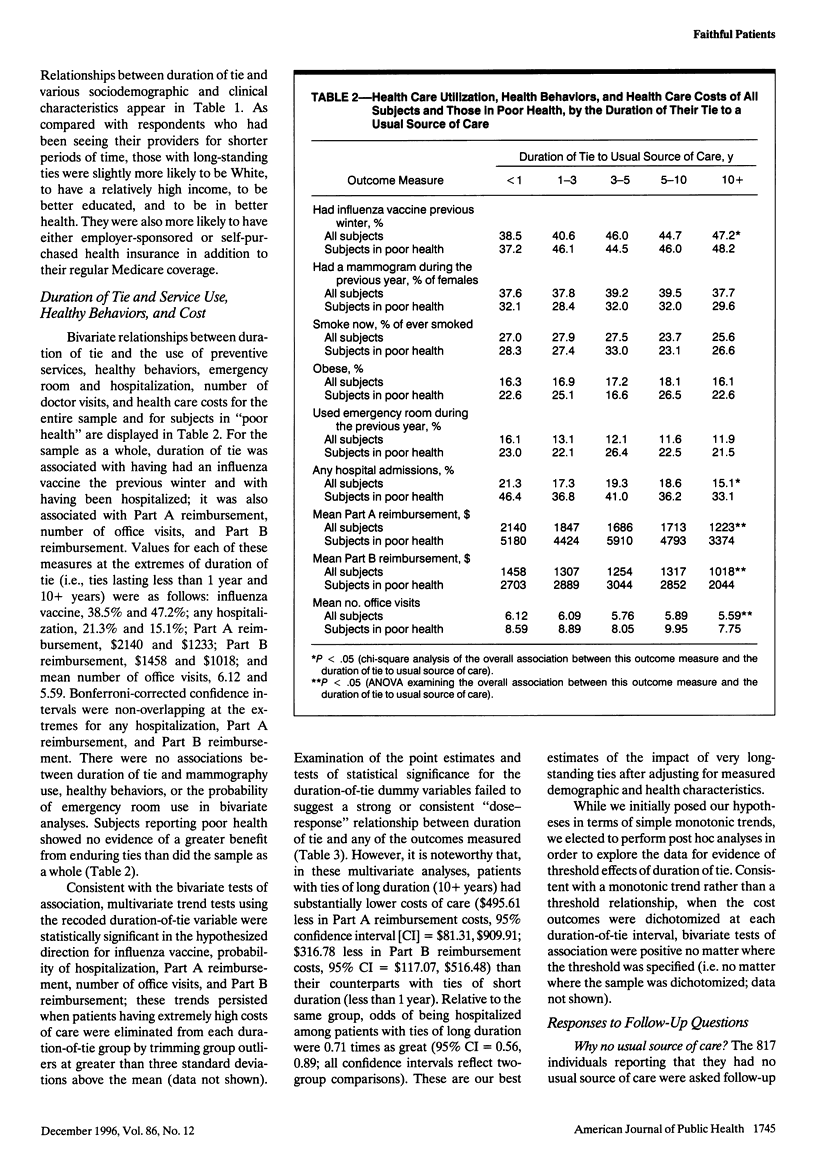
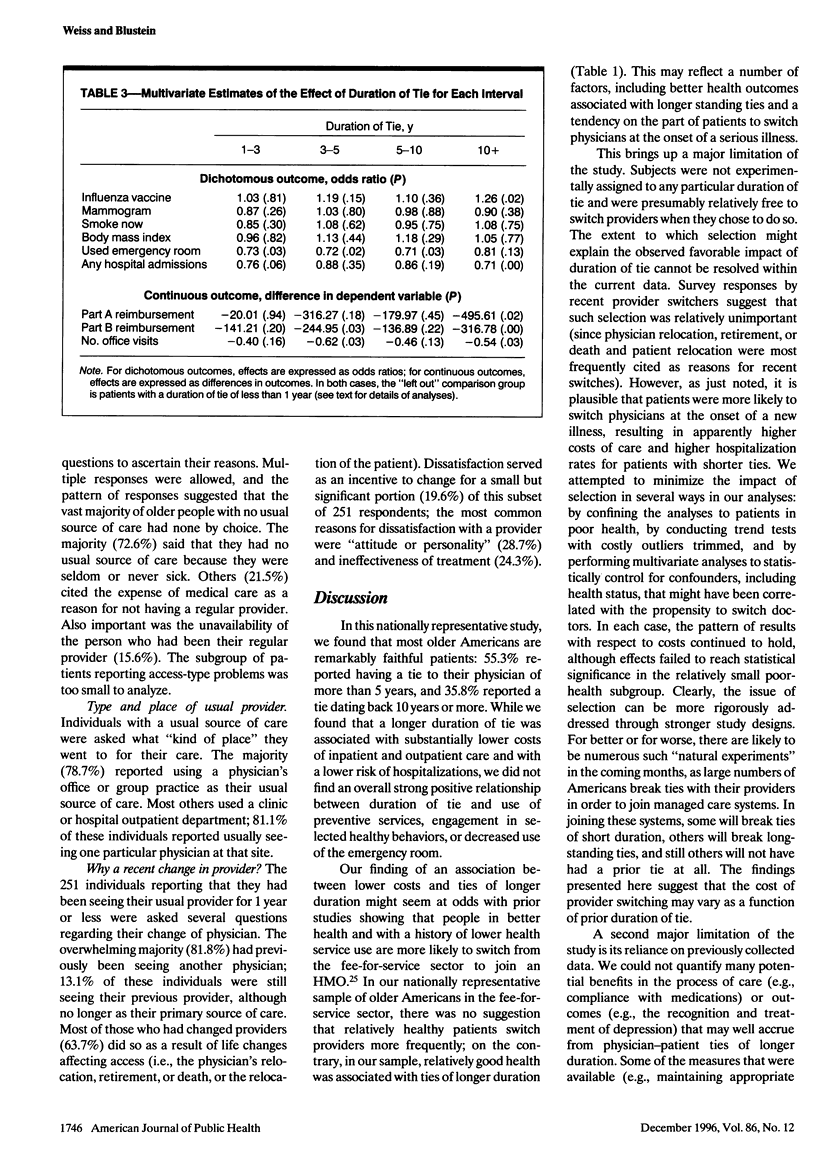
OBJECTIVES: This study examined the impact of duration of physician-patient ties on the processes and costs of medical care. METHODS: The analyses used a nationally representative sample of Americans 65 years old or older who participated in the Medicare Current Beneficiary Survey in 1991 and had a usual source of care. RESULTS: Older Americans have long-standing ties with their physicians; among those with a usual source of care, 35.8% had ties enduring 10 years or more. Longer ties were associated with a decreased likelihood of hospitalization and lower costs. Compared with patients with a tie of 1 year or less, patients with ties of 10 years or more incurred $316.78 less in Part B Medicare costs, after adjustment for key demographic and health characteristics. However, substantial impacts on the use of selected preventive care services and the adoption of certain healthy behaviors were not observed. CONCLUSIONS: This preliminary study suggests that long-standing physician-patient ties foster less expensive, less intensive medical care. Further studies are needed to confirm these findings and to understand how duration of tie influences the processes and outcomes of care.
Full text
PDF

Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Becker M. H., Drachman R. H., Kirscht J. P. A field experiment to evaluate various outcomes of continuity of physician care. Am J Public Health. 1974 Nov;64(11):1062–1070. doi: 10.2105/ajph.64.11.1062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Breslau N. Continuity reexamined: differential impact on satisfaction with medical care for disabled and normal children. Med Care. 1982 Apr;20(4):347–360. [PubMed] [Google Scholar]
- Breslau N., Mortimer E. A., Jr Seeing the same doctor: determinants of satisfaction with specialty care for disabled children. Med Care. 1981 Jul;19(7):741–758. doi: 10.1097/00005650-198107000-00005. [DOI] [PubMed] [Google Scholar]
- Burke W., Baron R. B., Lemon M., Losh D., Novack A. Training generalist physicians: structural elements of the curriculum. J Gen Intern Med. 1994 Apr;9(4 Suppl 1):S23–S30. doi: 10.1007/BF02598115. [DOI] [PubMed] [Google Scholar]
- Davis K., Collins K. S., Schoen C., Morris C. Choice matters: enrollees' views of their health plans. Health Aff (Millwood) 1995 Summer;14(2):99–112. doi: 10.1377/hlthaff.14.2.99. [DOI] [PubMed] [Google Scholar]
- Dietrich A. J., Marton K. I. Does continuous care from a physician make a difference? J Fam Pract. 1982 Nov;15(5):929–937. [PubMed] [Google Scholar]
- Emanuel E. J., Dubler N. N. Preserving the physician-patient relationship in the era of managed care. JAMA. 1995 Jan 25;273(4):323–329. [PubMed] [Google Scholar]
- Freeman G. K., Richards S. C. Is personal continuity of care compatible with free choice of doctor? Patients' views on seeing the same doctor. Br J Gen Pract. 1993 Dec;43(377):493–497. [PMC free article] [PubMed] [Google Scholar]
- Hellinger F. J. Selection bias in HMOs and PPOs: a review of the evidence. Inquiry. 1995 Summer;32(2):135–142. [PubMed] [Google Scholar]
- Hjortdahl P., Borchgrevink C. F. Continuity of care: influence of general practitioners' knowledge about their patients on use of resources in consultations. BMJ. 1991 Nov 9;303(6811):1181–1184. doi: 10.1136/bmj.303.6811.1181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hjortdahl P., Laerum E. Continuity of care in general practice: effect on patient satisfaction. BMJ. 1992 May 16;304(6837):1287–1290. doi: 10.1136/bmj.304.6837.1287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hurley R. E., Gage B. J., Freund D. A. Rollover effects in gatekeeper programs: cushioning the impact of restricted choice. Inquiry. 1991 Winter;28(4):375–384. [PubMed] [Google Scholar]
- Kibbe D. C., Bentz E., McLaughlin C. P. Continuous quality improvement for continuity of care. J Fam Pract. 1993 Mar;36(3):304–308. [PubMed] [Google Scholar]
- Law M., Tang J. L. An analysis of the effectiveness of interventions intended to help people stop smoking. Arch Intern Med. 1995 Oct 9;155(18):1933–1941. [PubMed] [Google Scholar]
- Leibel R. L., Rosenbaum M., Hirsch J. Changes in energy expenditure resulting from altered body weight. N Engl J Med. 1995 Mar 9;332(10):621–628. doi: 10.1056/NEJM199503093321001. [DOI] [PubMed] [Google Scholar]
- Moore S. H., Martin D. P., Richardson W. C. Does the primary-care gatekeeper control the costs of health care? Lessons from the SAFECO experience. N Engl J Med. 1983 Dec 1;309(22):1400–1404. doi: 10.1056/NEJM198312013092239. [DOI] [PubMed] [Google Scholar]
- Starfield B. Continuous confusion? Am J Public Health. 1980 Feb;70(2):117–119. doi: 10.2105/ajph.70.2.117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wasson J. H., Sauvigne A. E., Mogielnicki R. P., Frey W. G., Sox C. H., Gaudette C., Rockwell A. Continuity of outpatient medical care in elderly men. A randomized trial. JAMA. 1984 Nov 2;252(17):2413–2417. [PubMed] [Google Scholar]
- Wilson D. M., Taylor D. W., Gilbert J. R., Best J. A., Lindsay E. A., Willms D. G., Singer J. A randomized trial of a family physician intervention for smoking cessation. JAMA. 1988 Sep 16;260(11):1570–1574. [PubMed] [Google Scholar]


