Abstract
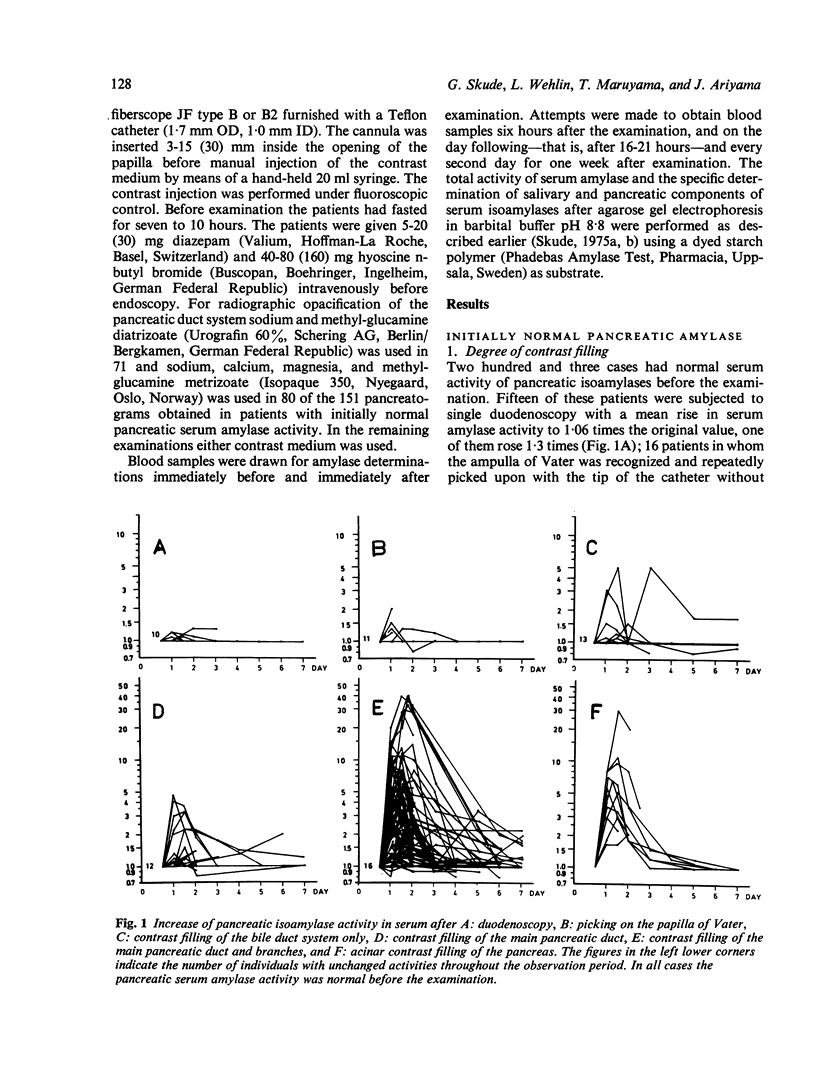
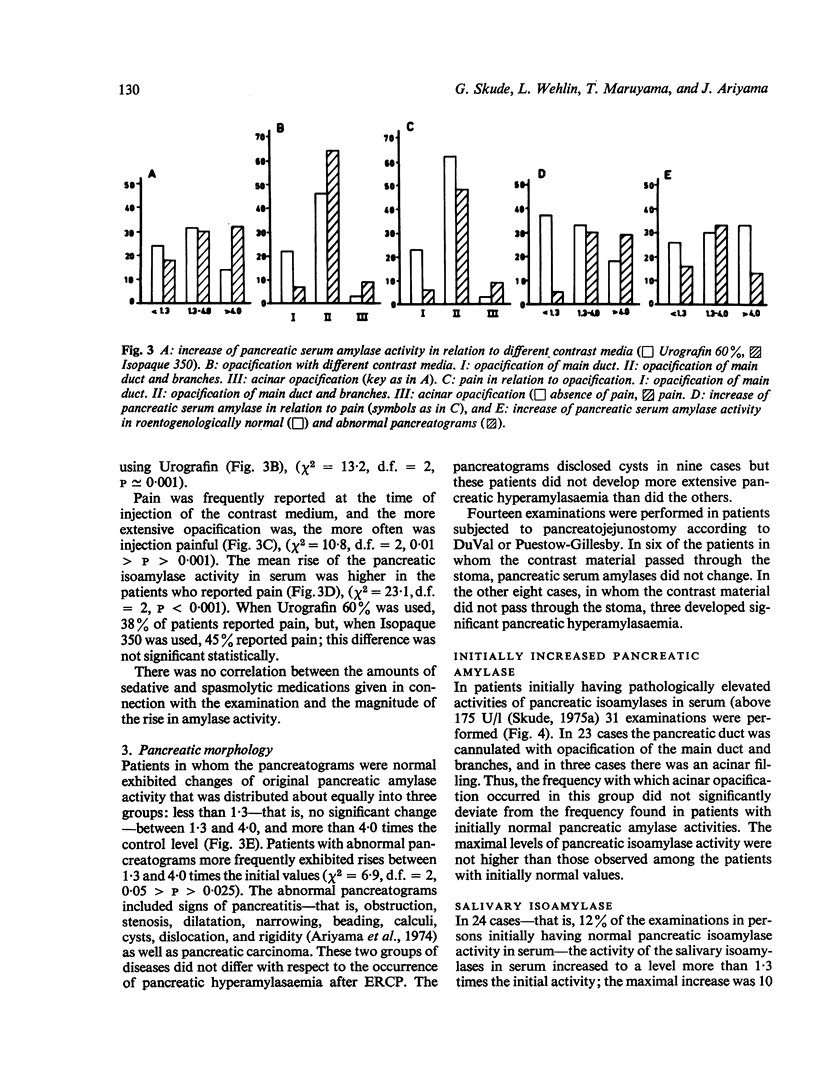
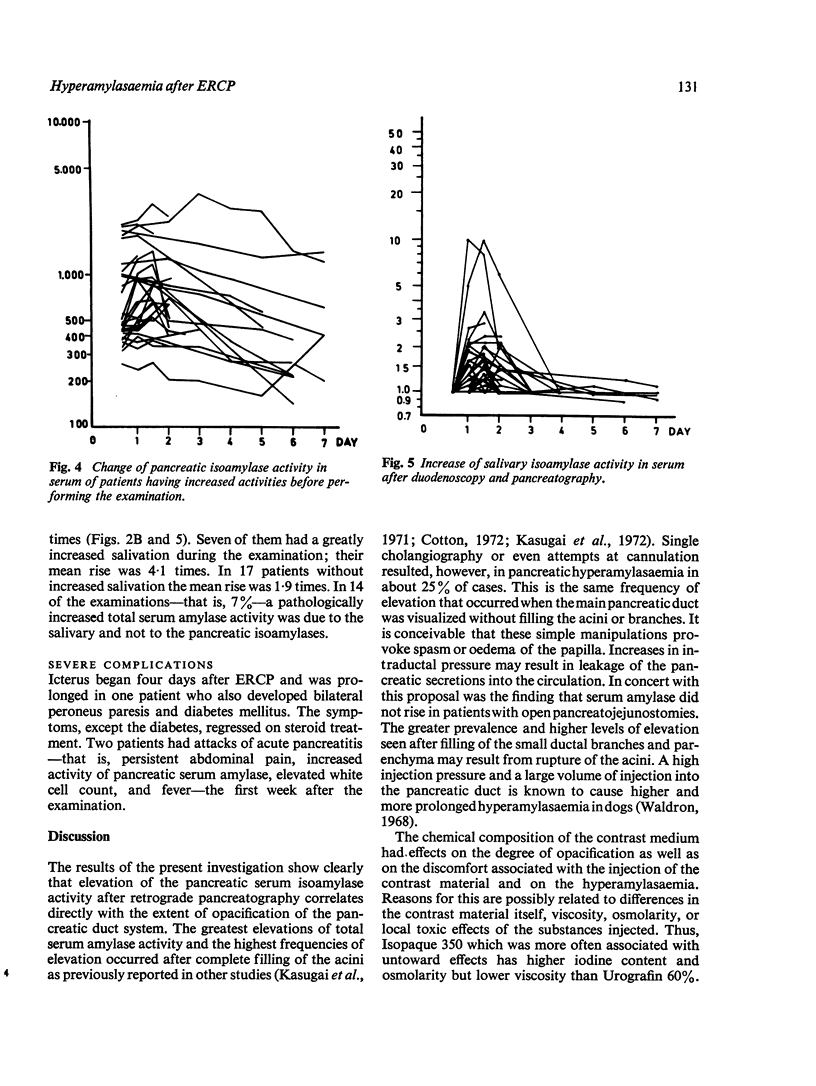
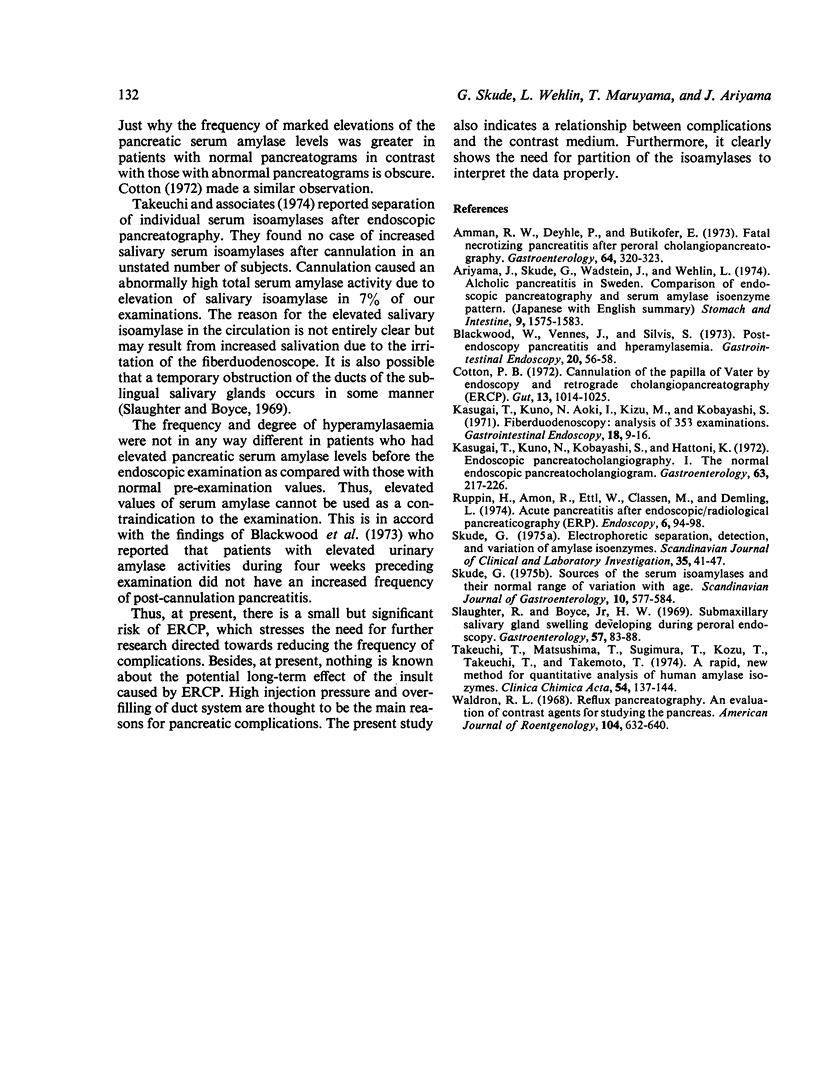
The salivary and pancreatic isoamylases of serum were determined separately in 234 cases of duodenoscopy and retrograde cholangiopancreatography. Successful pancreatic opacification was associated with pathologically high pancreatic serum amylase activities in 60% of the cases. Extensive opacification was associated with large increases of pancreatic serum isoamylases, the maximal rise recorded was 40 times the initial value. In spite of these striking chemical events only two patients developed clinical acute pancreatitis. There were some variations in pancreatic opacification and in the elevation of pancreatic serum amylase which seemed to depend upon the particular contrast material used. A rise of the salivary serum isoamylases caused pathologically high total serum amylase activities in 7% of the cases. High levels of pancreatic serum isoamylase activity before the time of examination did not result in any different pattern of hyperamylasaemia.
Full text
PDF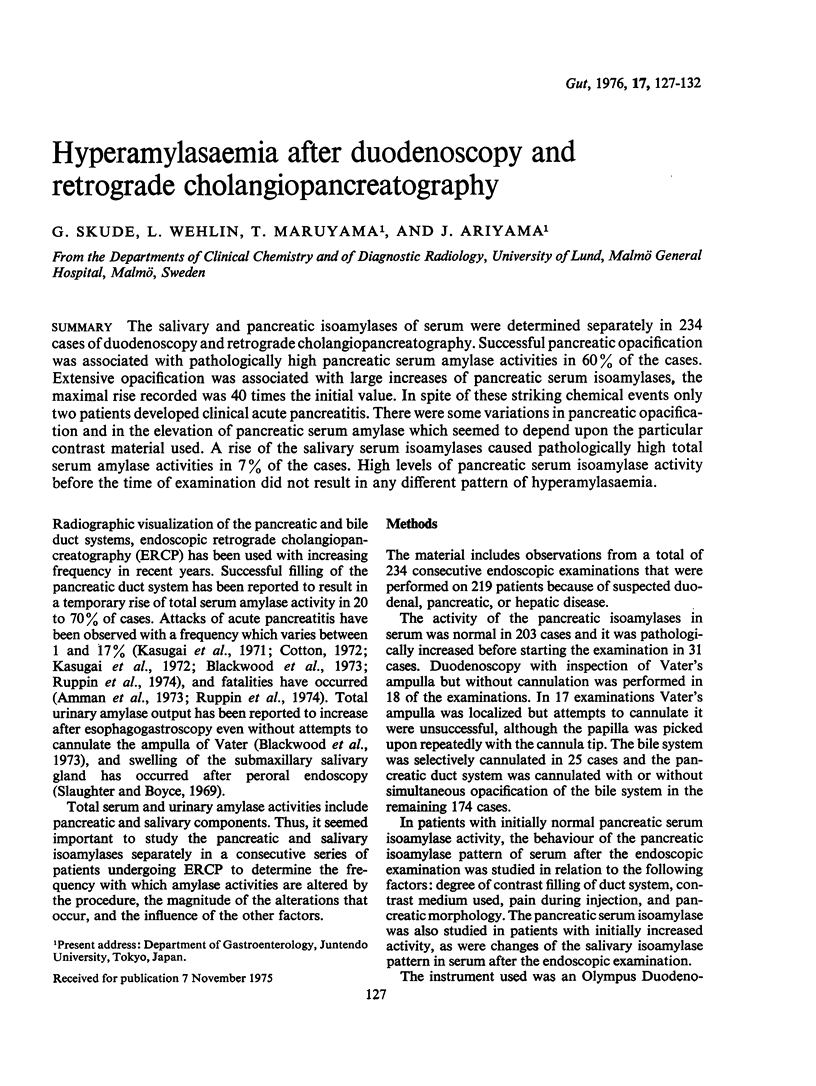
Images in this article
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Ammann R. W., Deyhle P., Butikofer E. Fatal nectotizing pancreatitis after peroral cholangiopancreatography. Gastroenterology. 1973 Feb;64(2):320–323. [PubMed] [Google Scholar]
- Blackwood W. D., Vennes J. A., Silvis S. E. Post-endoscopy pancreatitis and hyperamylasuria. Gastrointest Endosc. 1973 Nov;20(2):56–58. doi: 10.1016/s0016-5107(73)73873-6. [DOI] [PubMed] [Google Scholar]
- Cotton P. B. Cannulation of the papilla of Vater by endoscopy and retrograde cholangiopancreatography (ERCP). Gut. 1972 Dec;13(12):1014–1025. doi: 10.1136/gut.13.12.1014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kasugai T., Kuno N., Aoki I., Kizu M., Kobayashi S. Fiberduodenoscopy: analysis of 353 examinations. Gastrointest Endosc. 1971 Aug;18(1):9–16. doi: 10.1016/s0016-5107(71)74011-5. [DOI] [PubMed] [Google Scholar]
- Kasugai T., Kuno N., Kobayashi S., Hattori K. Endoscopic pancreatocholangiography. I. The normal endoscopic pancreatocholangiogram. Gastroenterology. 1972 Aug;63(2):217–226. [PubMed] [Google Scholar]
- Skude G. Electrophoretic separation, detection, and variation of amylase isoenzymes. Scand J Clin Lab Invest. 1975 Jan;35(1):41–47. doi: 10.1080/00365517509068003. [DOI] [PubMed] [Google Scholar]
- Skude G. Sources of the serum isoamylases and their normal range of variation with age. Scand J Gastroenterol. 1975;10(6):577–584. [PubMed] [Google Scholar]
- Slaughter R. L., Boyce H. W., Jr Submaxillary salivary gland swelling developing during peroral endoscopy. Gastroenterology. 1969 Jul;57(1):83–88. [PubMed] [Google Scholar]
- Takeuchi T., Matsushima T., Sugimura T., Kozu T., Takeuchi T. A rapid, new method for quantitative analysis of human amylase isozymes. Clin Chim Acta. 1974 Jul 31;54(2):137–144. doi: 10.1016/0009-8981(74)90231-9. [DOI] [PubMed] [Google Scholar]
- Waldron R. L., 2nd Reflux pancreatography. An evalauation of contrast agents for studying the pancreas. Am J Roentgenol Radium Ther Nucl Med. 1968 Nov;104(3):632–640. [PubMed] [Google Scholar]