Abstract
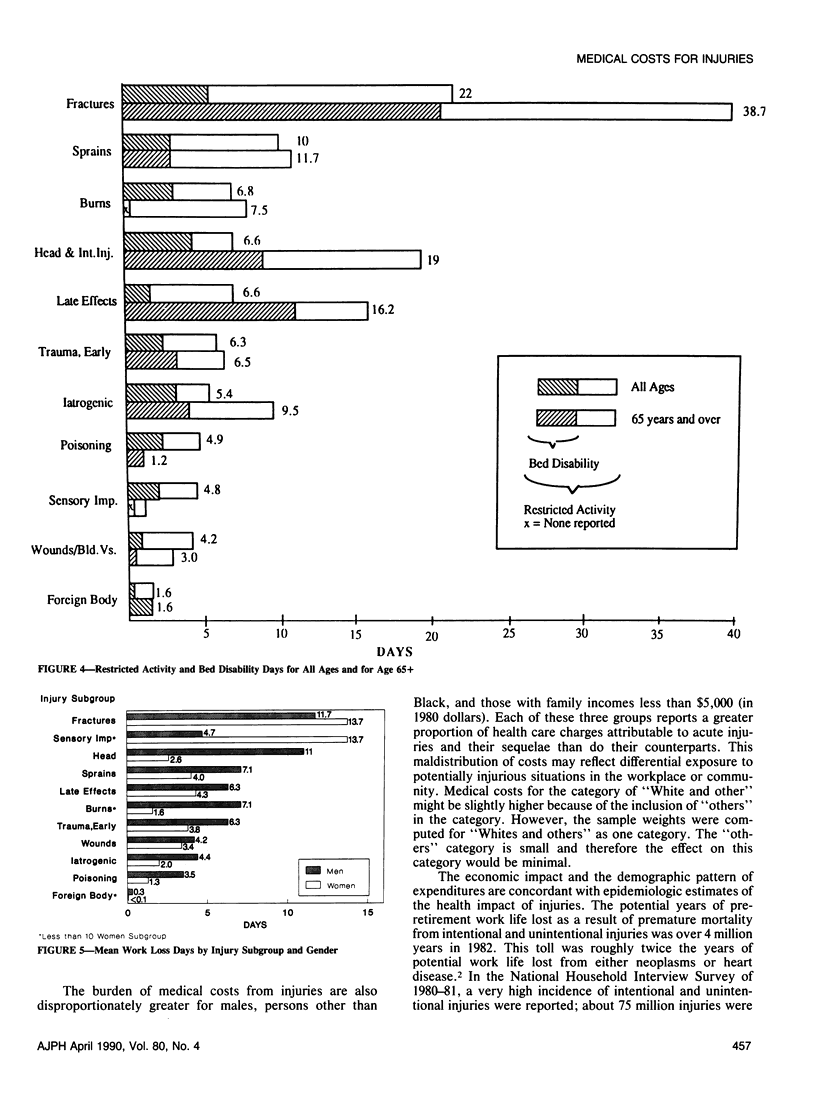
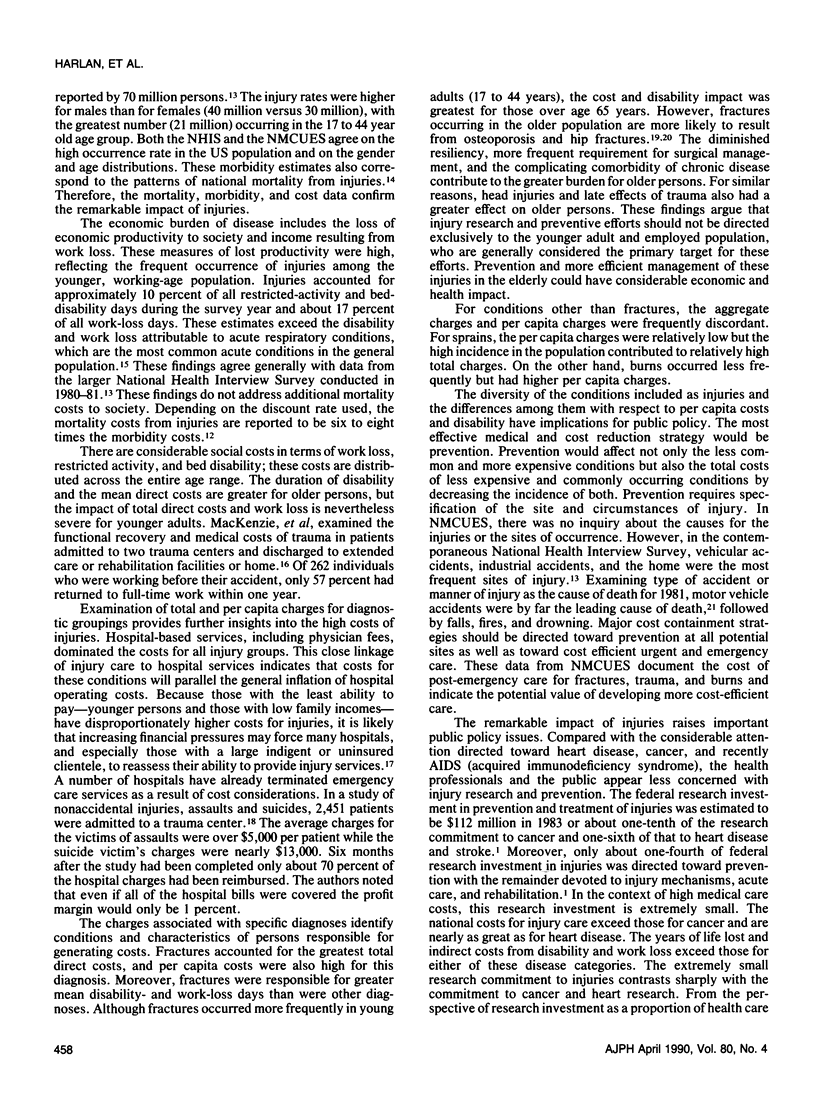
Data from the 1980 National Medical Care Utilization and Expenditure Survey were analyzed to place the costs for injuries in the context of all medical costs and to describe the distribution by demographic and diagnostic groups. For the non-institutionalized population, injuries, which include intentional and unintentional, were the second leading cause of direct medical costs, accounting for $16,745 million in medical care expenditures and a major contributor to work loss and disability in the US. For the working-age population (17-64 years) injuries were the leading cost category ($11,341 million) and the third most costly category for persons 65 years of age and over ($3,479 million). The preponderance of costs were attributable to hospital-based care. Direct medical costs were disproportionately greater for males, White and other persons, and for those with household incomes less than $5,000. Injury morbidity also accounts for major indirect costs. Fractures accounted for the highest direct medical costs, greatest per capita charges (based on those with charges), and largest number of restricted activity days. These national estimates document the economic importance of injuries and direct public attention to policy imperatives related to research and prevention.
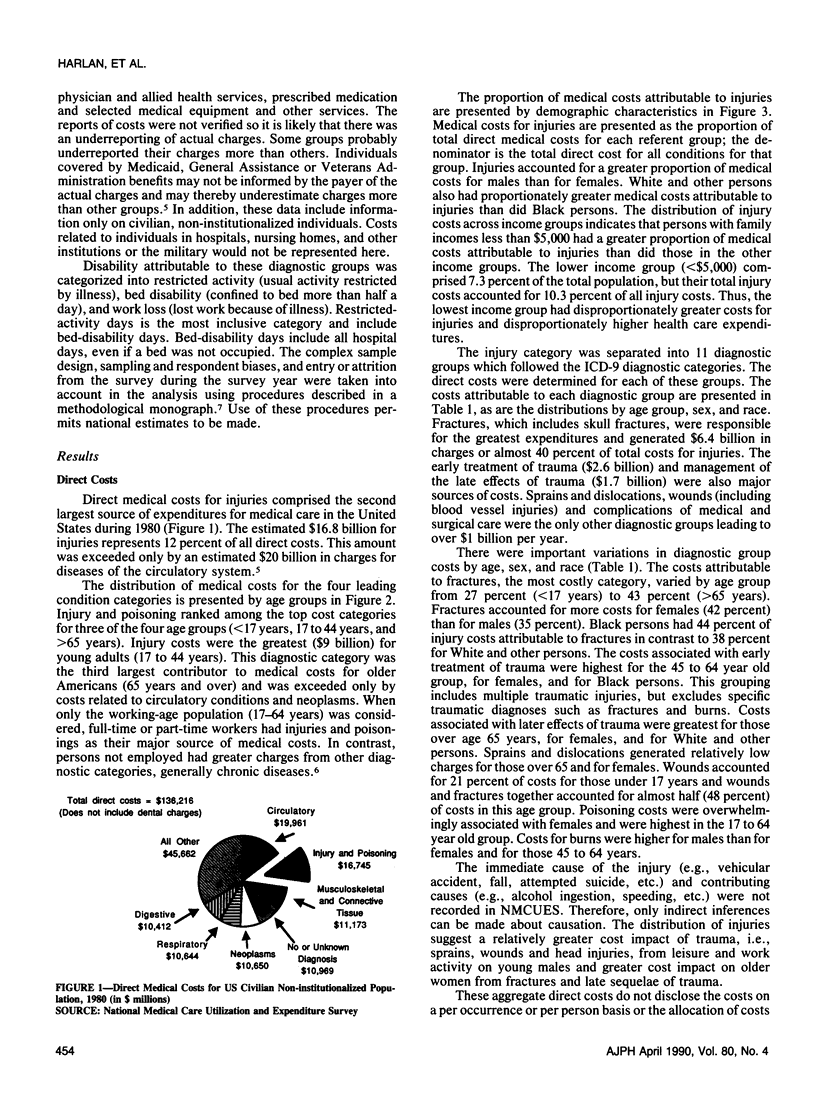
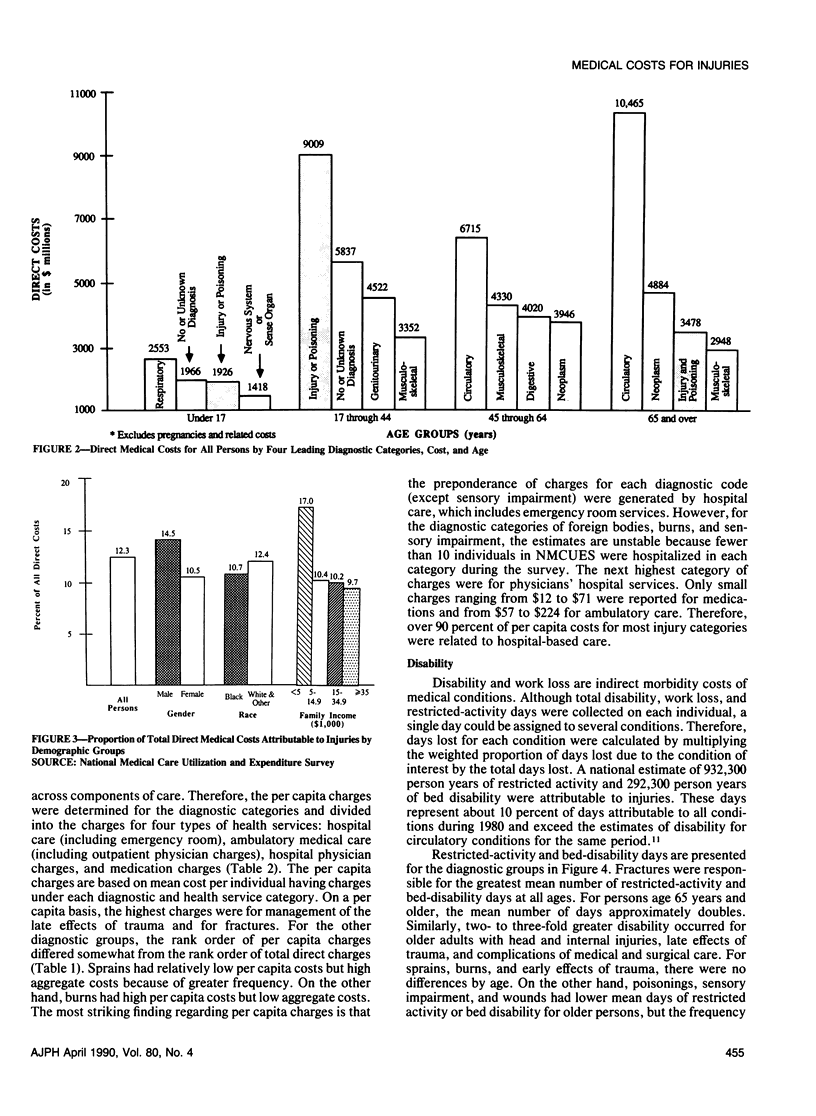
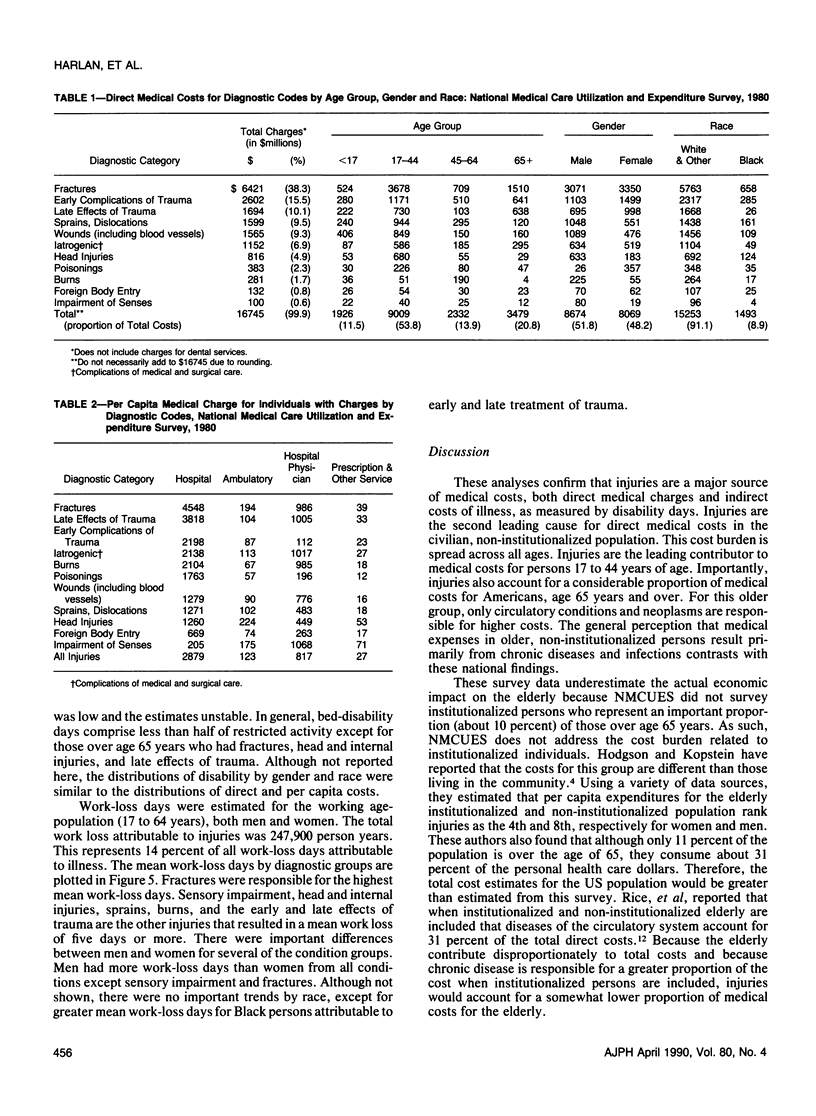
Full text
PDF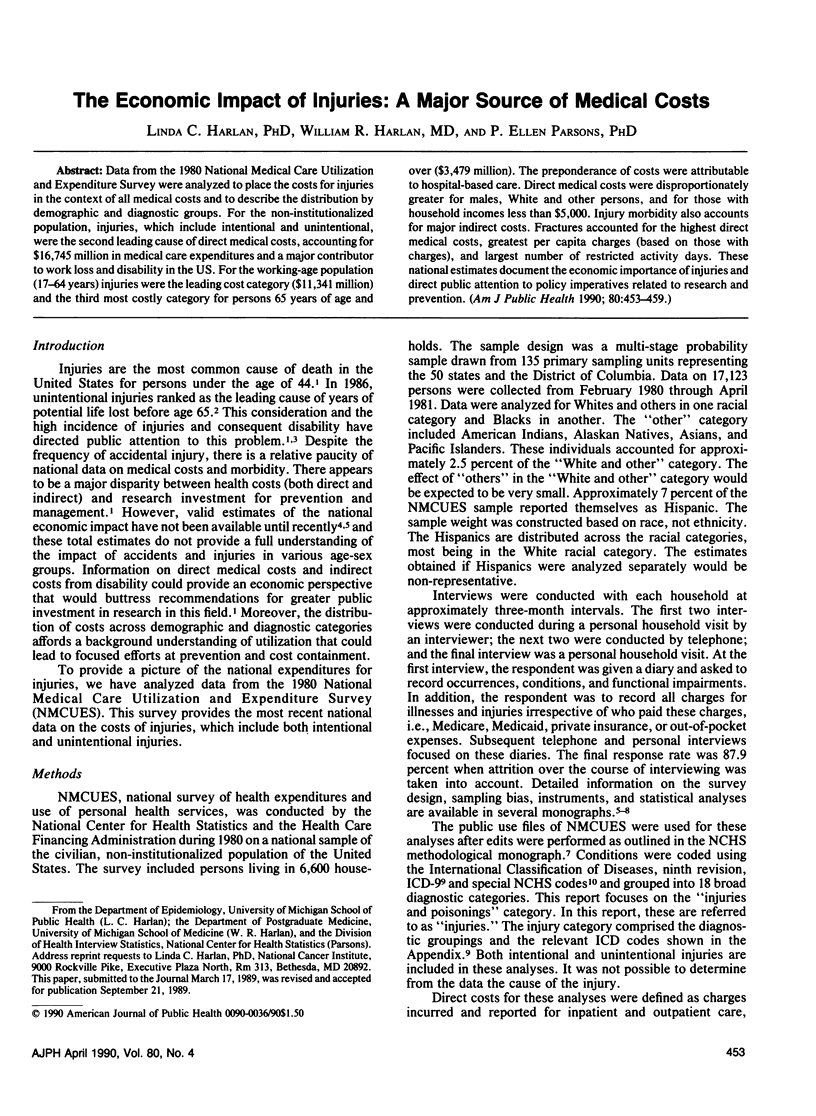
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Farmer M. E., White L. R., Brody J. A., Bailey K. R. Race and sex differences in hip fracture incidence. Am J Public Health. 1984 Dec;74(12):1374–1380. doi: 10.2105/ajph.74.12.1374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Foege W. H., Amler R. W., White C. C. Closing the gap. Report of the Carter Center Health Policy Consultation. JAMA. 1985 Sep 13;254(10):1355–1358. doi: 10.1001/jama.254.10.1355. [DOI] [PubMed] [Google Scholar]
- Gemmell M. K., Houk V. N. The possible dream: accident prevention and injury control--a conference to chart advances and plan strategy. Public Health Rep. 1985 Nov-Dec;100(6):557–559. [PMC free article] [PubMed] [Google Scholar]
- Luna G. K., Kendall K., Pilcher S., Copass M., Herman C. The medical and social impact of nonaccidental injury. Arch Surg. 1988 Jul;123(7):825–827. doi: 10.1001/archsurg.1988.01400310039006. [DOI] [PubMed] [Google Scholar]
- MacKenzie E. J., Siegel J. H., Shapiro S., Moody M., Smith R. T. Functional recovery and medical costs of trauma: an analysis by type and severity of injury. J Trauma. 1988 Mar;28(3):281–297. doi: 10.1097/00005373-198803000-00003. [DOI] [PubMed] [Google Scholar]
- Oakes D. D., Holcomb S. F., Sherck J. P. Patterns of trauma care costs and reimbursements: the burden of uninsured motorists. J Trauma. 1985 Aug;25(8):740–745. doi: 10.1097/00005373-198508000-00002. [DOI] [PubMed] [Google Scholar]
- Rice D. P., Hodgson T. A., Kopstein A. N. The economic costs of illness: a replication and update. Health Care Financ Rev. 1985 Fall;7(1):61–80. [PMC free article] [PubMed] [Google Scholar]


