Abstract
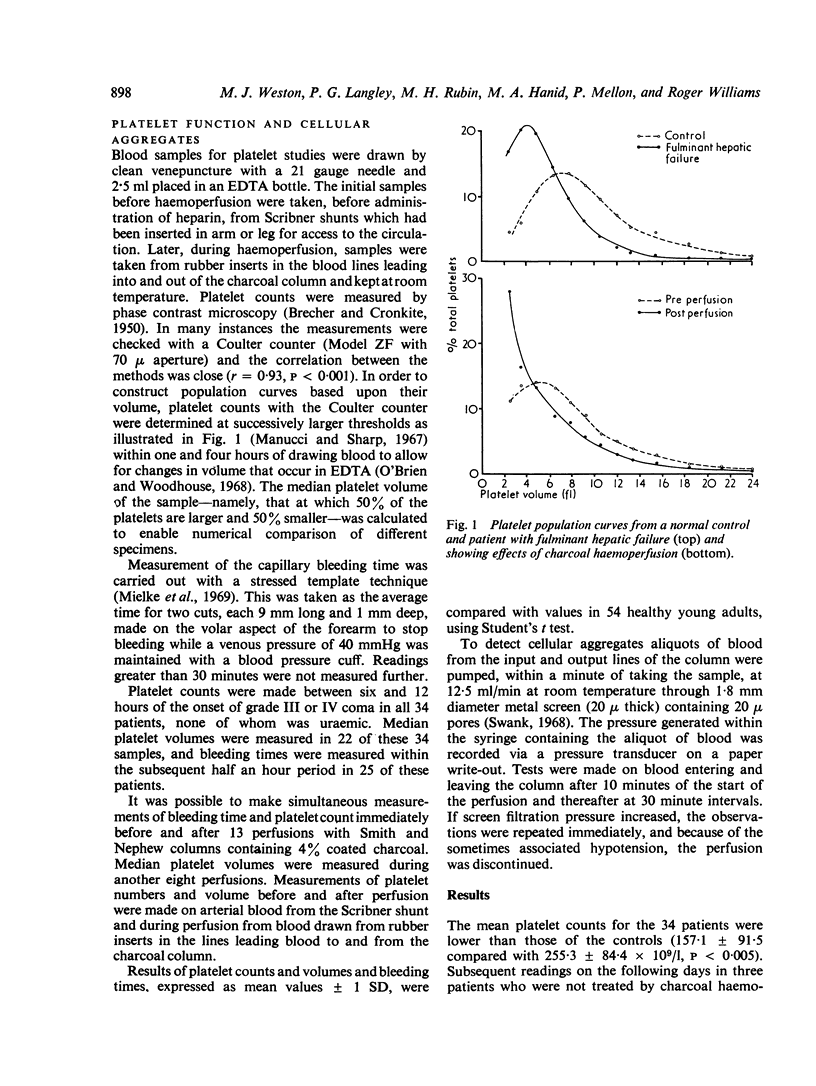
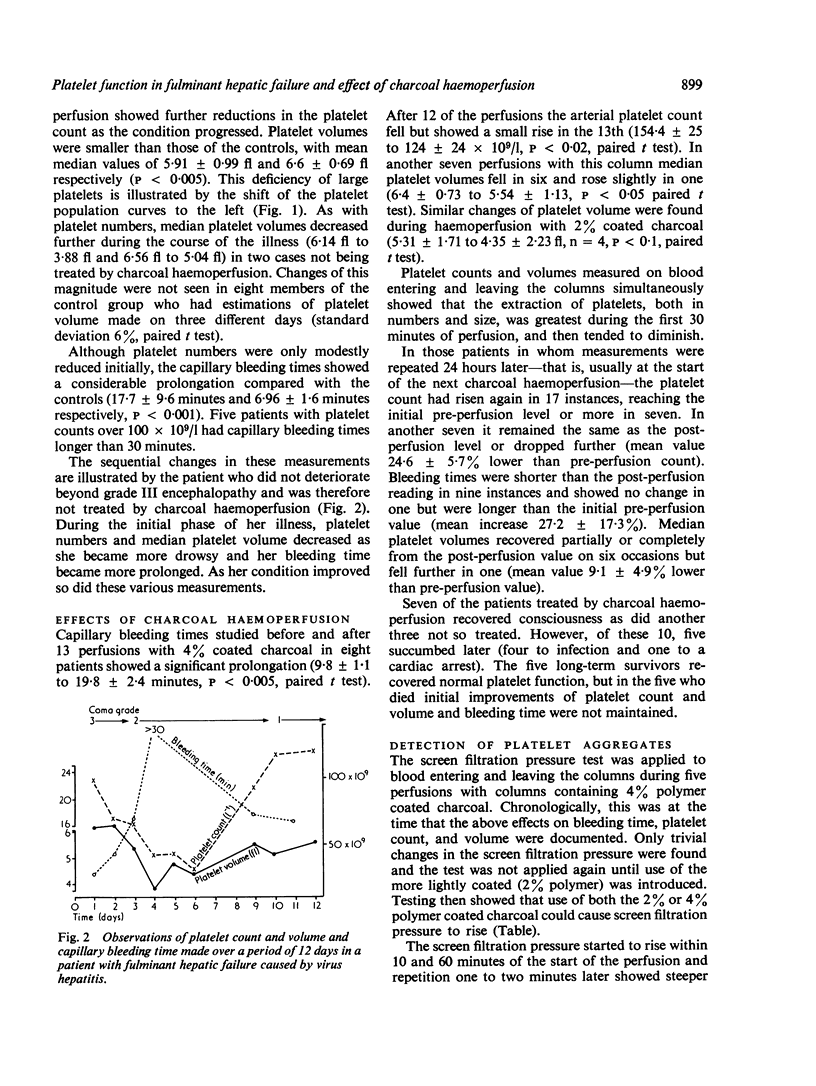
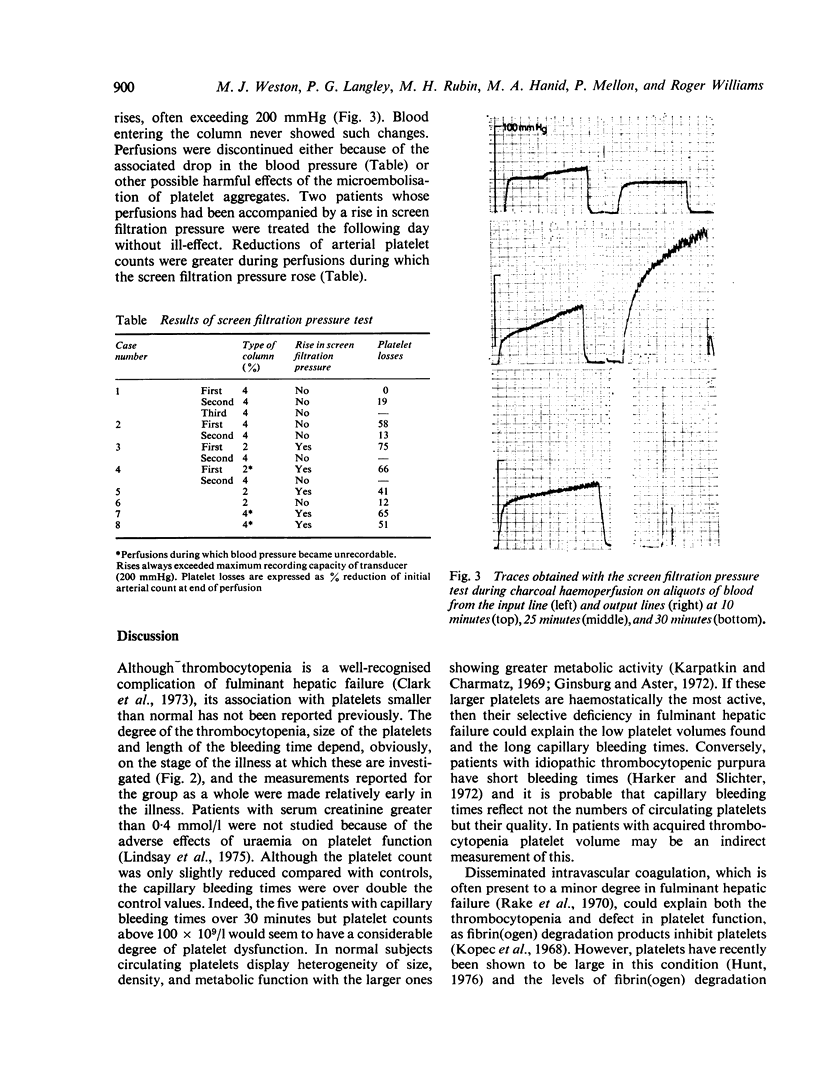
In 34 patients with fulminant hepatic failure, platelets, in addition to being reduced in numbers, were smaller than those of healthy controls. In keeping with this, capillary bleeding times were significantly longer than could be accounted for by reduction in numbers alone. In a small group of these patients use of charcoal haemoperfusion for temporary liver support produced a doubling of the capillary bleeding time despite only a small drop in arterial platelet counts. This disproportionate prolongation of bleeding time was almost certainly caused by the loss of larger platelets in the charcoal columns during perfusion, as the mean median volume also fell during perfusion. Rises in screen filtration pressure of blood leaving the columns were found during some perfusions and thought to be indicative of platelet aggregates. Release of vasoactive substances from platelets could account for the hypotension often found at this time.
Full text
PDF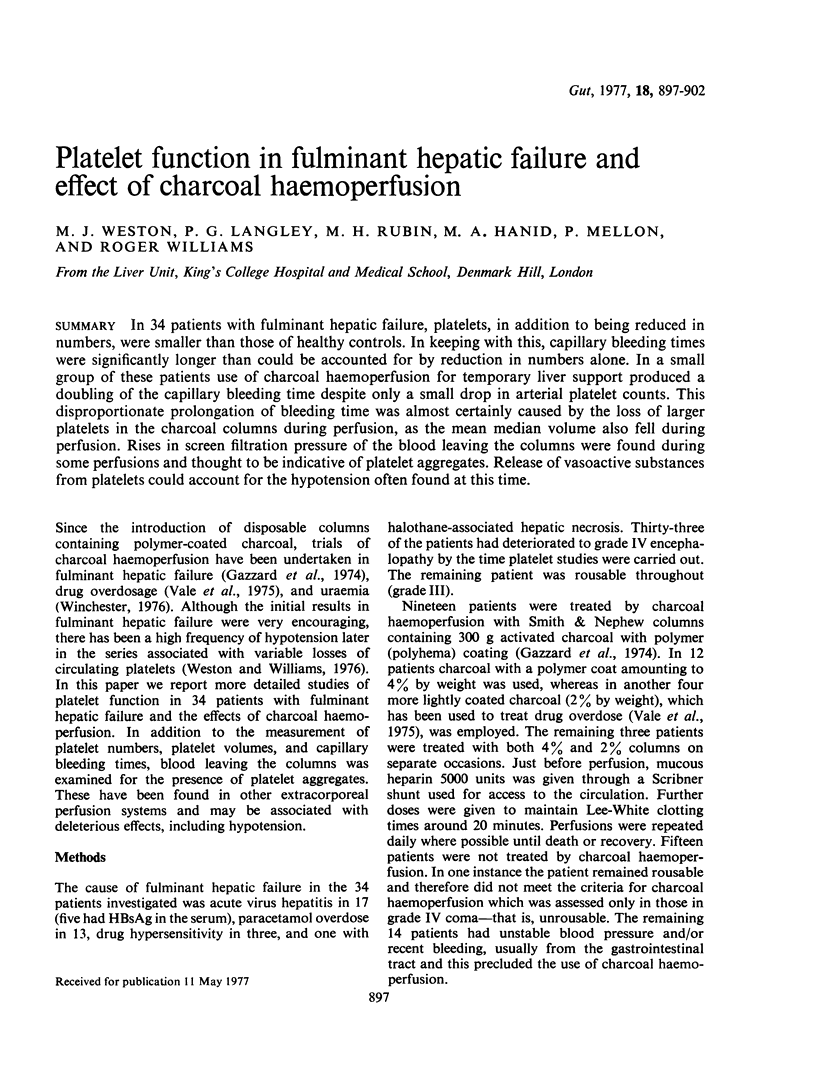

Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Allardyce D. B., Yoshida S. H., Ashmore P. G. The importance of microembolism in the pathogenesis of organ dysfunction caused by prolonged use of the pump oxygenator. J Thorac Cardiovasc Surg. 1966 Nov;52(5):706–715. [PubMed] [Google Scholar]
- BORCHGREVINK C. F. The mechanism of the prolonged bleeding time provoked by dextran sulphate or by excessive doses of heparin. Acta Med Scand. 1961 Sep;170:365–373. doi: 10.1111/j.0954-6820.1961.tb00249.x. [DOI] [PubMed] [Google Scholar]
- BRECHER G., CRONKITE E. P. Morphology and enumeration of human blood platelets. J Appl Physiol. 1950 Dec;3(6):365–377. doi: 10.1152/jappl.1950.3.6.365. [DOI] [PubMed] [Google Scholar]
- Clark R., Rake M. O., Flute P. T., Williams R. Coagulation abnormalities in acute liver failure; pathogenetic and therapeutic implications. Scand J Gastroenterol Suppl. 1973;19:63–70. [PubMed] [Google Scholar]
- Gazzard B. G., Weston M. J., Murray-Lyon I. M., Flax H., Record C. O., Williams R., Portmann B., Langley P. G., Dunlop E. H., Mellon P. J. Charcoal haemoperfusion in the treatment of fulminant hepatic failure. Lancet. 1974 Jun 29;1(7870):1301–1307. doi: 10.1016/s0140-6736(74)90678-3. [DOI] [PubMed] [Google Scholar]
- Ginsburg A. D., Aster R. H. Changes associated with platelet aging. Thromb Diath Haemorrh. 1972 Jul 31;27(3):407–415. [PubMed] [Google Scholar]
- Harker L. A., Slichter S. J. The bleeding time as a screening test for evaluation of platelet function. N Engl J Med. 1972 Jul 27;287(4):155–159. doi: 10.1056/NEJM197207272870401. [DOI] [PubMed] [Google Scholar]
- Hunt F. A. A rapid method for assessing megathrombocytes: its application to thrombocytotic and acquired thrombocytopenic states. Pathology. 1976 Jan;8(1):47–55. doi: 10.3109/00313027609094424. [DOI] [PubMed] [Google Scholar]
- Karpatkin S. Heterogeneity of human platelets. I. Metabolic and kinetic evidence suggestive of young and old platelets. J Clin Invest. 1969 Jun;48(6):1073–1082. doi: 10.1172/JCI106063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Laufer N., Merin G., Grover N. B., Pessachowicz B., Borman J. B. The influence of cardiopulmonary bypass on the size of human platelets. J Thorac Cardiovasc Surg. 1975 Oct;70(4):727–731. [PubMed] [Google Scholar]
- Lindsay R. M., Moorthy A. V., Koens F., Linton A. L. Platelet function in dialyzed and non-dialyzed patients with chronic renal failure. Clin Nephrol. 1975 Aug;4(2):52–57. [PubMed] [Google Scholar]
- Mannucci P. M., Sharp A. A. Platelet volume and shape in relation to aggregation and adhesion. Br J Haematol. 1967 Jul;13(4):604–617. doi: 10.1111/j.1365-2141.1967.tb00768.x. [DOI] [PubMed] [Google Scholar]
- McKenna R., Bachmann F., Whittaker B., Gilson J. R., Weinberg M. The hemostatic mechanism after open-heart surgery. II. Frequency of abnormal platelet functions during and after extracorporeal circulation. J Thorac Cardiovasc Surg. 1975 Aug;70(2):298–308. [PubMed] [Google Scholar]
- Mielke C. H., Jr, Kaneshiro M. M., Maher I. A., Weiner J. M., Rapaport S. I. The standardized normal Ivy bleeding time and its prolongation by aspirin. Blood. 1969 Aug;34(2):204–215. [PubMed] [Google Scholar]
- Rake M. O., Flute P. T., Pannell G., Williams R. Intravascular coagulation in acute hepatic necrosis. Lancet. 1970 Mar 14;1(7646):533–537. doi: 10.1016/s0140-6736(70)90767-1. [DOI] [PubMed] [Google Scholar]
- Siemensma N. P., Bathal P. S., Penington D. G. The effect of massive liver resection on platelet kinetics in the rat. J Lab Clin Med. 1975 Nov;86(5):817–833. [PubMed] [Google Scholar]
- Vale J. A., Rees A. J., Widdop B., Goulding R. Use of charcoal haemoperfusion in the management of severely poisoned patients. Br Med J. 1975 Jan 4;1(5948):5–9. doi: 10.1136/bmj.1.5948.5. [DOI] [PMC free article] [PubMed] [Google Scholar]


