Abstract
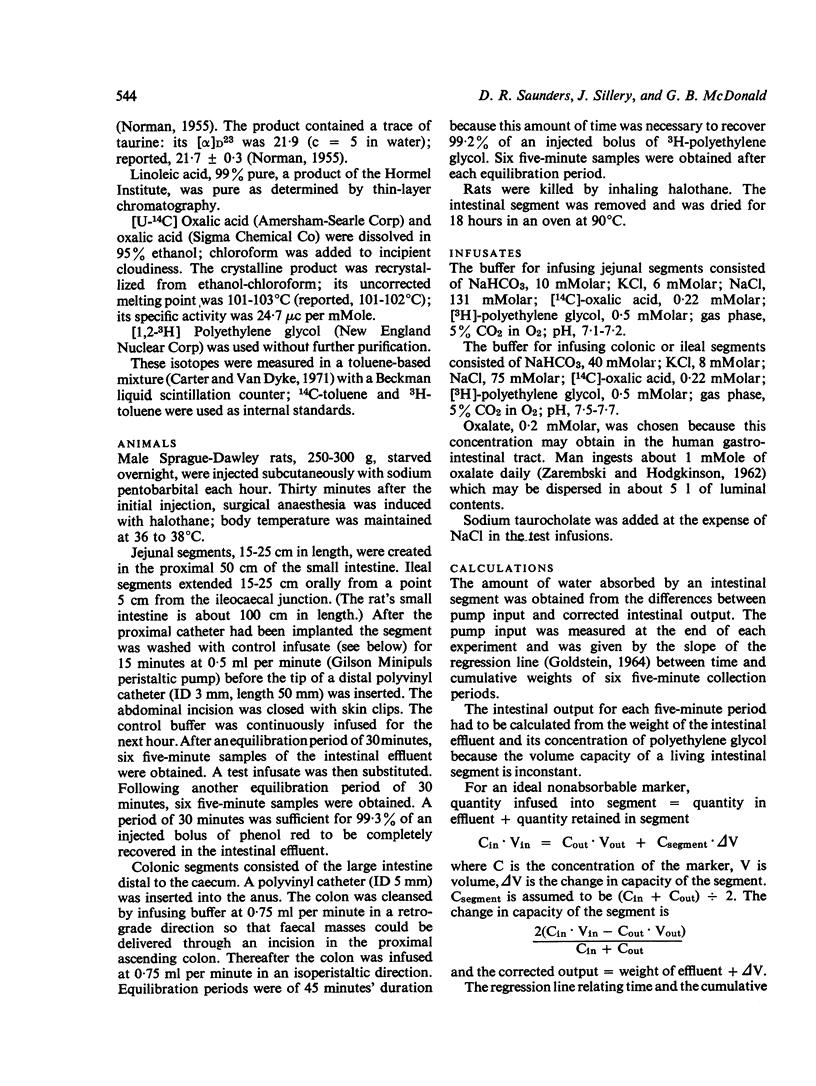
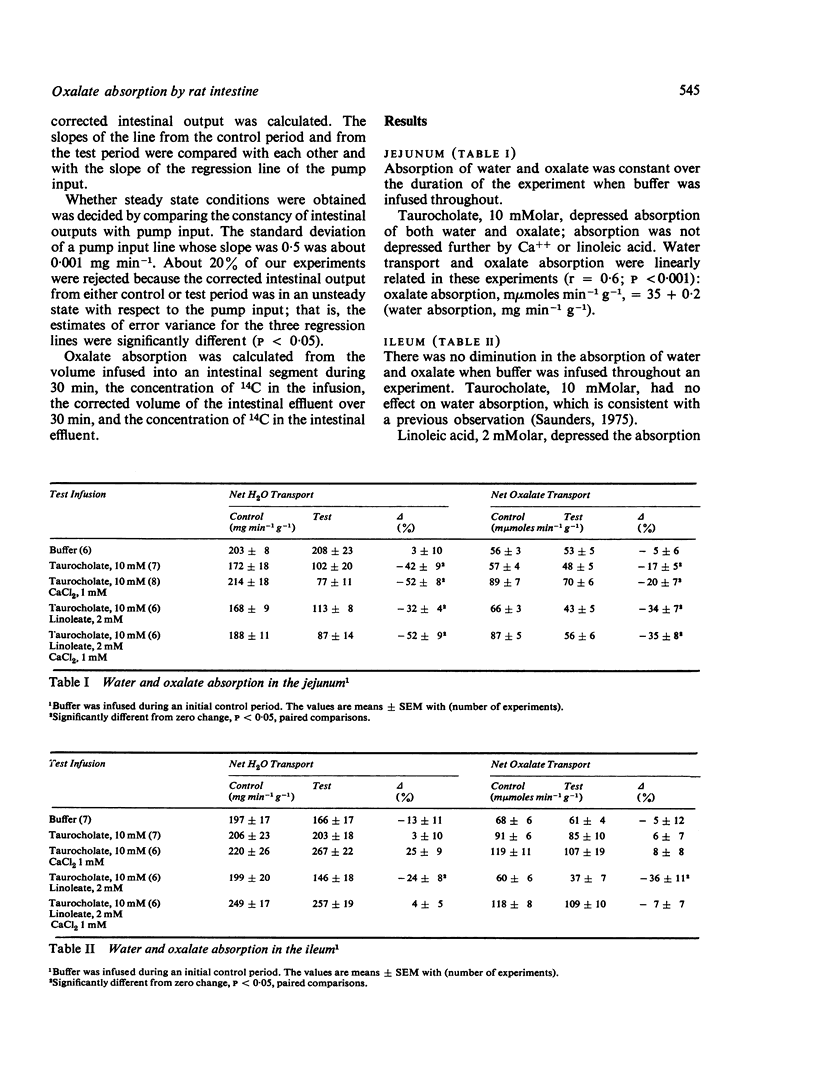
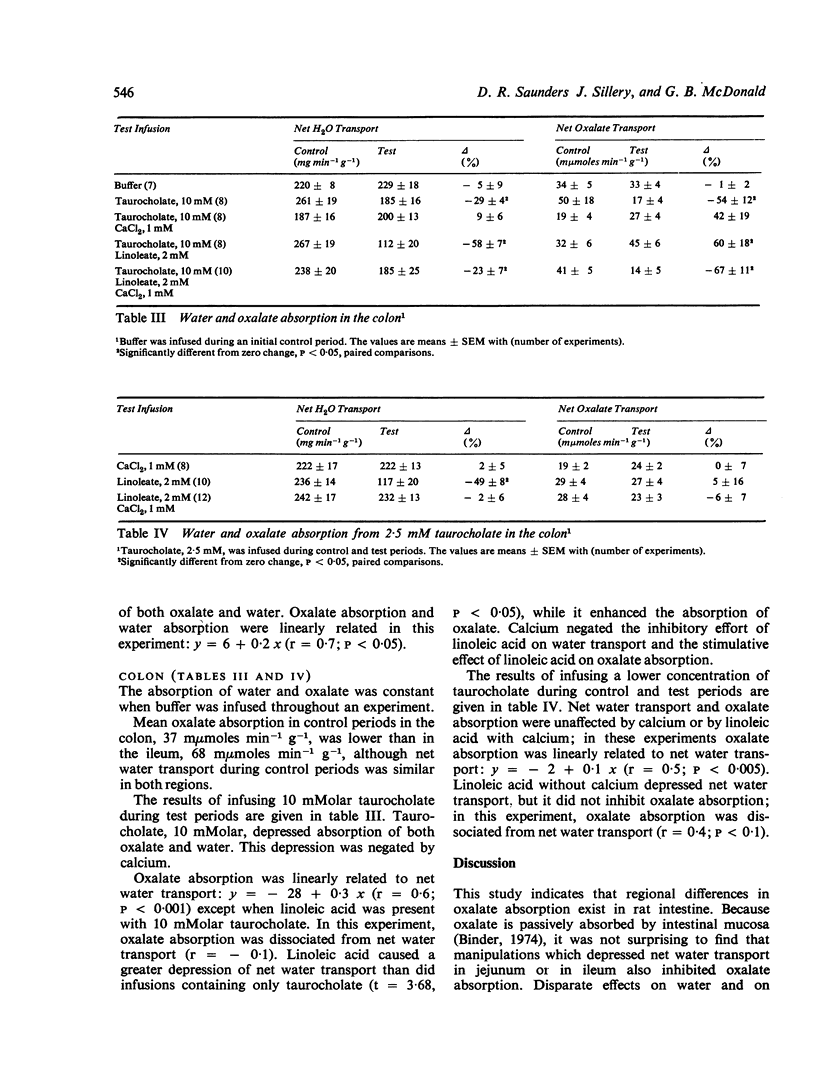
Clinical studies suggest that steatorrhoea can be associated with excessive absorption of dietary oxalate. We examined the influence of bile salts, Ca++, and long-chain fatty acid on the absorption of oxalate and water by rat intestine in vivo. Absorption was measured under steady-state conditions during single-pass infusions. Each intestinal segment served as its own control. In jejunum, 10 mM taurocholate, the principal salt in rat bile, depressed absorption of oxalate and water. Absorption was not depressed further by Ca++ or linoleic acid. In ileum, 10 mM taurocholate did not inhibit absorption. Linoleic acid, 2 mM, depressed absorption of both oxalate and water. In colon 10 mM taurocholate decreased absorption. Net water transport was depressed further when linoleic acid was added to the infusion, but oxalate absorption was enhanced. Ca++ negated these effects of linoleic acid. It is concluded that long-chain fatty acids may enhance the absorption of oxalate from the rat colon. This observation may be relevant to understanding hyperoxaluria in patients with steatorrhoea.
Full text
PDF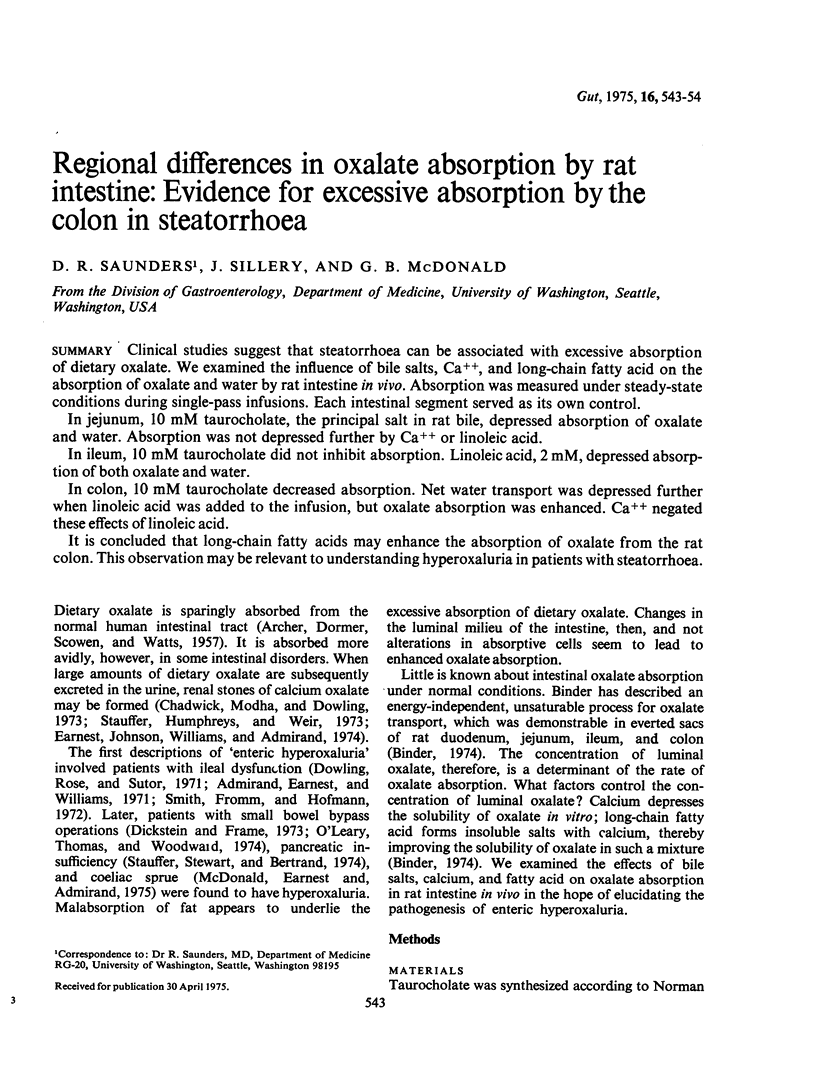
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- ARCHER H. E., DORMER A. E., SCOWEN E. F., WATTS R. W. Studies on the urinary excretion of oxalate by normal subjects. Clin Sci. 1957 Aug;16(3):405–411. [PubMed] [Google Scholar]
- Admirand W. H., Earnest D. L., Williams H. E. Hyperoxaluria and bowel disease. Trans Assoc Am Physicians. 1971;84:307–312. [PubMed] [Google Scholar]
- Ammon H. V., Phillips S. F. Inhibition of ileal water absorption by intraluminal fatty acids. Influence of chain length, hydroxylation, and conjugation of fatty acids. J Clin Invest. 1974 Jan;53(1):205–210. doi: 10.1172/JCI107539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Andersson H., Jagenburg R. Fat-reduced diet in the treatment of hyperoxaluria in patients with ileopathy. Gut. 1974 May;15(5):360–366. doi: 10.1136/gut.15.5.360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bennett R. C., Jepson R. P. Uric acid stone formation following ileostomy. Aust N Z J Surg. 1966 Nov;36(2):153–158. doi: 10.1111/j.1445-2197.1966.tb05509.x. [DOI] [PubMed] [Google Scholar]
- Binder H. J. Intestinal oxalate absorption. Gastroenterology. 1974 Sep;67(3):441–446. [PubMed] [Google Scholar]
- Bright-Asare P., Binder H. J. Stimulation of colonic secretion of water and electrolytes by hydroxy fatty acids. Gastroenterology. 1973 Jan;64(1):81–88. [PubMed] [Google Scholar]
- Carter G. W., Van Dyke K. A superior counting solution for water-soluble tritiated compounds. Clin Chem. 1971 Jul;17(7):576–580. [PubMed] [Google Scholar]
- Chadwick V. S., Modha K., Dowling R. H. Mechanism for hyperoxaluria in patients with ileal dysfunction. N Engl J Med. 1973 Jul 26;289(4):172–176. doi: 10.1056/NEJM197307262890402. [DOI] [PubMed] [Google Scholar]
- Dickstein S. S., Frame B. Urinary tract calculi after intestinal shunt operations for the treatment of obesity. Surg Gynecol Obstet. 1973 Feb;136(2):257–260. [PubMed] [Google Scholar]
- Dowling R. H., Rose G. A., Sutor D. J. Hyperoxaluria and renal calculi in ileal disease. Lancet. 1971 May 29;1(7709):1103–1106. doi: 10.1016/s0140-6736(71)91840-x. [DOI] [PubMed] [Google Scholar]
- Earnest D. L., Johnson G., Williams H. E., Admirand W. H. Hyperoxaluria in patients with ileal resection: an abnormality in dietary oxalate absorption. Gastroenterology. 1974 Jun;66(6):1114–1122. [PubMed] [Google Scholar]
- Findlay J. M., Eastwood M. A., Mitchell W. D. The physical state of bile acids in the diarrhoeal stool of ileal dysfunction. Gut. 1973 Apr;14(4):319–323. doi: 10.1136/gut.14.4.319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hofmann A. F., Poley J. R. Role of bile acid malabsorption in pathogenesis of diarrhea and steatorrhea in patients with ileal resection. I. Response to cholestyramine or replacement of dietary long chain triglyceride by medium chain triglyceride. Gastroenterology. 1972 May;62(5):918–934. [PubMed] [Google Scholar]
- Letter: Management of women with phenylketonuria. N Engl J Med. 1974 Jan 10;290(2):108–109. doi: 10.1056/NEJM197401102900217. [DOI] [PubMed] [Google Scholar]
- Marshall R. W., Cochran M., Hodgkinson A. Relationships between calcium and oxalic acid intake in the diet and their excretion in the urine of normal and renal-stone-forming subjects. Clin Sci. 1972 Jul;43(1):91–99. doi: 10.1042/cs0430091. [DOI] [PubMed] [Google Scholar]
- Mitchell W. D., Findlay J. M., Prescott R. J., Eastwood M. A., Horn D. B. Bile acids in the diarrhoea of ileal resection. Gut. 1973 May;14(5):348–353. doi: 10.1136/gut.14.5.348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- NORMAN A. FAECAL EXCRETION PRODUCTS OF CHOLIC ACID IN MAN. Br J Nutr. 1964;18:173–186. doi: 10.1079/bjn19640017. [DOI] [PubMed] [Google Scholar]
- O'Leary J. P., Thomas W. C., Jr, Woodward E. R. Urinary tract stone after small bowel bypass for morbid obesity. Am J Surg. 1974 Feb;127(2):142–147. doi: 10.1016/0002-9610(74)90150-0. [DOI] [PubMed] [Google Scholar]
- Saunders D. R., Hedges J. R., Sillery J., Esther L., Matsumura K., Rubin C. E. Morphological and functional effects of bile salts on rat colon. Gastroenterology. 1975 May;68(5 Pt 1):1236–1245. [PubMed] [Google Scholar]
- Smith L. H., Fromm H., Hofmann A. F. Acquired hyperoxaluria, nephrolithiasis, and intestinal disease. Description of a syndrome. N Engl J Med. 1972 Jun 29;286(26):1371–1375. doi: 10.1056/NEJM197206292862601. [DOI] [PubMed] [Google Scholar]
- Stauffer J. Q., Humphreys M. H., Weir G. J. Acquired hyperoxaluria with regional enteritis after ileal resection. Role of dietary oxalate. Ann Intern Med. 1973 Sep;79(3):383–391. doi: 10.7326/0003-4819-79-3-383. [DOI] [PubMed] [Google Scholar]
- ZAREMBSKI P. M., HODGKINSON A. The oxalic acid content of English diets. Br J Nutr. 1962;16:627–634. doi: 10.1079/bjn19620061. [DOI] [PubMed] [Google Scholar]
- Zarembski P. M., Hodgkinson A. Some factors influencing the urinary excretion of oxalic acid in man. Clin Chim Acta. 1969 Jul;25(1):1–10. doi: 10.1016/0009-8981(69)90218-6. [DOI] [PubMed] [Google Scholar]


