Abstract
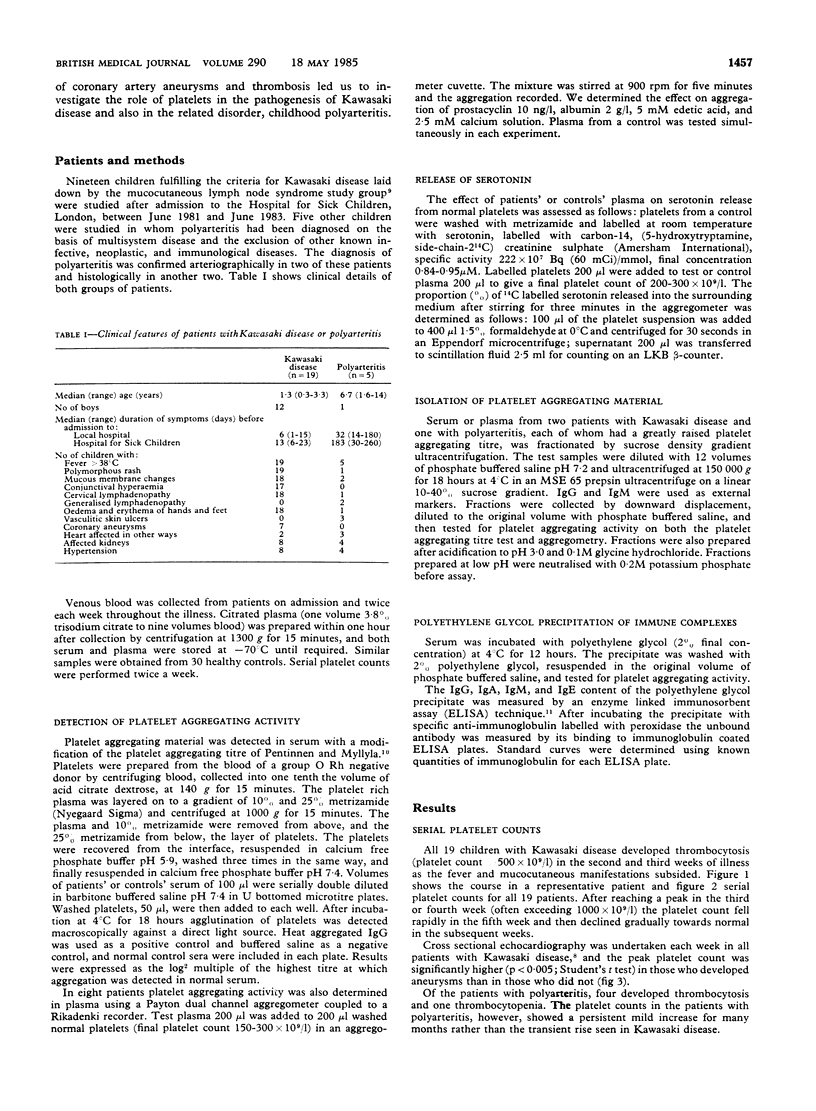
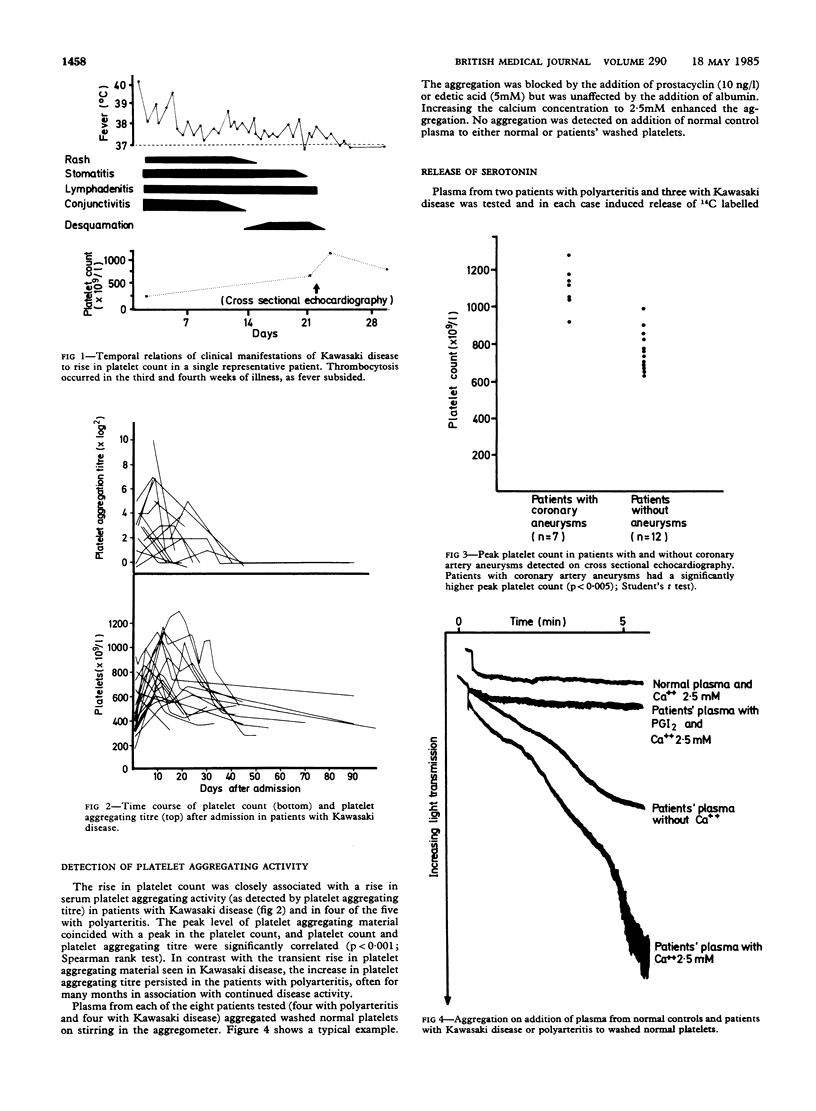
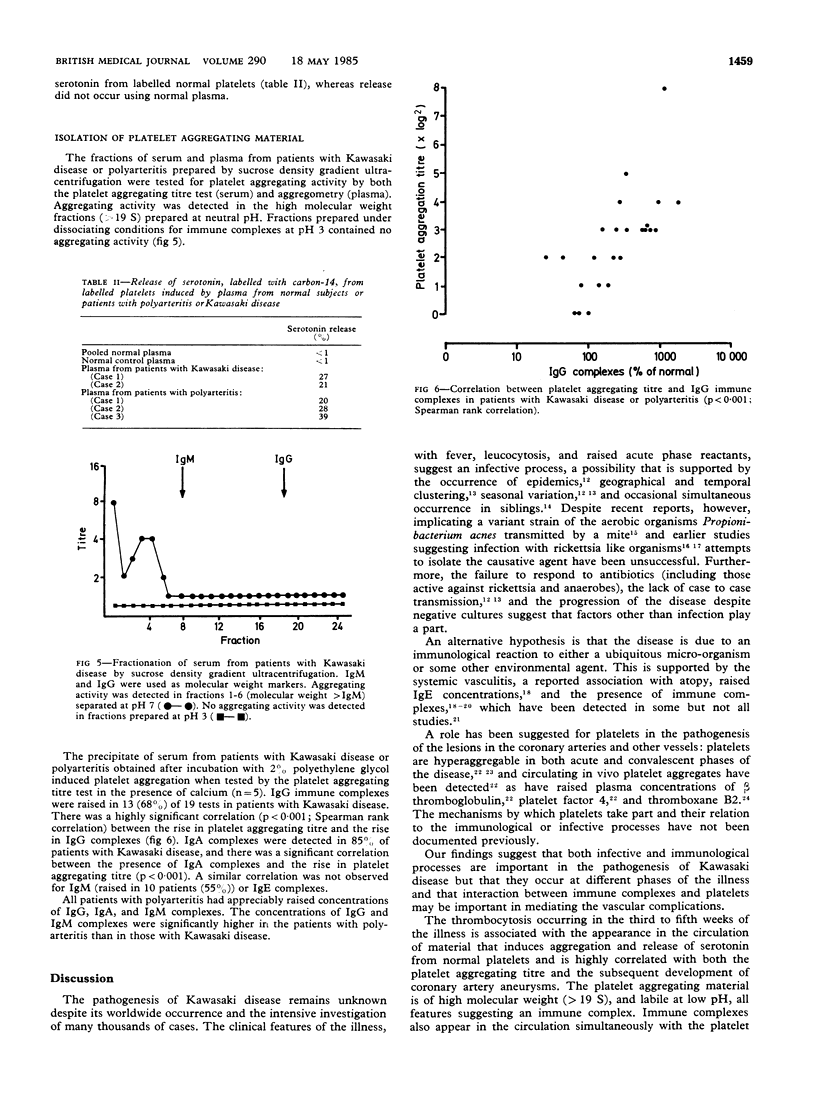
The role of platelets in the pathogenesis of vasculitis and the formation of coronary artery aneurysms was studied in 19 children with Kawasaki disease and five with polyarteritis. All patients with Kawasaki disease developed thrombocytosis in the third week of illness. The peak platelet count was significantly correlated (p less than 0.005) with the subsequent development of coronary artery aneurysms. The rise in platelet count was associated with the appearance in the circulation of a factor that induced aggregation and serotonin release in normal platelets. This factor was shown to be of high molecular weight, and its activity was lost at low pH--features suggestive of an immune complex. Immune complexes, detected by precipitation with polyethylene glycol, also appeared in the circulation as the platelet count increased. These complexes induced platelet aggregation, and there was a significant correlation (p less than 0.001) between the concentrations of IgG and IgA in the polyethylene glycol precipitated material and the platelet aggregating activity. Similar platelet aggregating activity was also detected in patients with polyarteritis but followed a different time course, persisting in the circulation for several months in association with continued disease activity. These findings imply that different mechanisms have a role in distinct phases of Kawasaki disease. The initial feverish phase (probably infective) is probably followed by an immune complex vasculitis that occurs when antibodies to the initiating agent appear in the circulation. The immune complexes aggregate platelets and induce release of serotonin. Platelet derived vasoactive mediators may increase vascular permeability and facilitate further deposition of complexes in the tissues.
Full text
PDF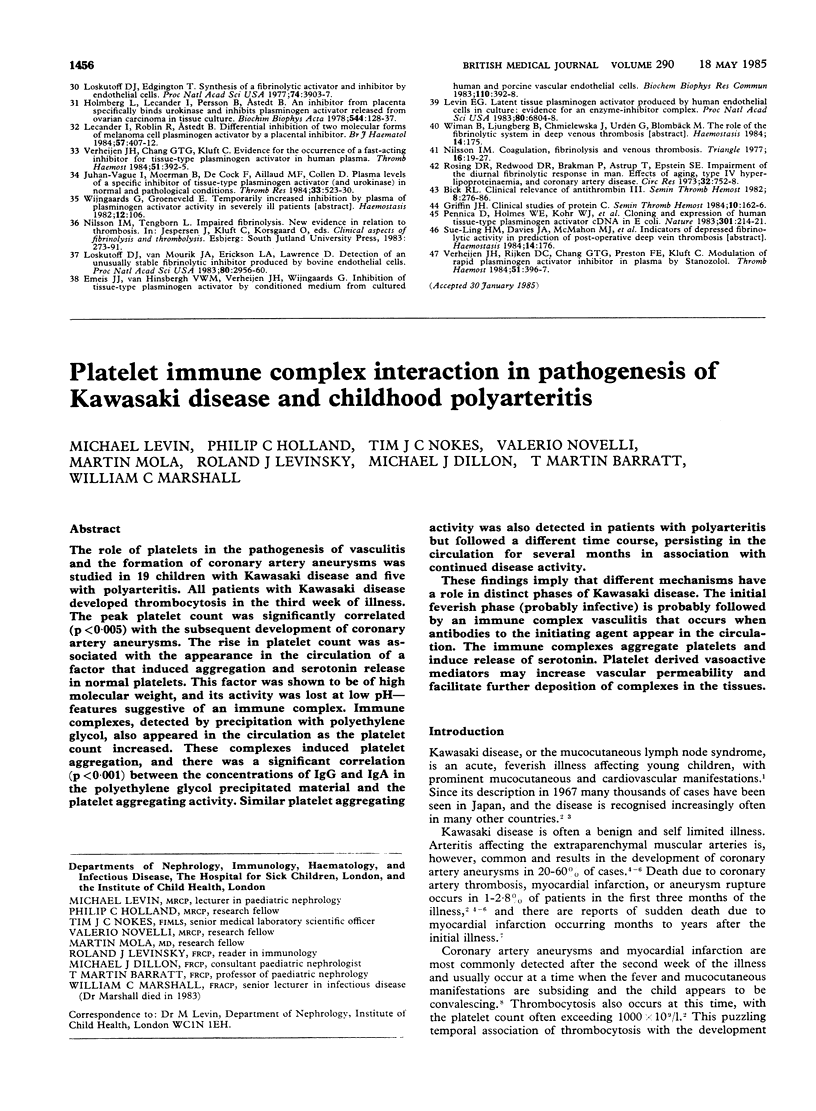
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- BENACERRAF B., SEBESTYEN M., COOPER N. S. The clearance of antigen antibody complexes from the blood by the reticuloendothelial system. J Immunol. 1959 Feb;82(2):131–137. [PubMed] [Google Scholar]
- Bhattacharya J., Bennett M. J., Tucker S. M. Long term follow up of newborns tested with the auditory response cradle. Arch Dis Child. 1984 Jun;59(6):504–511. doi: 10.1136/adc.59.6.504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- COCHRANE C. G. STUDIES ON THE LOCALIZATION OF CIRCULATING ANTIGEN-ANTIBODY COMPLEXES AND OTHER MACROMOLECULES IN VESSELS. II. PATHOGENETIC AND PHARMACODYNAMIC STUDIES. J Exp Med. 1963 Oct 1;118:503–513. doi: 10.1084/jem.118.4.503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Damiano A., Zulaica D., Cuadrado E., Ochoa M. Immunologic findings in Kawasaki disease. Ann Intern Med. 1981 Jan;94(1):138–139. doi: 10.7326/0003-4819-94-1-138_2. [DOI] [PubMed] [Google Scholar]
- Dean A. G., Melish M. E., Hicks R., Palumbo N. E. An epidemic of Kawasaki syndrome in Hawaii. J Pediatr. 1982 Apr;100(4):552–557. doi: 10.1016/S0022-3476(82)80751-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fossard C., Thompson R. A. Mucocutaneous lymph-node syndrome (Kawasaki disease): probable soluble-complex disorder. Br Med J. 1977 Apr 2;1(6065):883–883. doi: 10.1136/bmj.1.6065.883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frank M. M., Hamburger M. I., Lawley T. J., Kimberly R. P., Plotz P. H. Defective reticuloendothelial system Fc-receptor function in systemic lupus erythematosus. N Engl J Med. 1979 Mar 8;300(10):518–523. doi: 10.1056/NEJM197903083001002. [DOI] [PubMed] [Google Scholar]
- Fujimoto T., Kato H., Ichiose E., Sasaguri Y. Immune complex and mite antigen in Kawasaki disease. Lancet. 1982 Oct 30;2(8305):980–981. doi: 10.1016/s0140-6736(82)90174-x. [DOI] [PubMed] [Google Scholar]
- GOCKE D. J., OSLER A. G. IN VITRO DAMAGE OF RABBIT PLATELETS BY AN UNRELATED ANTIGEN-ANTIBODY REACTION. I. GENERAL CHARACTERISTICS OF THE REACTION. J Immunol. 1965 Feb;94:236–246. [PubMed] [Google Scholar]
- Haakenstad A. O., Mannik M. Saturation of the reticuloendothelial system with soluble immune complexes. J Immunol. 1974 May;112(5):1939–1948. [PubMed] [Google Scholar]
- Hamashima Y., Kishi K., Tasaka K. Rickettsia-like bodies in infantile acute febrile mucocutaneous lymph-node syndrome. Lancet. 1973 Jul 7;2(7819):42–42. doi: 10.1016/s0140-6736(73)91975-2. [DOI] [PubMed] [Google Scholar]
- Kato H., Fujimoto T., Inoue O., Kondo M., Koga Y., Yamamoto S., Shingu M., Tominaga K., Sasaguri Y. Variant strain of Propionibacterium acnes: a clue to the aetiology of Kawasaki disease. Lancet. 1983 Dec 17;2(8364):1383–1388. doi: 10.1016/s0140-6736(83)90921-2. [DOI] [PubMed] [Google Scholar]
- Kato H., Koike S., Yamamoto M., Ito Y., Yano E. Coronary aneurysms in infants and young children with acute febrile mucocutaneous lymph node syndrome. J Pediatr. 1975 Jun;86(6):892–898. doi: 10.1016/s0022-3476(75)80220-4. [DOI] [PubMed] [Google Scholar]
- Kato H., Koike S., Yokoyama T. Kawasaki disease: effect of treatment on coronary artery involvement. Pediatrics. 1979 Feb;63(2):175–179. [PubMed] [Google Scholar]
- Kawasaki disease in London. Lancet. 1983 Jul 16;2(8342):172–173. [PubMed] [Google Scholar]
- Kawasaki T. [Acute febrile mucocutaneous syndrome with lymphoid involvement with specific desquamation of the fingers and toes in children]. Arerugi. 1967 Mar;16(3):178–222. [PubMed] [Google Scholar]
- Kniker W. T., Cochrane C. G. The localization of circulating immune complexes in experimental serum sickness. The role of vasoactive amines and hydrodynamic forces. J Exp Med. 1968 Jan 1;127(1):119–136. doi: 10.1084/jem.127.1.119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kusakawa S., Heiner D. C. Elevated levels of immunoglobulin E in the acute febrile mucocutaneous lymph node syndrome. Pediatr Res. 1976 Feb;10(2):108–111. doi: 10.1203/00006450-197602000-00007. [DOI] [PubMed] [Google Scholar]
- Landing B. H., Larson E. J. Are infantile periarteritis nodosa with coronary artery involvement and fatal mucocutaneous lymph node syndrome the same? Comparison of 20 patients from North America with patients from Hawaii and Japan. Pediatrics. 1977 May;59(5):651–662. [PubMed] [Google Scholar]
- Lockwood C. M., Worlledge S., Nicholas A., Cotton C., Peters D. K. Reversal of impaired splenic function in patients with nephritis or vasculitis (or both) by plasma exchange. N Engl J Med. 1979 Mar 8;300(10):524–530. doi: 10.1056/NEJM197903083001003. [DOI] [PubMed] [Google Scholar]
- Meade R. H., 3rd, Brandt L. Manifestations of Kawasaki disease in New England outbreak of 1980. J Pediatr. 1982 Apr;100(4):558–562. doi: 10.1016/s0022-3476(82)80752-x. [DOI] [PubMed] [Google Scholar]
- Morens D. M., Anderson L. J., Hurwitz E. S. National surveillance of Kawasaki disease. Pediatrics. 1980 Jan;65(1):21–25. [PubMed] [Google Scholar]
- Penttinen K., Myllylä G. Interaction in human blood platelets, viruses and antibodies. I. Platelet aggregation test with microequipment. Ann Med Exp Biol Fenn. 1968;46(2):188–192. [PubMed] [Google Scholar]
- Tanaka N. Kawasaki disease (acute febrile infantile muco-cutaneous lymph node syndrome) in Japan; relationship with infantile periarteritis nodosa. Pathol Microbiol (Basel) 1975;43(2-O):204–218. doi: 10.1159/000162822. [DOI] [PubMed] [Google Scholar]


