Abstract
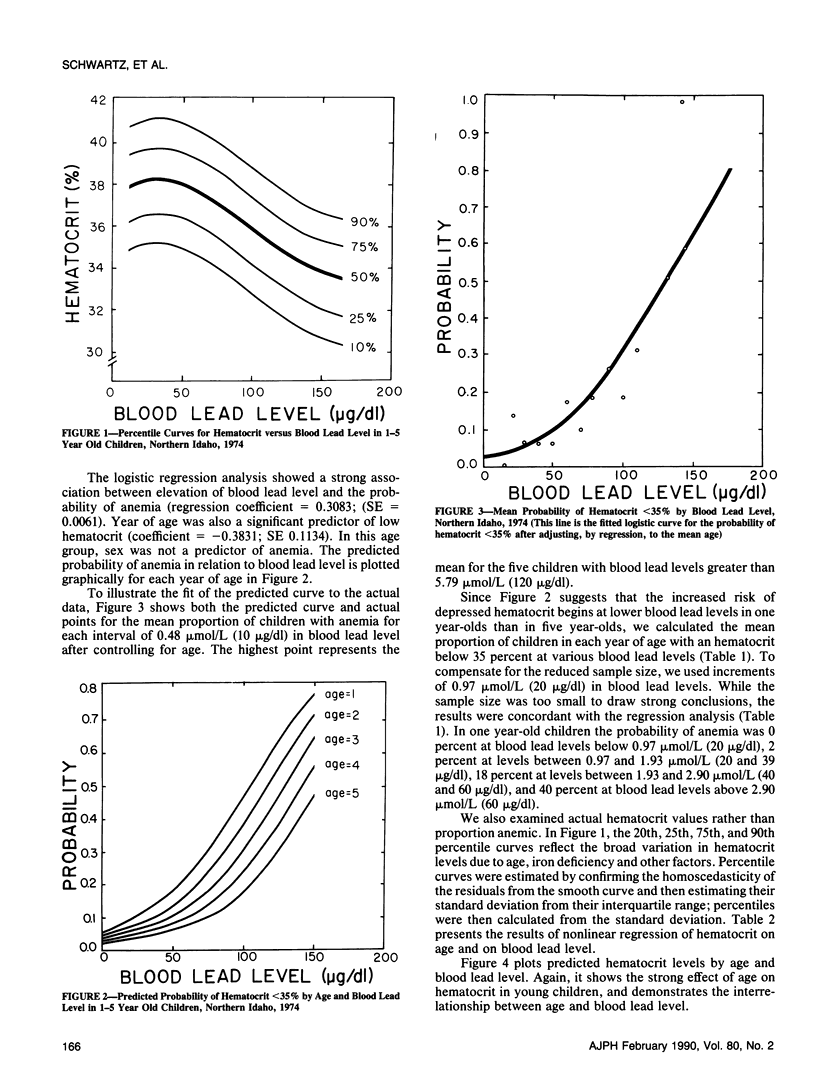
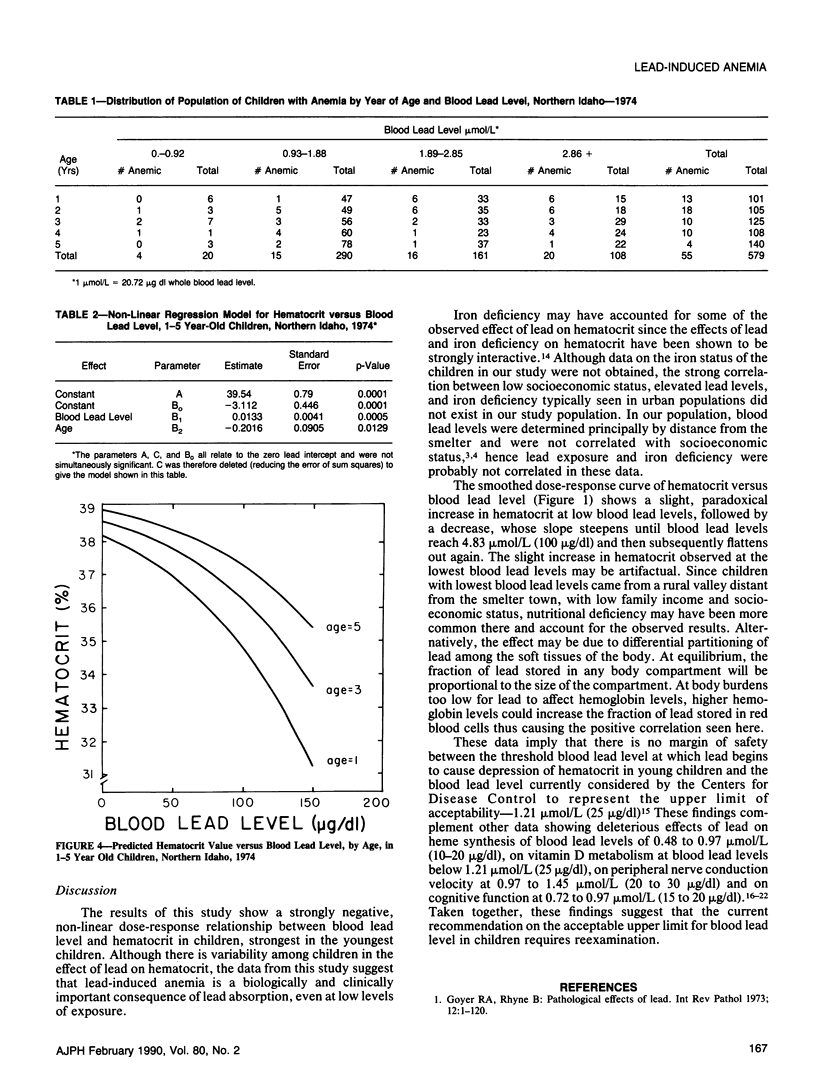
We conducted a cross-sectional epidemiologic study to assess the association between blood lead level and hematocrit in 579 one to five year-old children living near a primary lead smelter in 1974. Blood lead levels ranged from 0.53 to 7.91 mumol/L (11 to 164 micrograms/dl). To predict hematocrit as a function of blood lead level and age, we derived non-linear regression models and fit percentile curves. We used logistic regression to predict the probability of hematocrit values less than 35 per cent. We found a strong non-linear, dose-response relationship between blood lead level and hematocrit. This relationship was influenced by age, but (in this age group) not by sex; the effect was strongest in youngest children. In one year-olds, the age group most severely affected, the risk of an hematocrit value below 35 percent was 2 percent above background at blood lead levels between 0.97 and 1.88 mumol/L (20 and 39 micrograms/dl), 18 percent above background at lead levels of 1.93 to 2.85 mumol/L (40 to 59 micrograms/dl), and 40 percent above background at lead levels of 2.9 mumol/L (60 micrograms/dl) and greater; background was defined as a blood lead level below 1.88 mumol/L (20 micrograms/dl). This effect appeared independent of iron deficiency. These findings suggest that blood lead levels close to the currently recommended limit value of 1.21 mumol/L (25 micrograms/dl) are associated with dose-related depression of hematocrit in young children.
Full text
PDF

Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Adebonojo F. O. Hematologic status of urban black children in Philadelphia. Clin Pediatr (Phila) 1974 Oct;13(10):874-5, 880-3, 886-8. doi: 10.1177/000992287401301012. [DOI] [PubMed] [Google Scholar]
- Bellinger D., Leviton A., Waternaux C., Needleman H., Rabinowitz M. Longitudinal analyses of prenatal and postnatal lead exposure and early cognitive development. N Engl J Med. 1987 Apr 23;316(17):1037–1043. doi: 10.1056/NEJM198704233161701. [DOI] [PubMed] [Google Scholar]
- Goyer R. A., Rhyne B. C. Pathological effects of lead. Int Rev Exp Pathol. 1973;12:1–77. [PubMed] [Google Scholar]
- Granick S., Sassa S., Granick J. L., Levere R. D., Kappas A. Assays for porphyrins, delta-aminolevulinic-acid dehydratase, and porphyrinogen synthetase in microliter samples of whole blood: applications to metabolic defects involving the heme pathway. Proc Natl Acad Sci U S A. 1972 Sep;69(9):2381–2385. doi: 10.1073/pnas.69.9.2381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hernberg S., Nikkanen J., Mellin G., Lilius H. Delta-aminolevulinic acid dehydrase as a measure of lead exposure. Arch Environ Health. 1970 Aug;21(2):140–145. doi: 10.1080/00039896.1970.10667211. [DOI] [PubMed] [Google Scholar]
- Landrigan P. J., Baker E. L., Jr, Feldman R. G., Cox D. H., Eden K. V., Orenstein W. A., Mather J. A., Yankel A. J., Von Lindern I. H. Increased lead absorption with anemia and slowed nerve conduction in children near a lead smelter. J Pediatr. 1976 Dec;89(6):904–910. doi: 10.1016/s0022-3476(76)80594-x. [DOI] [PubMed] [Google Scholar]
- Marcus A. H., Schwartz J. Dose-response curves for erythrocyte protoporphyrin vs blood lead: effects of iron status. Environ Res. 1987 Dec;44(2):221–227. doi: 10.1016/s0013-9351(87)80230-x. [DOI] [PubMed] [Google Scholar]
- Piomelli S., Seaman C., Zullow D., Curran A., Davidow B. Threshold for lead damage to heme synthesis in urban children. Proc Natl Acad Sci U S A. 1982 May;79(10):3335–3339. doi: 10.1073/pnas.79.10.3335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schwartz J., Landrigan P. J., Feldman R. G., Silbergeld E. K., Baker E. L., Jr, von Lindern I. H. Threshold effect in lead-induced peripheral neuropathy. J Pediatr. 1988 Jan;112(1):12–17. doi: 10.1016/s0022-3476(88)80111-2. [DOI] [PubMed] [Google Scholar]
- Tola S., Hernberg S., Asp S., Nikkanen J. Parameters indicative of absorption and biological effect in new lead exposure: a prospective study. Br J Ind Med. 1973 Apr;30(2):134–141. doi: 10.1136/oem.30.2.134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yankel A. J., von Lindern I. H., Walter S. D. The Silver Valley lead study: the relationship between childhood blood lead levels and environmental exposure. J Air Pollut Control Assoc. 1977 Aug;27(8):763–767. doi: 10.1080/00022470.1977.10470488. [DOI] [PubMed] [Google Scholar]


