Abstract
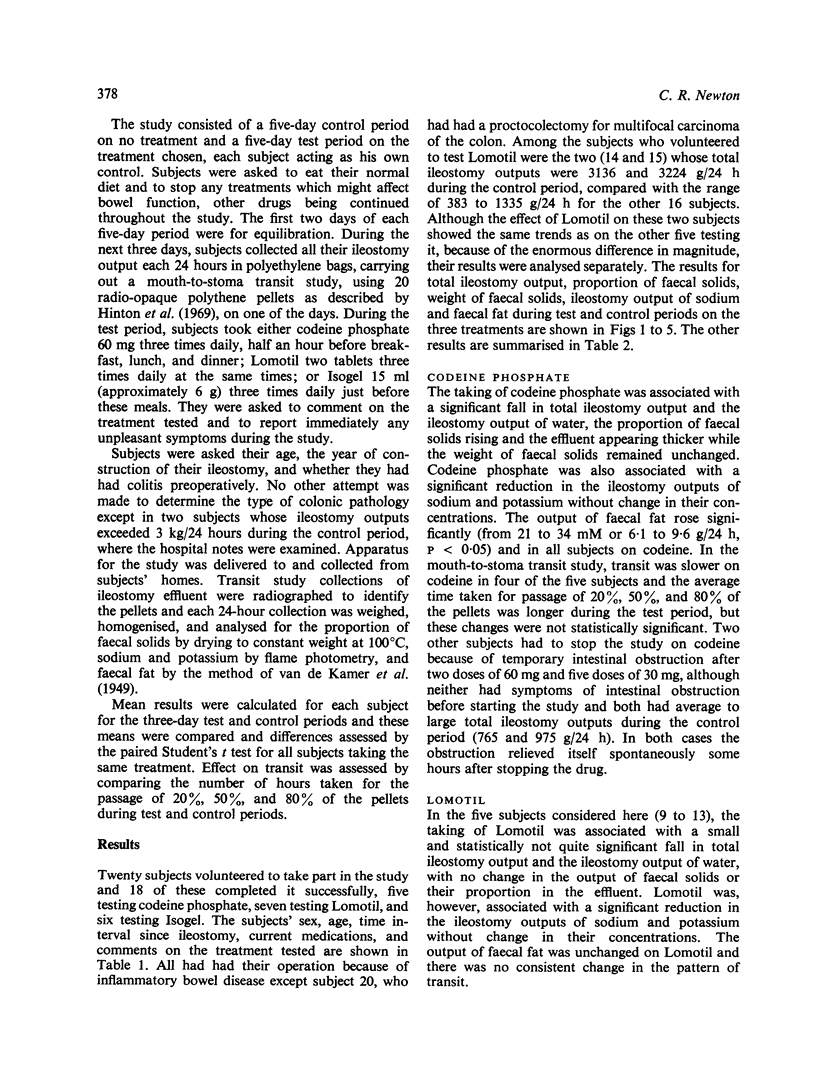
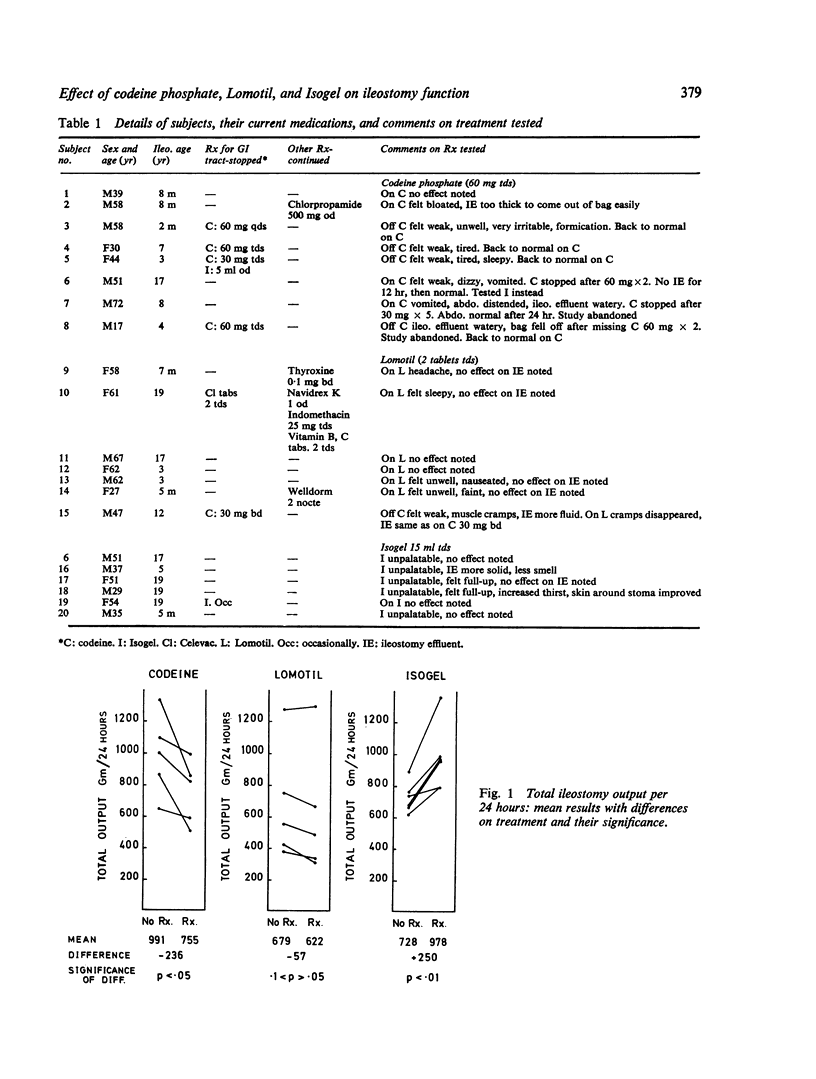
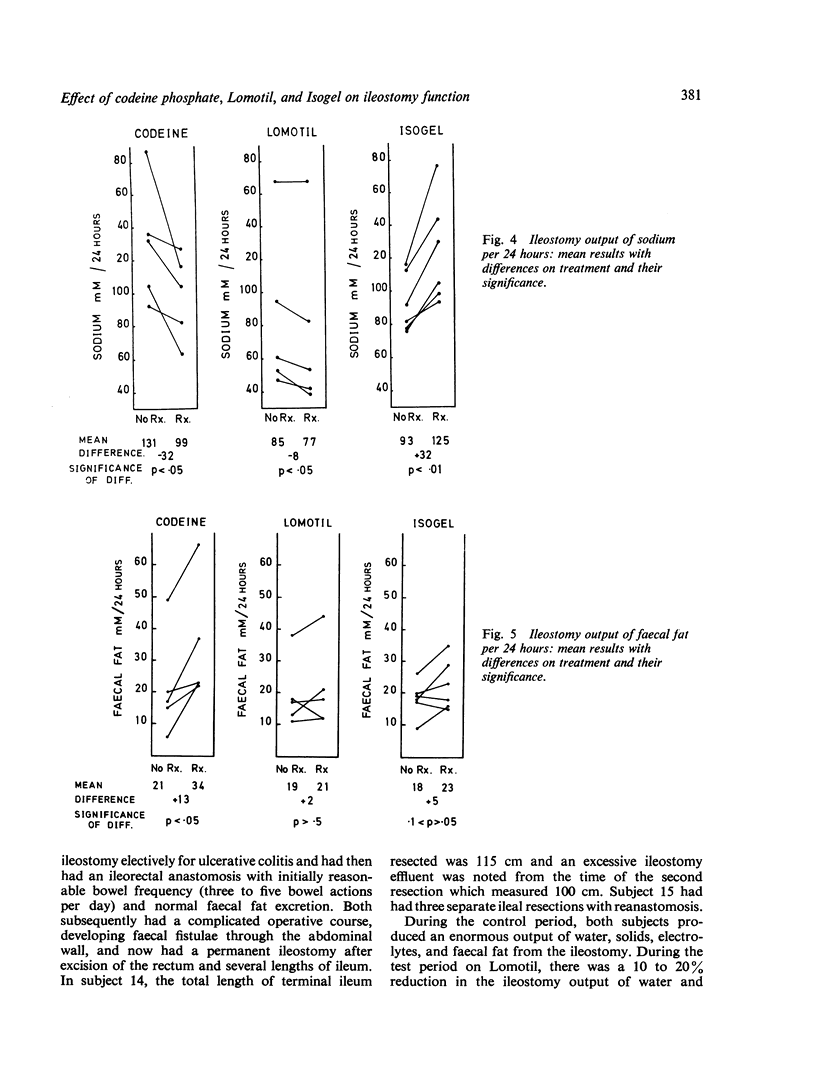
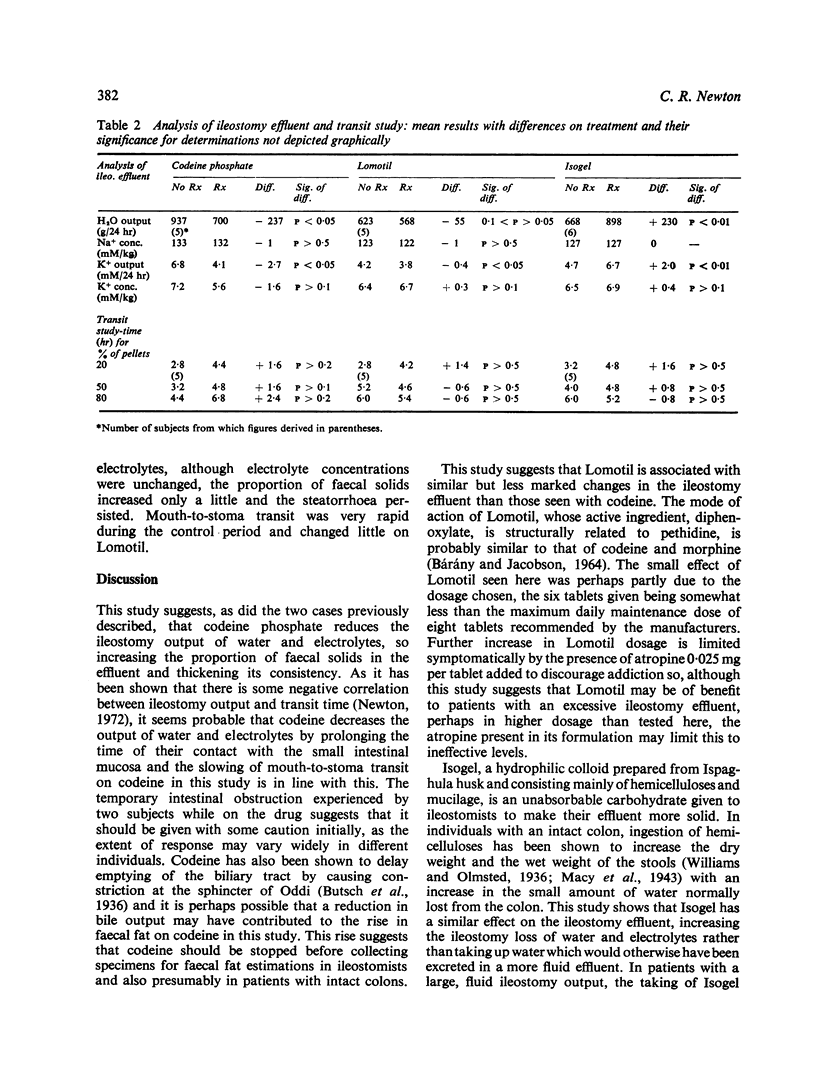
The effect on ileostomy function of codeine phosphate, Lomotil, or Isogel was tested in 20 subjects at home living a normal life, studied over two three-day periods on and off treatment. Codeine phosphate 60 mg three times daily was associated with a reduction in the mean total weight of ileostomy output and the ileostomy outputs of water, sodium, and potassium (p < 0·05). The proportion of faecal solids increased on codeine and the effluent appeared thicker but the output of faecal solids remained unchanged. Mean faecal fat increased on codeine. The transit rate from mouth to stoma was slower in four of the five subjects on codeine and a further two subjects withdrew from the trial with temporary intestinal obstruction while on the drug. Lomotil two tablets three times daily was associated with a small and statistically not quite significant fall in the mean total weight of ileostomy output and the ileostomy output of water. Sodium and potassium outputs in the effluent fell on Lomotil (p < 0·05) but the other parameters remained unchanged. Isogel 15 ml three times daily was associated with an increase in the mean total weight of ileostomy output and the ileostomy outputs of water, sodium, potassium, and faecal solids (p < 0·01). Although the effluent looked more viscid on Isogel, the proportion of faecal solids was unchanged. These results suggest that codeine phosphate has a beneficial effect on ileostomy function, reducing the loss of water and electrolytes, while Lomotil has a similar but less effective action in the dosage tested. By contrast, Isogel increases the ileostomy loss of water and electrolytes and will aggravate their depletion in patients with excessive fluid effluents. The increase in faecal fat associated with taking codeine phosphate suggests that it should be stopped before collecting specimens for faecal fat estimations.
Full text
PDF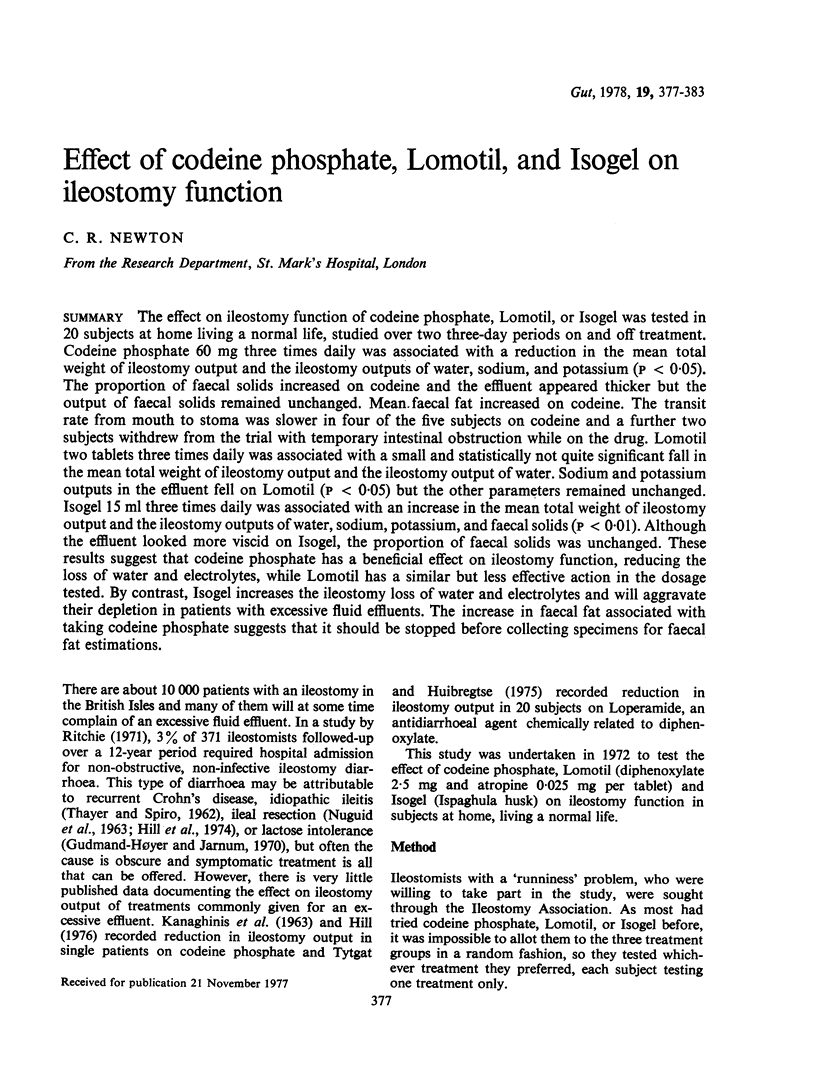

Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- BARANY F., JACOBSON B. ENDORADIOSONDE STUDY OF PROPULSION AND PRESSURE ACTIVITY INDUCED BY TEST MEALS, PROSTIGMINE, AND DIPHENOXYLATE IN THE SMALL INTESTINE. Gut. 1964 Feb;5:90–95. doi: 10.1136/gut.5.1.90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gudmand-Hoyer E., Jarnum S. Incidence and clinical significance of lactose malabsorption in ulcerative colitis and Crohn's disease. Gut. 1970 Apr;11(4):338–343. doi: 10.1136/gut.11.4.338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hill G. L., Mair W. S., Goligher J. C. Impairment of 'ileostomy adaptation' in patients after ileal resection. Gut. 1974 Dec;15(12):982–987. doi: 10.1136/gut.15.12.982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hinton J. M., Lennard-Jones J. E., Young A. C. A ne method for studying gut transit times using radioopaque markers. Gut. 1969 Oct;10(10):842–847. doi: 10.1136/gut.10.10.842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- KANAGHINIS T., LUBRAN M., COGHILL N. F. THE COMPOSITION OF ILEOSTOMY FLUID. Gut. 1963 Dec;4:322–338. doi: 10.1136/gut.4.4.322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- NUGUID T. P., BACON H. E., BOUTWELL J. THE ILEOSTOMY: ITS PHYSICAL CHARACTERISTICS AND CHEMICAL BEHAVIOR. Dis Colon Rectum. 1963 Jul-Aug;6:293–296. doi: 10.1007/BF02617268. [DOI] [PubMed] [Google Scholar]
- Newton C. R. Comparison of bowel function after colectomy and ileostomy or ileorectal anastomosis for inflammatory bowel disease. Gut. 1972 Oct;13(10):855–855. [PubMed] [Google Scholar]
- Ritchie J. K. Ileostomy and excisional surgery for chronic inflammatory disease of the colon: a survey of one hospital region. Gut. 1971 Jul;12(7):528–540. doi: 10.1136/gut.12.7.528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tytgat G. N., Huibregtse K. Loperamide and ileostomy output--placebo-controled double-blind crossover study. Br Med J. 1975 Jun 21;2(5972):667–667. doi: 10.1136/bmj.2.5972.667. [DOI] [PMC free article] [PubMed] [Google Scholar]


