Abstract
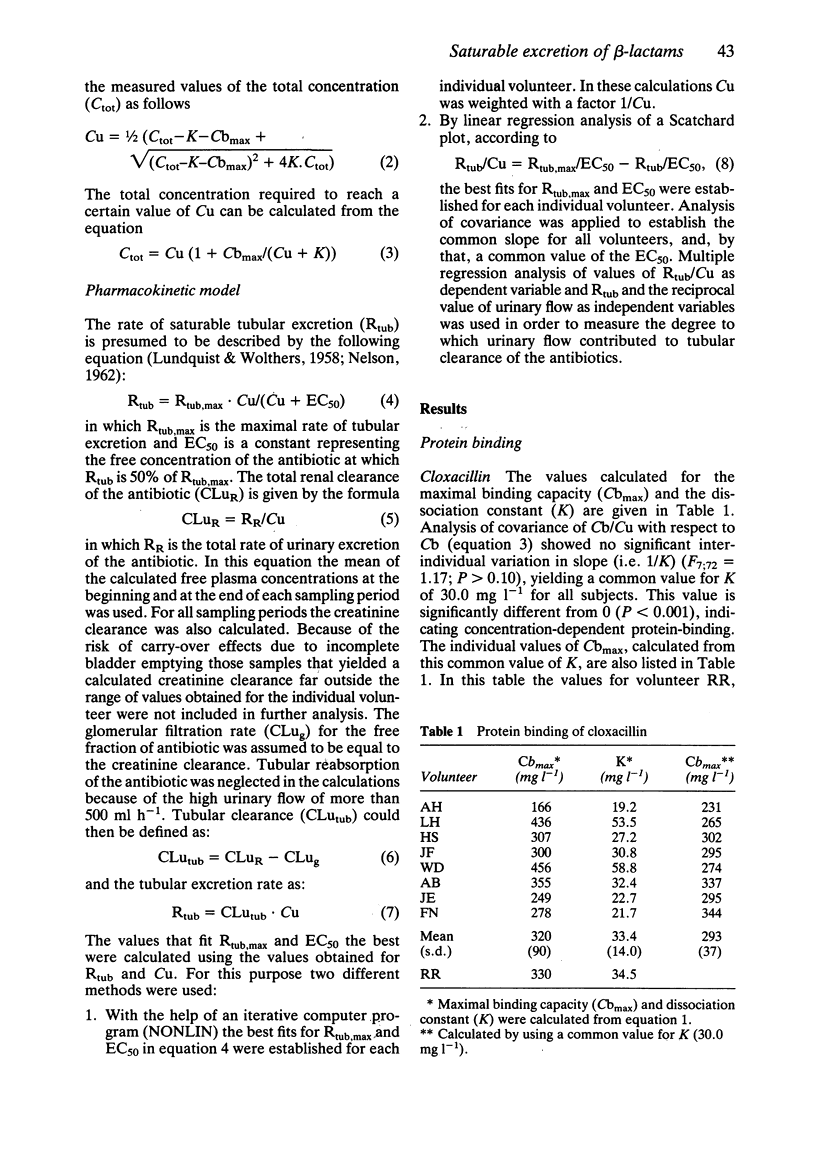
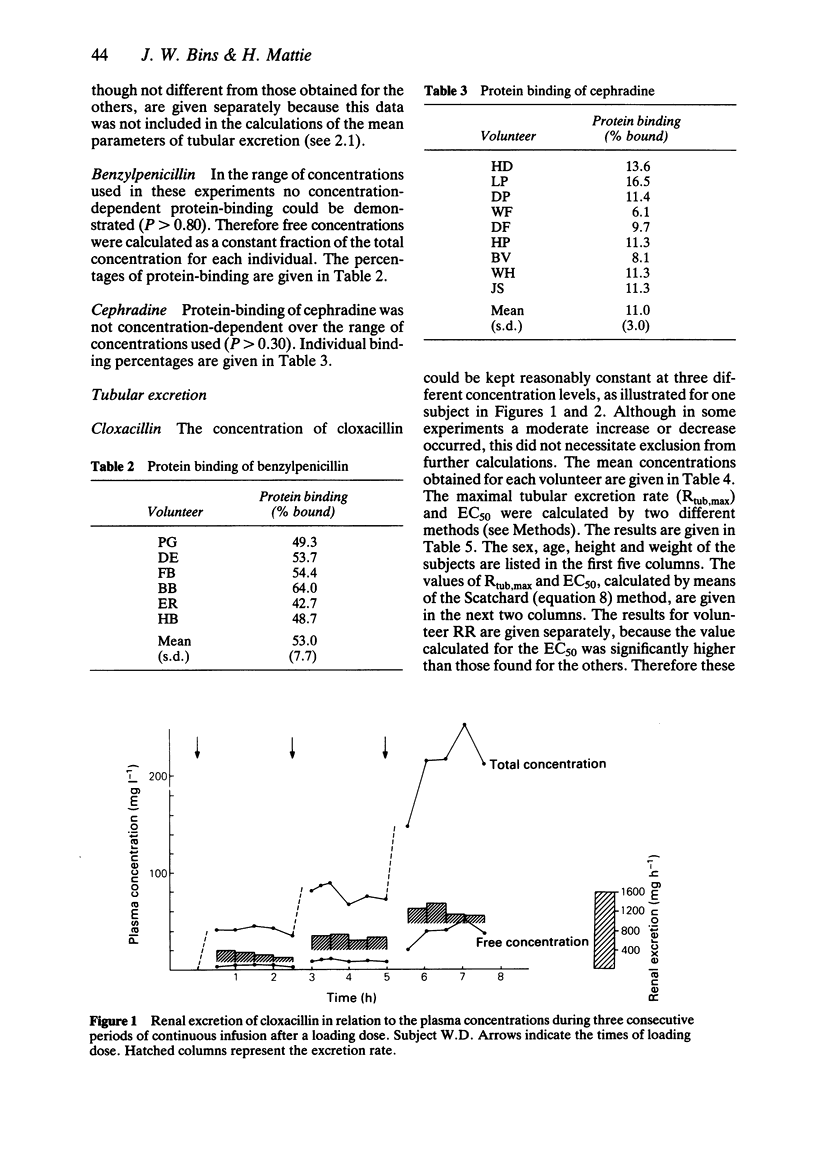
1 The saturability of the tubular excretion of cloxacillin, benzylpenicillin and cephradine was investigated. 2 Volunteers received a continuous infusion of one of the antibiotics at increasing infusion rates in order to maintain constant plasma concentrations at three different levels. Blood and urine samples were taken every 30 min. Sufficient urinary flow was ensured by a saline infusion (500 ml h-1). 3 Renal clearance of the antibiotic was calculated for the non-protein bound fraction of the drug. 4 Tubular clearance and tubular excretion rate were estimated by using the renal clearance of the antibiotic minus the glomerular filtration rate; the latter was considered to be equal to creatinine clearance. 5 Data were fitted to a Scatchard transformation and, by nonlinear methods, to a Michaelis-Menten equation. 6 Parameters of saturability, i.e. EC50 and maximal tubular excretion rate, were established. The values found for EC50 were 7.7, 93.0 and 266 mg l-1 for cloxacillin, benzylpenicillin and cephradine, respectively. The values calculated for the maximal tubular excretion rate were 1017, 5535 and 4537 mg h-1, respectively.
Full text
PDF

Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Appel G. B., Neu H. C. The nephrotoxicity of antimicrobial agents (second of three parts). N Engl J Med. 1977 Mar 31;296(13):722–728. doi: 10.1056/NEJM197703312961305. [DOI] [PubMed] [Google Scholar]
- Arvidsson A., Borgå O., Alván G. Renal excretion of cephapirin and cephaloridine: evidence for saturable tubular reabsorption. Clin Pharmacol Ther. 1979 Jun;25(6):870–876. doi: 10.1002/cpt1979256870. [DOI] [PubMed] [Google Scholar]
- Barza M., Melethil S., Berger S., Ernst E. C. Comparative pharmacokinetics of cefamandole, cephapirin, and cephalothin in healthy subjects and effect of repeated dosing. Antimicrob Agents Chemother. 1976 Sep;10(3):421–425. doi: 10.1128/aac.10.3.421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bergan T., Michalsen H. Pharmacokinetics of azlocillin in children with cystic fibrosis. Arzneimittelforschung. 1979;29(12A):1955–1957. [PubMed] [Google Scholar]
- Bergan T. Pharmacokinetics of beta-lactam antibiotics. Scand J Infect Dis Suppl. 1984;42:83–98. [PubMed] [Google Scholar]
- Bronfenbrenner J., Favour C. B. INCREASING AND PROLONGING BLOOD PENICILLIN CONCENTRATIONS FOLLOWING INTRAMUSCULAR ADMINISTRATION. Science. 1945 Jun 29;101(2635):673–674. doi: 10.1126/science.101.2635.673. [DOI] [PubMed] [Google Scholar]
- Eagle H., Newman E., Musselman A. D., Robinson M., Birmingham M. THE RENAL CLEARANCE OF PENICILLINS F, G, K, AND X IN RABBITS AND MAN. J Clin Invest. 1947 Sep;26(5):903–918. doi: 10.1172/JCI101885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fong I. W., Ralph E. D., Engelking E. R., Kirby W. M. Clinical pharmacology of cefamandole as compared with cephalothin. Antimicrob Agents Chemother. 1976 Jan;9(1):65–69. doi: 10.1128/aac.9.1.65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- HITZENBERGER G., SPITZY K. H. PHARMAKOKINETIK VON PENICILLIN-G BEI KONVENTIONELLER UND EXTREM HOHER DOSIERUNG. Arzneimittelforschung. 1964 Jan;14:19–23. [PubMed] [Google Scholar]
- LUNDQUIST F., WOLTHERS H. The kinetics of alcohol elimination in man. Acta Pharmacol Toxicol (Copenh) 1958;14(3):265–289. doi: 10.1111/j.1600-0773.1958.tb01164.x. [DOI] [PubMed] [Google Scholar]
- Mattie H., Goslings W. R., Noach E. L. Cloxacillin and nafcillin: serum binding and its relationship to antibacterial effect in mice. J Infect Dis. 1973 Aug;128(2):170–177. doi: 10.1093/infdis/128.2.170. [DOI] [PubMed] [Google Scholar]
- NELSON E. Zero order oxidation of tolbutamide in vivo. Nature. 1962 Jan 6;193:76–77. doi: 10.1038/193076b0. [DOI] [PubMed] [Google Scholar]
- Nauta E. H., Mattie H. Dicloxacillin and cloxacillin: pharmacokinetics in healthy and hemodialysis subjects. Clin Pharmacol Ther. 1976 Jul;20(1):98–108. doi: 10.1002/cpt197620198. [DOI] [PubMed] [Google Scholar]
- Nightingale C. H., Greene D. S., Quintiliani R. Pharmacokinetics and clinical use of cephalosporin antibiotics. J Pharm Sci. 1975 Dec;64(12):1899–1926. doi: 10.1002/jps.2600641202. [DOI] [PubMed] [Google Scholar]
- PERS M. Penicillin clearance as kidney function test, determinations with and without collection of urine. Scand J Clin Lab Invest. 1954;6(4):341–348. doi: 10.3109/00365515409134873. [DOI] [PubMed] [Google Scholar]
- Rammelkamp C. H., Keefer C. S. THE ABSORPTION, EXCRETION, AND DISTRIBUTION OF PENICILLIN. J Clin Invest. 1943 May;22(3):425–437. doi: 10.1172/JCI101412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rantz L. A., Kirby W. M., Randall E. THE ABSORPTION AND EXCRETION OF PENICILLIN FOLLOWING CONTINUOUS INTRAVENOUS AND SUBCUTANEOUS ADMINISTRATION. J Clin Invest. 1944 Sep;23(5):789–794. doi: 10.1172/JCI101552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simon C., Vock J., Malerczyk V. Zur Blutspiegelkinetik bei hochdosierter parenteraler Penicillin-G-Therapie. Dtsch Med Wochenschr. 1971 Aug 27;96(35):1393–1398. doi: 10.1055/s-0028-1110149. [DOI] [PubMed] [Google Scholar]
- Tjandramaga T. B., Mullie A., Verbesselt R., De Schepper P. J., Verbist L. Piperacillin: human pharmacokinetics after intravenous and intramuscular administration. Antimicrob Agents Chemother. 1978 Dec;14(6):829–837. doi: 10.1128/aac.14.6.829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tune B. M., Wu K. Y., Longerbeam D. F., Kempson R. L. Transport and toxicity of cephaloridine in the kidney. Effect of furosemide, p-aminohippurate and saline diuresis. J Pharmacol Exp Ther. 1977 Aug;202(2):472–478. [PubMed] [Google Scholar]


