Abstract
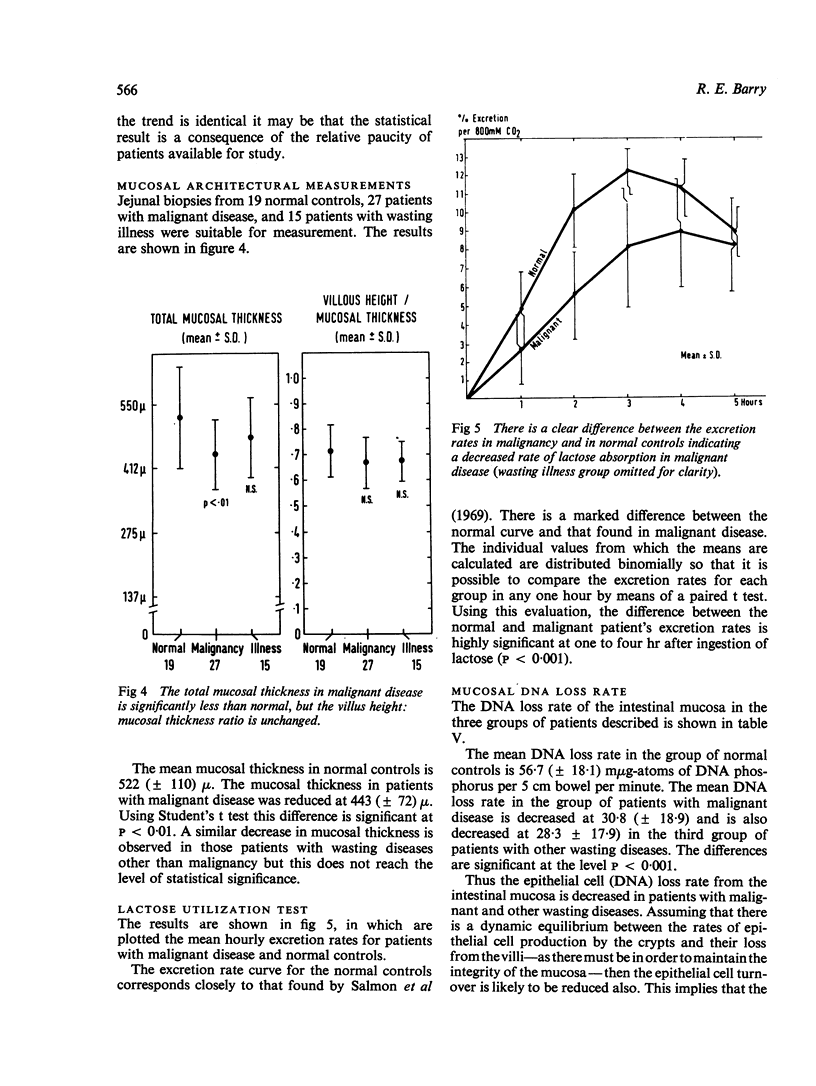
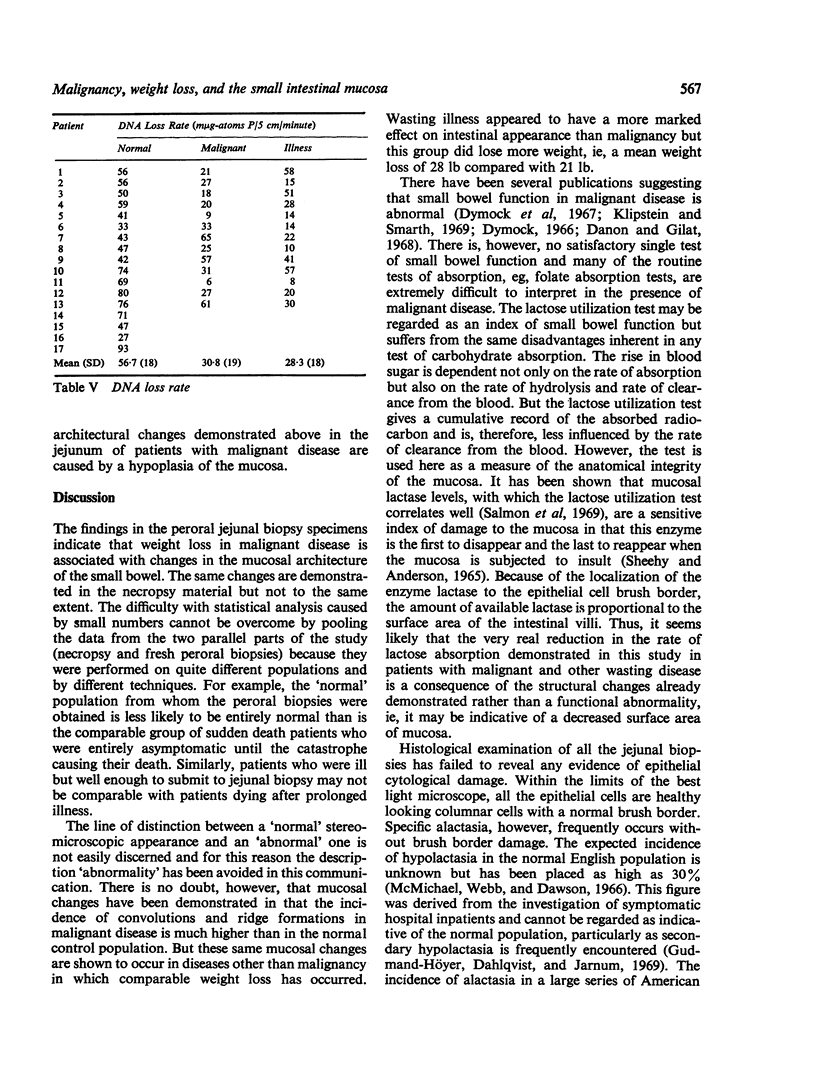
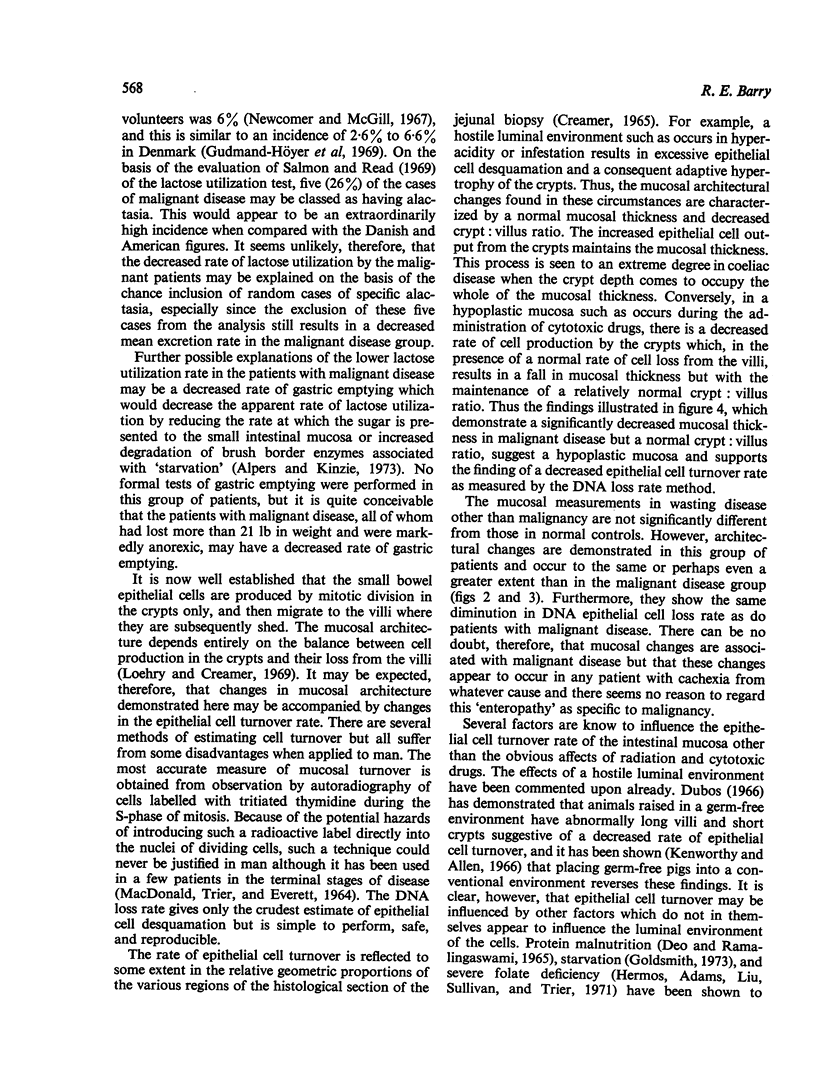
The mucosal architecture and mucosal dynamics of the small bowel have been studied in patients with malignant disease not of the gastrointestinal tract but associated with severe weight loss. Mucosal changes in malignant disease are demonstrated by stereomicroscopy, mucosal architectural measurement, and decreased lactose utilization. Measurement of the epithelial DNA loss rate indicates, in association with mucosal measurement, that the architectural changes are caused by a hypoplasia of the epithelium. Similar findings are demonstrated in patients with profound weight loss due to other non-malignant wasting diseases. Although mucosal changes undoubtedly occur in malignant disease, the changes are not specific for malignancy and the concept of `cancer enteropathy' is not tenable. It is suggested that mucosal changes are the effect of and not the cause of cachexia.
Full text
PDF
Images in this article
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Alpers D. H., Kinzie J. L. Regulation of small intestinal protein metabolism. Gastroenterology. 1973 Mar;64(3):471–496. [PubMed] [Google Scholar]
- Berndt H. Malabsorption in cancer of and outside the bowel. Digestion. 1968;1(5):305–310. doi: 10.1159/000196868. [DOI] [PubMed] [Google Scholar]
- CREAMER B. MALIGNANCY AND THE SMALL-INTESTINAL MUCOSA. Br Med J. 1964 Dec 5;2(5422):1435–1436. doi: 10.1136/bmj.2.5422.1435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DAVIDSON J. N., LESLIE I. A new approach in the biochemistry of growth and development. Nature. 1950 Jan 14;165(4185):49–53. doi: 10.1038/165049a0. [DOI] [PubMed] [Google Scholar]
- DEO M. G., RAMALINGASWAMI V. REACTION OF THE SMALL INTESTINE TO INDUCED PROTEIN MALNUTRITION IN RHESUS MONKEYS. A STUDY OF CELL POPULATION KINETICS IN THE JEJUNUM. Gastroenterology. 1965 Aug;49:150–157. [PubMed] [Google Scholar]
- Deller D. J., Murrell T. G., Blowes R. Jejunal biopsy in malignant disease. Australas Ann Med. 1967 Aug;16(3):236–241. doi: 10.1111/imj.1967.16.3.236. [DOI] [PubMed] [Google Scholar]
- Dowling R. H., Booth C. C. Structural and functional changes following small intestinal resection in the rat. Clin Sci. 1967 Feb;32(1):139–149. [PubMed] [Google Scholar]
- Dowling R. H., Gleeson M. H. Cell turnover following small bowel resection and by-pass. Digestion. 1973;8(2):176–190. doi: 10.1159/000197312. [DOI] [PubMed] [Google Scholar]
- Dubos R. The microbiota of the gastrointestinal tract. Gastroenterology. 1966 Nov;51(5):868–874. [PubMed] [Google Scholar]
- Dymock I. W. Enteropathy in malignant disease. Br J Cancer. 1966 Jun;20(2):236–238. doi: 10.1038/bjc.1966.29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dymock I. W., MacKay N., Miller V., Thomson T. J., Gray B., Kennedy E. H., Adams J. F. Small intestinal function in neoplastic disease. Br J Cancer. 1967 Sep;21(3):505–511. doi: 10.1038/bjc.1967.59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fischer R. A., Rosoff B. M., Altshuler J. H., Thayer W. R., Jr, Spiro H. M. Disacchariduria in malignant disease. Cancer. 1965 Oct;18(10):1278–1284. doi: 10.1002/1097-0142(196510)18:10<1278::aid-cncr2820181010>3.0.co;2-e. [DOI] [PubMed] [Google Scholar]
- GIRDWOOD R. H., DELAMORE I. W., WILLIAMS A. W. Jejunal biopsy in malabsorptive disorders of the adult. Br Med J. 1961 Feb 4;1(5222):319–323. doi: 10.1136/bmj.1.5222.319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gilat T., Fischel B., Danon J., Loewenthal M. Morphology of small bowel mucosa in malignancy. Digestion. 1972;7(3):147–155. doi: 10.1159/000197269. [DOI] [PubMed] [Google Scholar]
- Gleeson M. H., Cullen J., Dowling R. H. Intestinal structure and function after small bowel by-pass in the rat. Clin Sci. 1972 Dec;43(6):731–742. doi: 10.1042/cs0430731. [DOI] [PubMed] [Google Scholar]
- Goldsmith D. P. Changes in desquamation rate of jejunal epithelium in cats during fasting. Digestion. 1973;8(2):130–141. doi: 10.1159/000197308. [DOI] [PubMed] [Google Scholar]
- Gudmand-Höyer E., Dahlqvist A., Jarnum S. Specific small-intestinal lactase deficiency in adults. Scand J Gastroenterol. 1969;4(4):377–386. doi: 10.3109/00365526909180619. [DOI] [PubMed] [Google Scholar]
- Kenworthy R., Allen W. D. The significance of Escherichia Coli to the young pig. J Comp Pathol. 1966 Jan;76(1):31–44. doi: 10.1016/0021-9975(66)90045-4. [DOI] [PubMed] [Google Scholar]
- Klipstein F. A., Smarth G. Intestinal structure and function in neoplastic disease. Am J Dig Dis. 1969 Dec;14(12):887–899. doi: 10.1007/BF02233210. [DOI] [PubMed] [Google Scholar]
- LORAN M. R., ALTHAUSEN T. L. Cellular proliferation of intestinal epithelia in the rat two months after partial resection of the ileum. J Biophys Biochem Cytol. 1960 Jul;7:667–672. doi: 10.1083/jcb.7.4.667. [DOI] [PMC free article] [PubMed] [Google Scholar]
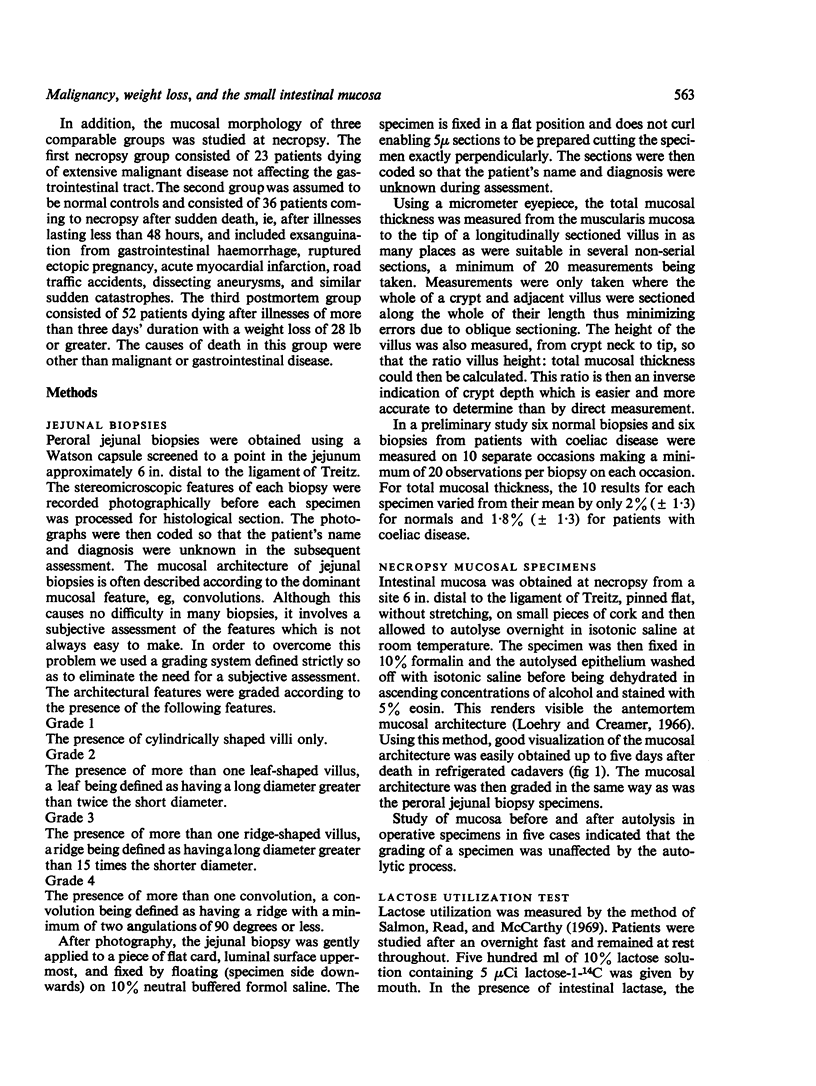
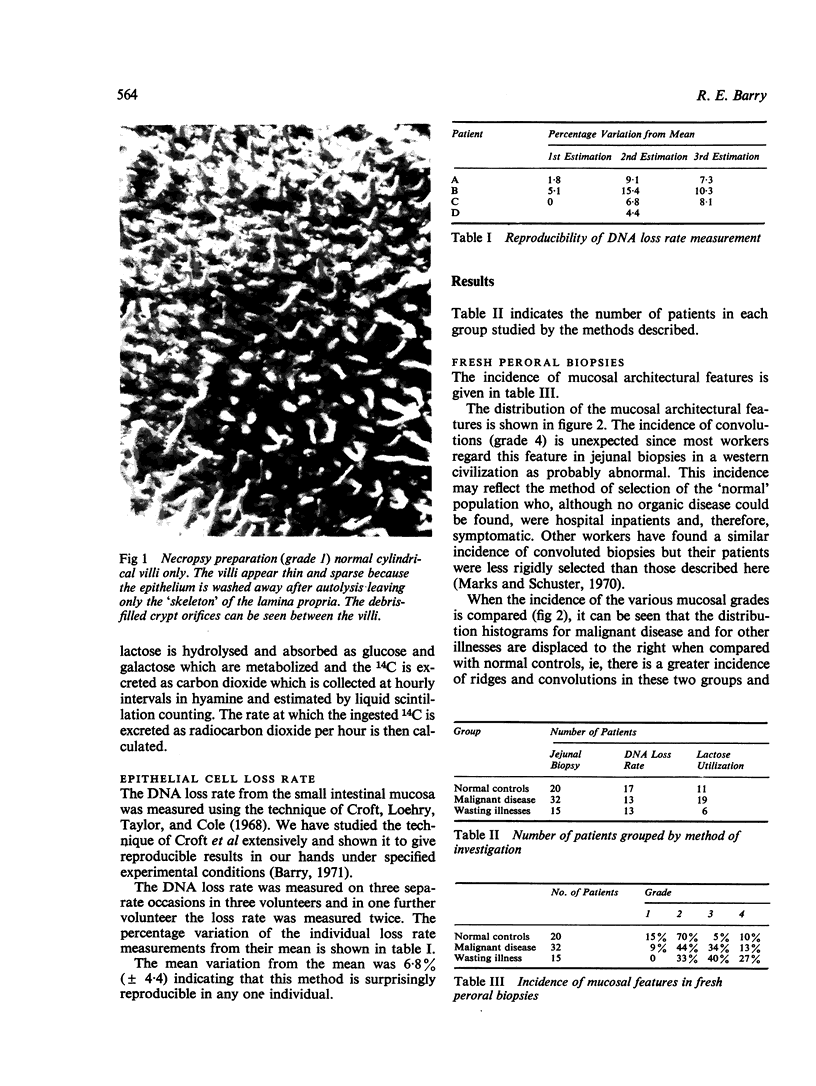
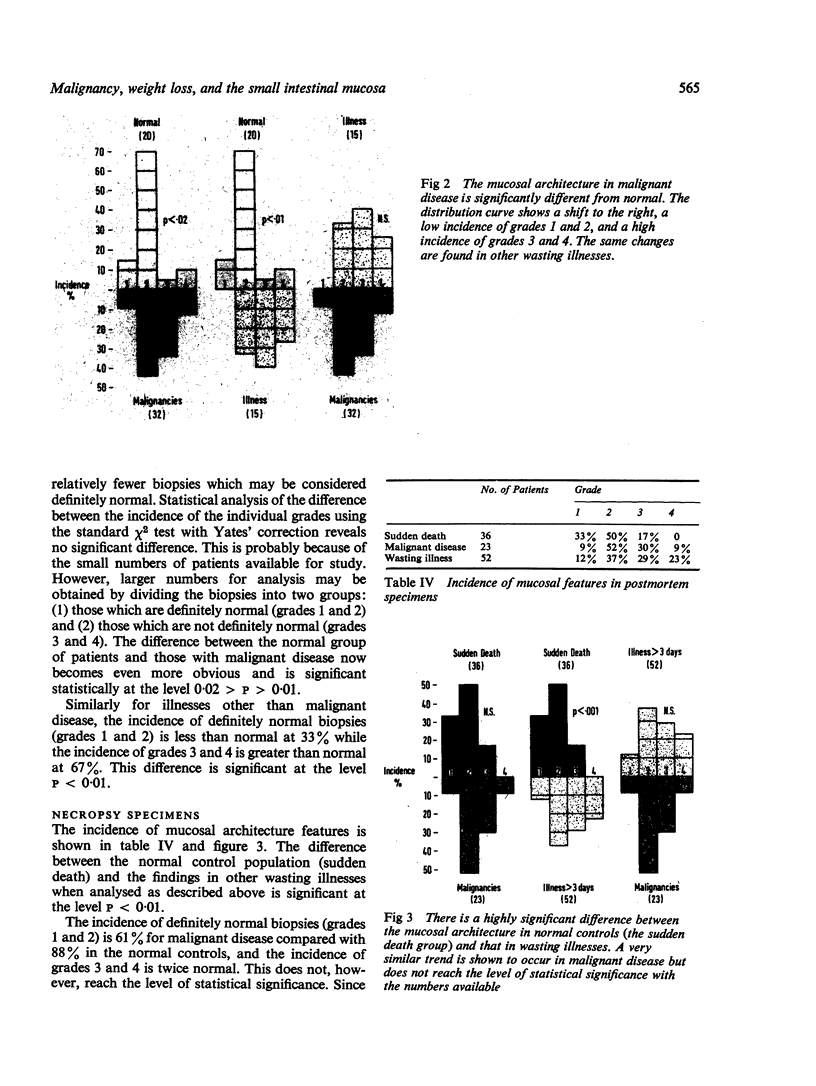
- Loehry C. A., Creamer B. Post-mortem Study of Small-intestinal Mucosa. Br Med J. 1966 Apr 2;1(5491):820.2–82829. doi: 10.1136/bmj.1.5491.820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Loehry C. A., Creamer B. Three-demensional structure of the rat small intestinal mucosa related to mucosal dynamics. I. Mucosal structure and dynamics in the rat after the administration of methotrexate. Gut. 1969 Feb;10(2):112–116. doi: 10.1136/gut.10.2.112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MACDONALD W. C., TRIER J. S., EVERETT N. B. CELL PROLIFERATION AND MIGRATION IN THE STOMACH, DUODENUM, AND RECTUM OF MAN: RADIOAUTOGRAPHIC STUDIES. Gastroenterology. 1964 Apr;46:405–417. [PubMed] [Google Scholar]
- Marks J., Shuster S. Small-intestinal mucosal abnormalities in various skin diseases--fact or fancy? Gut. 1970 Apr;11(4):281–291. doi: 10.1136/gut.11.4.281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McMichael H. B., Webb J., Dawson A. M. Jejunal disaccharidases and some observations on the cause of lactase deficiency. Br Med J. 1966 Oct 29;2(5521):1037–1041. doi: 10.1136/bmj.2.5521.1037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Newcomer A. D., McGill D. B. Disaccharidase activity in the small intestine: prevalence of lactase deficiency in 100 healthy subjects. Gastroenterology. 1967 Dec;53(6):881–889. [PubMed] [Google Scholar]
- Pittman F. E. Primary malabsorption following extreme attempts to lose weight. Gut. 1966 Apr;7(2):154–158. doi: 10.1136/gut.7.2.154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salmon P. R., Read A. E., McCarthy C. F. An isotope technique for measuring lactose absorption. Gut. 1969 Aug;10(8):685–689. doi: 10.1136/gut.10.8.685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- WANGEL A. G., DELLER D. J. MALABSORPTION SYNDROME ASSOCIATED WITH CARCINOMA OF THE BRONCHUS. Gut. 1965 Feb;6:73–76. doi: 10.1136/gut.6.1.73. [DOI] [PMC free article] [PubMed] [Google Scholar]