Abstract
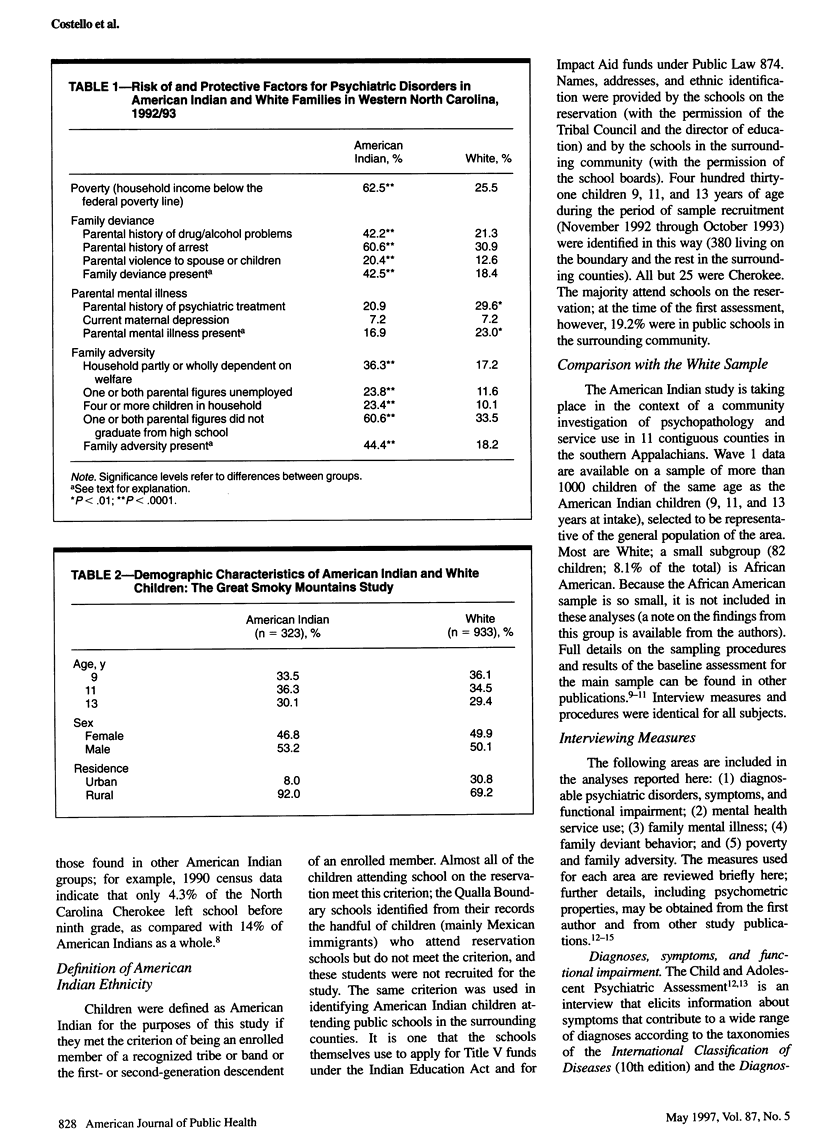
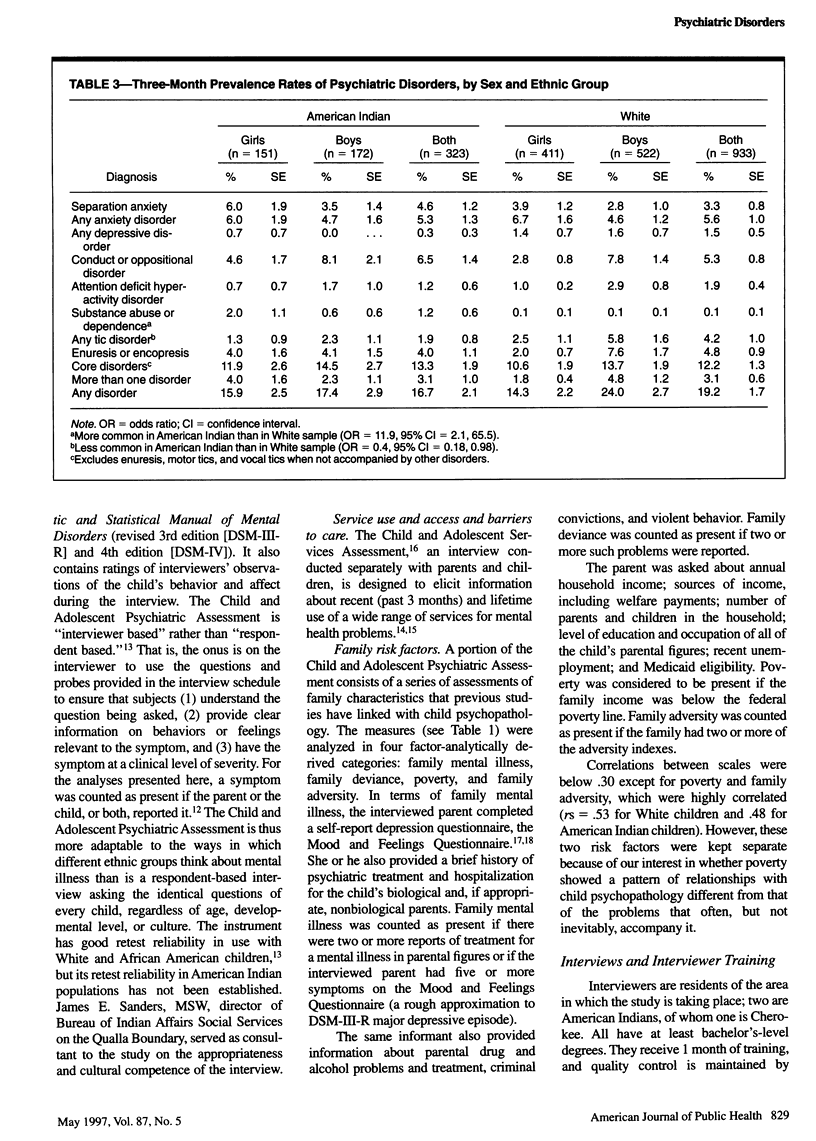
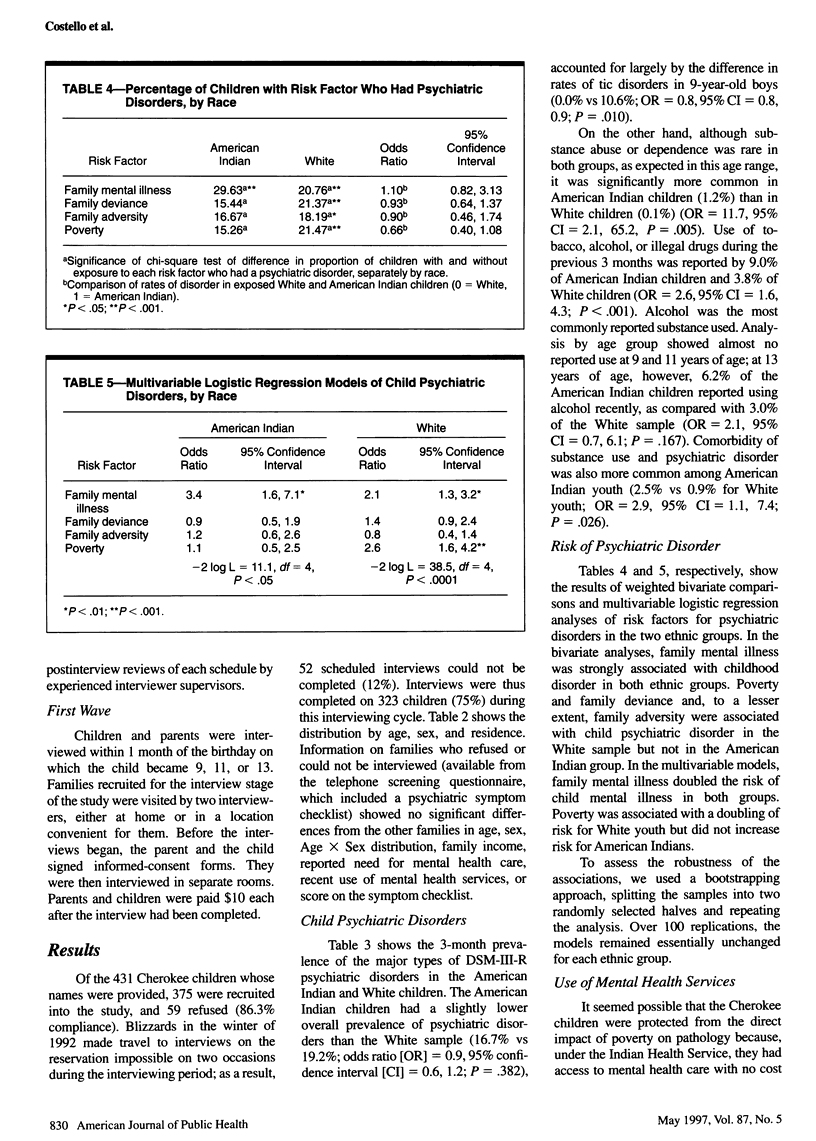
OBJECTIVES: This study examined prevalence of psychiatric disorders, social and family risk factors for disorders, and met and unmet needs for mental health care among Appalachian youth. METHODS: All 9-, 11-, and 13-year-old American Indian children in an 11-county area of the southern Appalachians were recruited, together with a representative sample of the surrounding population of White children. RESULTS: Three-month prevalences of psychiatric disorders were similar (American Indian, 16.7%; White, 19.2%). Substance use was more common in American Indian children (9.0% vs 3.8% in White children), as was comorbidity of substance use and psychiatric disorder (2.5% vs 0.9%). American Indian poverty, family adversity (e.g., parental unemployment, welfare dependency), and family deviance (parental violence, substance abuse, and crime) rates were higher, but the rate of family mental illness, excluding substance abuse, was lower. Child psychiatric disorder and mental health service use were associated with family mental illness in both ethnic groups but were associated with poverty and family deviance only in White children. Despite lower financial barriers, American Indian children used fewer mental health services. CONCLUSIONS: This study suggests that poverty and crime play different roles in different communities in the etiology of child psychiatric disorder.
Full text
PDF
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Angold A., Costello E. J. A test-retest reliability study of child-reported psychiatric symptoms and diagnoses using the Child and Adolescent Psychiatric Assessment (CAPA-C). Psychol Med. 1995 Jul;25(4):755–762. doi: 10.1017/s0033291700034991. [DOI] [PubMed] [Google Scholar]
- Angold A., Prendergast M., Cox A., Harrington R., Simonoff E., Rutter M. The Child and Adolescent Psychiatric Assessment (CAPA). Psychol Med. 1995 Jul;25(4):739–753. doi: 10.1017/s003329170003498x. [DOI] [PubMed] [Google Scholar]
- Burns B. J., Costello E. J., Angold A., Tweed D., Stangl D., Farmer E. M., Erkanli A. Children's mental health service use across service sectors. Health Aff (Millwood) 1995 Fall;14(3):147–159. doi: 10.1377/hlthaff.14.3.147. [DOI] [PubMed] [Google Scholar]
- Costello E. J., Angold A., Burns B. J., Erkanli A., Stangl D. K., Tweed D. L. The Great Smoky Mountains Study of Youth. Functional impairment and serious emotional disturbance. Arch Gen Psychiatry. 1996 Dec;53(12):1137–1143. doi: 10.1001/archpsyc.1996.01830120077013. [DOI] [PubMed] [Google Scholar]
- Costello E. J., Angold A., Burns B. J., Stangl D. K., Tweed D. L., Erkanli A., Worthman C. M. The Great Smoky Mountains Study of Youth. Goals, design, methods, and the prevalence of DSM-III-R disorders. Arch Gen Psychiatry. 1996 Dec;53(12):1129–1136. doi: 10.1001/archpsyc.1996.01830120067012. [DOI] [PubMed] [Google Scholar]
- Costello E. J. Developments in child psychiatric epidemiology. J Am Acad Child Adolesc Psychiatry. 1989 Nov;28(6):836–841. doi: 10.1097/00004583-198911000-00004. [DOI] [PubMed] [Google Scholar]
- Donnermeyer J. F., Park D. S. Alcohol use among rural adolescents: predictive and situational factors. Int J Addict. 1995 Mar;30(4):459–479. doi: 10.3109/10826089509048737. [DOI] [PubMed] [Google Scholar]
- Kelleher K. J., Rickert V. I., Hardin B. H., Pope S. K., Farmer F. L. Rurality and gender. Effects on early adolescent alcohol use. Am J Dis Child. 1992 Mar;146(3):317–322. doi: 10.1001/archpedi.1992.02160150057022. [DOI] [PubMed] [Google Scholar]
- Metzner H. L., Harburg E., Lamphiear D. E. Residential mobility and urban-rural residence within life stages related to health risk and chronic disease in Tecumseh, Michigan. J Chronic Dis. 1982;35(5):359–374. doi: 10.1016/0021-9681(82)90007-8. [DOI] [PubMed] [Google Scholar]
- Nelson S. H., McCoy G. F., Stetter M., Vanderwagen W. C. An overview of mental health services for American Indians and Alaska Natives in the 1990s. Hosp Community Psychiatry. 1992 Mar;43(3):257–261. doi: 10.1176/ps.43.3.257. [DOI] [PubMed] [Google Scholar]
- Oetting E. R., Swaim R. C., Edwards R. W., Beauvais F. Indian and Anglo adolescent alcohol use and emotional distress: path models. Am J Drug Alcohol Abuse. 1989;15(2):153–172. doi: 10.3109/00952998909092718. [DOI] [PubMed] [Google Scholar]
- Offord D. R., Boyle M. H., Szatmari P., Rae-Grant N. I., Links P. S., Cadman D. T., Byles J. A., Crawford J. W., Blum H. M., Byrne C. Ontario Child Health Study. II. Six-month prevalence of disorder and rates of service utilization. Arch Gen Psychiatry. 1987 Sep;44(9):832–836. doi: 10.1001/archpsyc.1987.01800210084013. [DOI] [PubMed] [Google Scholar]
- Rutter M., Cox A., Tupling C., Berger M., Yule W. Attainment and adjustment in two geographical areas. I--The prevalence of psychiatric disorder. Br J Psychiatry. 1975 Jun;126:493–509. doi: 10.1192/bjp.126.6.493. [DOI] [PubMed] [Google Scholar]
- SCHAIE K. W. A GENERAL MODEL FOR THE STUDY OF DEVELOPMENTAL PROBLEMS. Psychol Bull. 1965 Aug;64:92–107. doi: 10.1037/h0022371. [DOI] [PubMed] [Google Scholar]


