Full text
PDF








Images in this article
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Abe H., Carballo J., Appert H. E., Howard J. M. The release and fate of the intestinal lysosomal enzymes after acute ischemic injury of the intestine. Surg Gynecol Obstet. 1972 Oct;135(4):581–585. [PubMed] [Google Scholar]
- Ahrén C., Haglund U. Mucosal lesions in the small intestine of the cat during low flow. Acta Physiol Scand. 1973 Aug;88(4):541–550. doi: 10.1111/j.1748-1716.1973.tb05483.x. [DOI] [PubMed] [Google Scholar]
- BOLEY S. J., SCHWARTZ S., LASH J., STERNHILL V. Reversible vascular occlusion of the colon. Surg Gynecol Obstet. 1963 Jan;116:53–60. [PubMed] [Google Scholar]
- Bloch R., Menge H., Lingelbach B., Lorenz-Meyer H., Haberich F. J., Riecken E. O. The relationship between structure and function of small intestine in patients with a sprue syndrome and in healthy controls. Klin Wochenschr. 1973 Dec 1;51(23):1151–1158. doi: 10.1007/BF01468564. [DOI] [PubMed] [Google Scholar]
- Boley S. J., Krieger H., Schultz L., Robinson K., Siew F. P., Allen A. C., Schwartz S. Experimental aspects of peripheral vascular occlusion of the intestine. Surg Gynecol Obstet. 1965 Oct;121(4):789–794. [PubMed] [Google Scholar]
- Bounous G., Konok G. Intestinal brush border enzymes after short-term mesenteric ischemia. Am J Surg. 1977 Mar;133(3):304–306. doi: 10.1016/0002-9610(77)90533-5. [DOI] [PubMed] [Google Scholar]
- Bounous G., McArdle A. H. Release of intestinal enzymes in acute mesenteric ischemia. J Surg Res. 1969 Jun;9(6):339–346. doi: 10.1016/0022-4804(69)90078-x. [DOI] [PubMed] [Google Scholar]
- Bounous G., Menard D., De Medicis E. Role of pancreatic proteases in the pathogenesis of ischemic enteropathy. Gastroenterology. 1977 Jul;73(1):102–108. [PubMed] [Google Scholar]
- Bounous G. Metabolic changes in the intestinal mucosa during hemorrhagic shock. Can J Surg. 1965 Oct;8(4):332–339. [PubMed] [Google Scholar]
- Bounous G., Proulx J., Konok G., Wollin A. The role of bile and pancreatic proteases in the pathogenesis of ischemic enteropathy. Int J Clin Pharmacol Biopharm. 1979 Jul;17(7):317–323. [PubMed] [Google Scholar]
- Bounous G. Role of the intestinal contents in the pathophysiology of acute intestinal ischemia. Am J Surg. 1967 Sep;114(3):368–375. doi: 10.1016/0002-9610(67)90158-4. [DOI] [PubMed] [Google Scholar]
- Brown R. A., Chiu C. J., Scott H. J., Gurd F. N. Ultrastructural changes in the canine ileal mucosal cell after mesenteric arterial occlusion. Arch Surg. 1970 Aug;101(2):290–297. doi: 10.1001/archsurg.1970.01340260194029. [DOI] [PubMed] [Google Scholar]
- CAMERON G. R., KHANNA S. D. Regeneration of the intestinal villi after extensive mucosal infarction. J Pathol Bacteriol. 1959 Apr;77(2):505–510. doi: 10.1002/path.1700770222. [DOI] [PubMed] [Google Scholar]
- Chiu C. J., McArdle A. H., Brown R., Scott H. J., Gurd F. N. Intestinal mucosal lesion in low-flow states. I. A morphological, hemodynamic, and metabolic reappraisal. Arch Surg. 1970 Oct;101(4):478–483. doi: 10.1001/archsurg.1970.01340280030009. [DOI] [PubMed] [Google Scholar]
- Chiu C. J., Scott H. J., Gurd F. N. Intestinal mucosal lesion in low-flow states. II. The protective effect of intraluminal glucose as energy substrate. Arch Surg. 1970 Oct;101(4):484–488. doi: 10.1001/archsurg.1970.01340280036010. [DOI] [PubMed] [Google Scholar]
- Clermont H. G., Williams J. S. Lymph lysosomal enzyme acid phosphatase in hemorrhagic shock. Ann Surg. 1972 Jul;176(1):90–96. doi: 10.1097/00000658-197207000-00016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cook B. H., Wilson E. R., Jr, Taylor A. E. Intestinal fluid loss in hemorrhagic shock. Am J Physiol. 1971 Nov;221(5):1494–1498. doi: 10.1152/ajplegacy.1971.221.5.1494. [DOI] [PubMed] [Google Scholar]
- Courtice F. C., Adams E. P., Shannon A. D., Bishop D. M. Acid hydrolases in the rabbit in haemorrhagic shock. Q J Exp Physiol Cogn Med Sci. 1974 Jan;59(1):31–42. doi: 10.1113/expphysiol.1974.sp002239. [DOI] [PubMed] [Google Scholar]
- De Villiers D. R. Ischaemia of the colon: an experimental study. Br J Surg. 1966 Jun;53(6):497–503. doi: 10.1002/bjs.1800530604. [DOI] [PubMed] [Google Scholar]
- Eastwood G. L. Gastrointestinal epithelial renewal. Gastroenterology. 1977 May;72(5 Pt 1):962–975. [PubMed] [Google Scholar]
- GLOTZER D. J., VILLEGAS A. H., ANEKAMAYA S., SHAW R. S. Healing of the intestine in experimental bowel infarction. Ann Surg. 1962 Feb;155:183–190. doi: 10.1097/00000658-196200000-00003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- GUTHRIE J. E., QUASTEL J. H. Absorption of sugars and amino acids from isolated surviving intestine after experimental shock. Arch Biochem Biophys. 1956 Jun;62(2):485–496. doi: 10.1016/0003-9861(56)90147-3. [DOI] [PubMed] [Google Scholar]
- Gabbert H., Wagner R., Aust P., Höhn P. Ischemia and post-ischemic regeneration of the small intestinal mucosa. An enzyme-histochemical investigation. Acta Histochem. 1978;63(2):197–213. doi: 10.1016/S0065-1281(78)80026-9. [DOI] [PubMed] [Google Scholar]
- Haglund U., Lundholm K., Lundgren O., Scherstén T. Intestinal lysosomal enzyme activity in regional simulated shock: influence of methylprednisolone and albumin. Circ Shock. 1977;4(1):27–34. [PubMed] [Google Scholar]
- Hueckel H. J., Chiu C. J., Hinchey E. J. The effect of intraluminally administered glucose in reducing fluid and electrolyte loss from the ischemic intestine. Surg Gynecol Obstet. 1973 May;136(5):780–784. [PubMed] [Google Scholar]
- KHANNA S. D. An experimental study of mesenteric occlusion. J Pathol Bacteriol. 1959 Apr;77(2):575–590. doi: 10.1002/path.1700770229. [DOI] [PubMed] [Google Scholar]
- Kingham J. G., Whorwell P. J., Loehry C. A. Small intestinal permeability. 1. Effects of ischaemia and exposure to acetyl salicylate. Gut. 1976 May;17(5):354–361. doi: 10.1136/gut.17.5.354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luisier A. L., Robinson J. W. Glycolysis as an energy source for intestinal transport of amino acids: comparison between rat and guinea-pig. Comp Biochem Physiol A Comp Physiol. 1975 May 1;51(1A):105–109. doi: 10.1016/0300-9629(75)90421-1. [DOI] [PubMed] [Google Scholar]
- Manohar M., Tyagi R. P. Experimental intestinal ischemia shock in dogs. Am J Physiol. 1973 Oct;225(4):887–892. doi: 10.1152/ajplegacy.1973.225.4.887. [DOI] [PubMed] [Google Scholar]
- Marston A., Marcuson R. W., Chapman M., Arthur J. F. Experimental study of devascularization of the colon. Gut. 1969 Feb;10(2):121–130. doi: 10.1136/gut.10.2.121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McArdle A. H., Chiu C. J., Gurd F. N. Intraluminal glucose: substrate for ischemic intestine. Arch Surg. 1972 Sep;105(3):441–445. doi: 10.1001/archsurg.1972.04180090046012. [DOI] [PubMed] [Google Scholar]
- McDonel J. L., Duncan C. L. Effects of Clostridium perfringens enterotoxin on metabolic indexes of everted rat ileal sacs. Infect Immun. 1975 Aug;12(2):274–280. doi: 10.1128/iai.12.2.274-280.1975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McDonel J. L., Duncan C. L. Regional localization of activity of Clostridium perfringens type A enterotoxin in the rabbit ileum, jejunum, and duodenum. J Infect Dis. 1977 Nov;136(5):661–666. doi: 10.1093/infdis/136.5.661. [DOI] [PubMed] [Google Scholar]
- Menge H., Gottesbüren H., Riecken E. O. Zum diagnostischen Aussagewert von segmentaler Perfusionsmethode, Fettbilanz und indirekten Dünndarmfunktionstests. Vergleichende Untersuchungen. Dtsch Med Wochenschr. 1973 Dec 14;98(50):2397–2402. doi: 10.1055/s-0028-1107264. [DOI] [PubMed] [Google Scholar]
- Menge H., Robinson J. W. Early phase of jejunal regeneration after short term ischemia in the rat. Lab Invest. 1979 Jan;40(1):25–30. [PubMed] [Google Scholar]
- Mirkovitch V., Menge H., Robinson J. W. Protection of the intestinal mucosa during ischaemia by intraluminal perfusion. Res Exp Med (Berl) 1975 Dec 11;166(2):183–191. doi: 10.1007/BF01851184. [DOI] [PubMed] [Google Scholar]
- Mirkovitch V., Robinson J. W., Menge H., Cobo F. The consequences of ischaemia after mechanical obstruction of the dog ileum. Res Exp Med (Berl) 1976 Jul 22;168(1):45–55. doi: 10.1007/BF01851732. [DOI] [PubMed] [Google Scholar]
- Modigliani R., Matchansky C., Bernier J. J. Depressed jejunal secretion of water and ions in response to prostaglandin E1 in adult celiac disease. Dig Dis Sci. 1979 Oct;24(10):763–768. doi: 10.1007/BF01317209. [DOI] [PubMed] [Google Scholar]
- Parks T. G. Experimental non-gangrenous mesenteric ischaemia. Acta Gastroenterol Belg. 1974 Dec;37(12):529–538. [PubMed] [Google Scholar]
- Rausis C., Robinson J. W., Mirkovitch V., Saegesser F. Désordres vasculaires du gros intestin: données expérimentales et corrélations cliniques. Helv Chir Acta. 1973 Mar;40(1):295–305. [PubMed] [Google Scholar]
- Riecken E. O., Stewart J. S., Dowling R. H. Neuere Methoden in der Diagnostik intestinaler Störungen. Internist (Berl) 1966 May;7(5):209–217. [PubMed] [Google Scholar]
- Rijke R. P., Gart R. Epithelial cell kinetics in the descending colon of the rat. I. The effect of ischaemia-induced epithelial cell loss. Virchows Arch B Cell Pathol Incl Mol Pathol. 1979;31(1):15–22. doi: 10.1007/BF02889918. [DOI] [PubMed] [Google Scholar]
- Rijke R. P., Hanson W. R., Plaisier H. M., Osborne J. W. The effect of ischemic villus cell damage on crypt cell proliferation in the small intestine: evidence for a feedback control mechanism. Gastroenterology. 1976 Nov;71(5):786–792. [PubMed] [Google Scholar]
- Robinson J. W., Antonioli J. A., Mirkovitch V. The intestinal response to ischaemia. Naunyn Schmiedebergs Arch Pharmakol Exp Pathol. 1966;255(2):178–191. doi: 10.1007/BF00543211. [DOI] [PubMed] [Google Scholar]
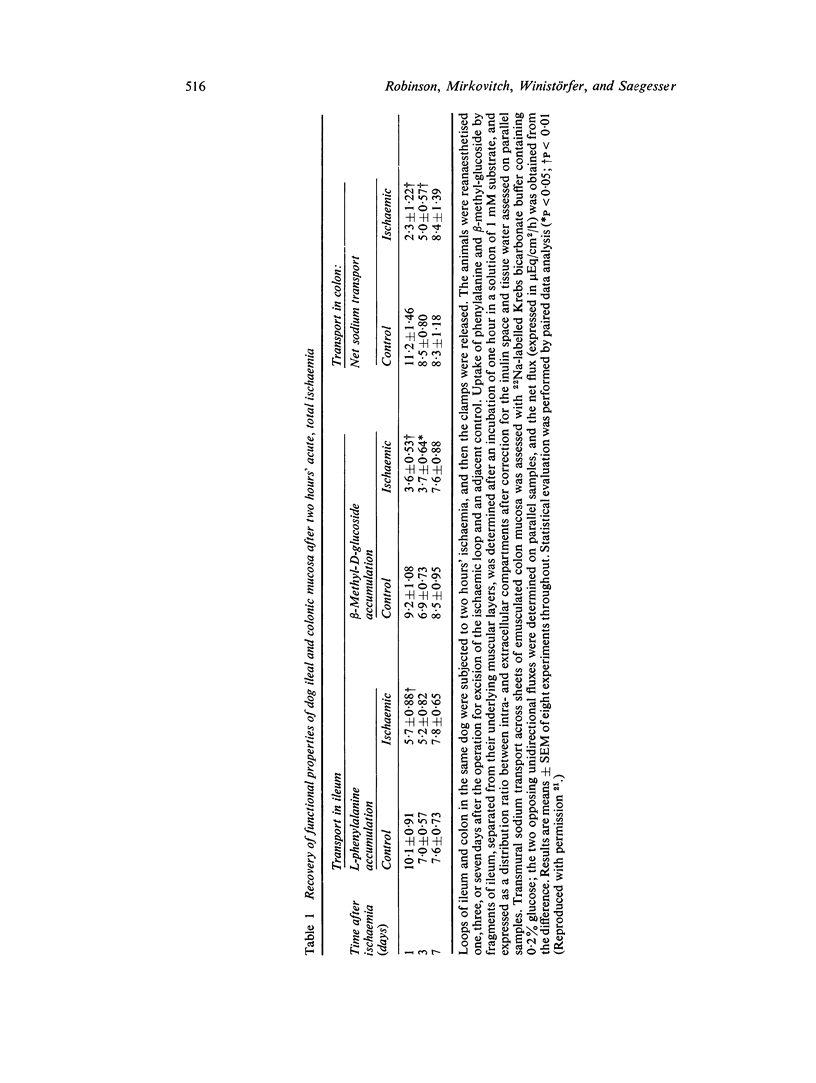
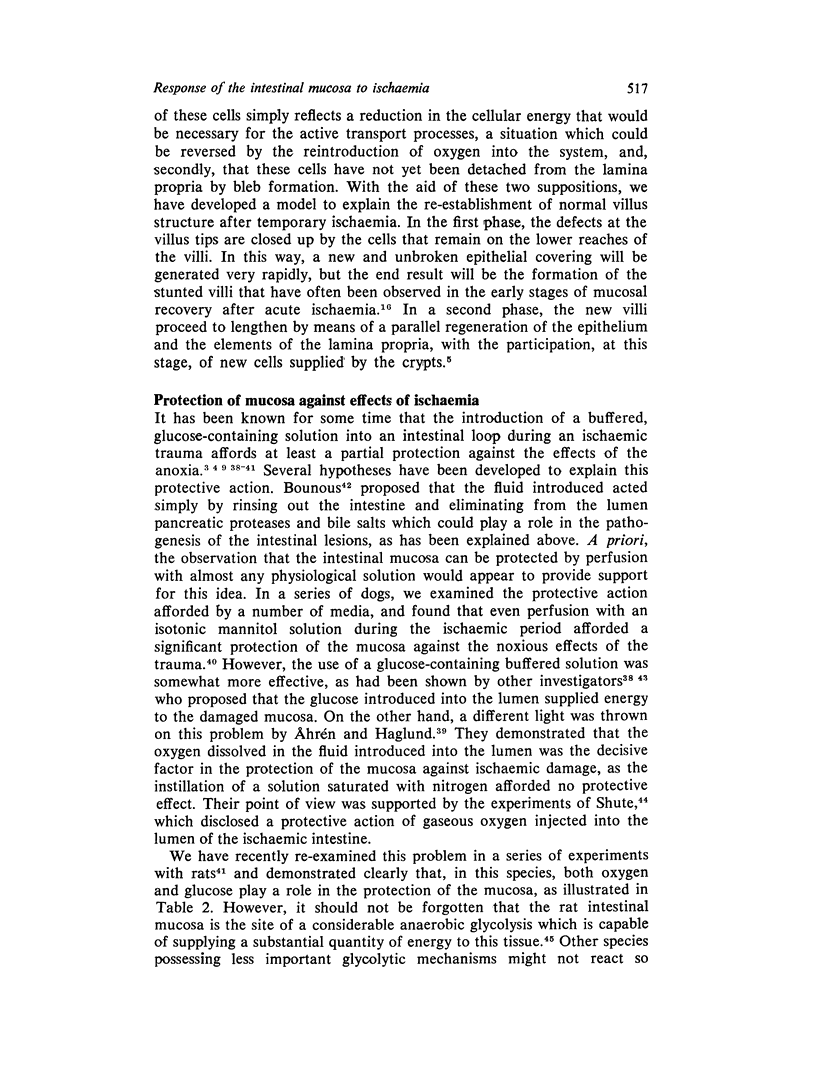
- Robinson J. W., Haroud M., Winistörfer B., Mirkovitch V. Recovery of function and structure of dog ileum and colon following two hours' acute ischaemia. Eur J Clin Invest. 1974 Dec 5;4(6):443–452. doi: 10.1111/j.1365-2362.1974.tb00418.x. [DOI] [PubMed] [Google Scholar]
- Robinson J. W., Luisier A. L., Mirkovitch V. Transport of amino-acids and sugars by the dog colonic mucosa. Pflugers Arch. 1973;345(4):317–326. doi: 10.1007/BF00585850. [DOI] [PubMed] [Google Scholar]
- Robinson J. W., Menge H., Mirkovitch V. The response of the dog colon mucosa one hour's ischaemia. Res Exp Med (Berl) 1975 Jul 14;165(2):127–134. doi: 10.1007/BF01854838. [DOI] [PubMed] [Google Scholar]
- Robinson J. W., Menge H., Sepúlveda F. V., Cobo F., Mirkovitch V. The functional response of the dog ileum to one hour's ischaemia. Clin Sci Mol Med. 1976 Feb;50(2):115–122. doi: 10.1042/cs0500115. [DOI] [PubMed] [Google Scholar]
- Robinson J. W., Mirkovitch V., Sepúlveda F. V., Menge H. Enhanced non-electrolyte uptake in vitro by the dog jejunal mucosa in the cholera-toxin-induced secretory phase. J Physiol (Paris) 1977 Jun;73(1):5–12. [PubMed] [Google Scholar]
- Robinson J. W., Mirkovitch V. The recovery of function and microcirculation in small intestinal loops following ischaemia. Gut. 1972 Oct;13(10):784–789. doi: 10.1136/gut.13.10.784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robinson J. W., Mirkovitch V. The roles on intraluminal oxygen and glucose in the protection of the rat intestinal mucosa from the effects of ischaemia. Biomedicine. 1977 Mar;27(2):60–62. [PubMed] [Google Scholar]
- Robinson J. W., Rausis C., Basset P., Mirkovitch V. Functional and morphological response of the dog colon to ischaemia. Gut. 1972 Oct;13(10):775–783. doi: 10.1136/gut.13.10.775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robinson J. W., Winistörfer B., Mirkovitch V. Source of net water and electrolyte loss following intestinal ischaemia. Res Exp Med (Berl) 1980;176(3):263–275. doi: 10.1007/BF01855846. [DOI] [PubMed] [Google Scholar]
- Röttger P., Oran M. Histochemische und biochemische Untersuchungen zur Frage des Enzym-Gehaltes der Dünndarmschleimhaut nach temporärer Ischämie. Verh Dtsch Ges Pathol. 1969;53:189–193. [PubMed] [Google Scholar]
- SMITH R. F., SZILAGYI D. E. Ischemia of the colon as a complication in the surgery of the abdominal aorta. Arch Surg. 1960 May;80:806–821. doi: 10.1001/archsurg.1960.01290220098012. [DOI] [PubMed] [Google Scholar]
- Saegesser F., Roenspies U., Robinson J. W. Ischemic diseases of the large intestine. Pathobiol Annu. 1979;9:303–337. [PubMed] [Google Scholar]
- Shute K. Effect of intraluminal oxygen on experimental ischaemia of the intestine. Gut. 1976 Dec;17(12):1001–1006. doi: 10.1136/gut.17.12.1001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stanley J. C., Brink B. E., Fry W. J. Experimental intestinal ischemia: provocative absorption studies following gradual celiac and superior mesenteric artery occlusion. J Surg Res. 1973 Feb;14(2):133–138. doi: 10.1016/0022-4804(73)90021-8. [DOI] [PubMed] [Google Scholar]
- Stirling C. E. Radioautographic localization of sodium pump sites in rabbit intestine. J Cell Biol. 1972 Jun;53(3):704–714. doi: 10.1083/jcb.53.3.704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sutherland N. G., Bounous G., Gurd F. N. Role of intestinal mucosal enzymes in the pathogenesis of shock. J Trauma. 1968 May;8(3):350–380. doi: 10.1097/00005373-196805000-00004. [DOI] [PubMed] [Google Scholar]
- Wagner R., Gabbert H., Höhn P. Ischemia and post-ischemic regeneration of the small intestinal mucosa. A light microscopic and autoradiographic study. Virchows Arch B Cell Pathol Incl Mol Pathol. 1979;31(3):259–276. doi: 10.1007/BF02889943. [DOI] [PubMed] [Google Scholar]
- Wagner R., Gabbert H., Höhn P. The mechanism of epithelial shedding after ischemic damage to the small intestinal mucosa. A light and electron microscopic investigation. Virchows Arch B Cell Pathol Incl Mol Pathol. 1979 May 4;30(1):25–31. doi: 10.1007/BF02889087. [DOI] [PubMed] [Google Scholar]