Short abstract
Referral management centres are intended to improve referrals between primary and secondary care. The aim is good but so far we have little evidence that they can deliver
As demand for health care outstrips supply, interest is increasing in how to manage the referral of patients by one practitioner to another for further care.1,2 Most complex health systems have considered strategies to manage demand. These initiatives began in healthcare services that provide the first point of contact for patients and entail telephone help lines, computer based decision support systems, and practitioner-led triage systems.3 Similar concepts are being developed at the interface between primary and secondary care: one such initiative is a concept known as referral management centres—a centralised process of managing referrals. Despite a lack of evidence about appropriate referrals rates4,5 and the value of such quality improvement initiatives,6 these centres seem to be expected to influence both the volume and quality of requests. Is this realistic?
Why manage referrals?
Many healthcare systems such as those in the United Kingdom, the Netherlands, and some health maintenance organisations in the United States use gatekeepers to regulate the flow of referrals from generalists to more specialised colleagues. Interest in managing demand arose in the US during the mid-1990s as health providers tried to curtail costs.7 Despite these origins, an important facet of managing demand is to encourage referrals to services that are both underused and cost effective.8 The accepted definitions recognise that management is equally concerned with creating and coping with demand as well as curtailing inappropriate flows.
Nevertheless, many initiatives seem to have an emphasis on reducing referrals.9 Referral management centres seem to have been largely set up to monitor the flow of referrals from generalists to specialists and often state that their prime aim is to curtail demand. Referral management has three potential roles: to count and monitor referrals, to assess their nature, and, perhaps, their quality, and to redirect or bar requests for referral.
Counting referrals
Comprehensive information on the volume and flow of referrals is often difficult to obtain. Nevertheless, knowledge of the volume and nature of referrals, categorised by variables such as disease, locality, urgency, and age, is essential for costing and planning services. Similarly, data on referral patterns can provide valuable indications of disease prevalence and information about the nature and quality of clinical practice.
Figure 1.
Assessing quality
Uncertainty, individual differences in interpreting risks to patients, and potential risks of litigation have led to substantial clinical variation in notions of appropriateness, making this area difficult to navigate. Guidelines focus on technical care whereas generalists take a much broader view of need.10,11 Similarly, estimates of cost effectiveness will depend on the measured used in their calculation and whether individual or population perspectives are most prominent.
Good referrals are those that send the right patient to the right service or specialist at the right time. Deviation from these principles is likely to contribute to delays in accessing specialist care and pose risks to patients. Inappropriate referrals can be considered under three broad categories:
Referrals made to the wrong service or specialist
Referrals containing insufficient information, making it difficult to assess urgency or relevance
Referrals that do not conform to accepted clinical guidance.
Referrals may be assessed for several reasons. Firstly, they may be assessed so that patients can be diverted to a service or specialist with more capacity. This is already happening in many centres and is largely welcomed. Secondly, assessment may be done purely to provide feedback to referrers. Information could be sent to the referring doctor pointing out deficiencies with the aim of improving future referrals. Thirdly, and more contentiously, referrals might be assessed to identify patients whose referral is clinically unjustified or who require further investigation in primary care. Refusal of referrals because of such judgments might result in delays and increase the risk that the patient fails to see a specialist. Generalists, specialists, and patients are likely to be concerned that assessors, who have not examined the patient, will be making decisions about the appropriateness of the referral.
Redirection
The increasing specialisation and centralisation of services makes it increasingly likely that generalists will not be fully aware of the most appropriate specialists, diagnostic tests, or treatments available for their patients. If referral management centres had a comprehensive database of services, they could potentially redirect referrals to more relevant and cost effective services—for example, diverting all upper gastroenterological endoscopy requests that met agreed guidelines to dedicated units.
What has been set up so far?
Although Faulkner and colleagues recently conducted a systematic review of the effects of service innovations on the quality and pattern of referrals,12 their work pre-dates centres to manage referrals. Managed healthcare organisations in North America use the term referral management mainly for administrative and financial pre-authorisation (checking age, address, etc).13
We searched the Cochrane Library, CINAHL, Database of Abstracts and Reviews of Effectiveness (DARE), and PubMed using terms such as referral management centre, demand management, gatekeeper, and referral assessment, and a recent systematic review6 but found no assessments of the effect of a centralised referral system and no reports of professional reactions to referral management organisations. Nevertheless, recent reports and websites describe the development of referral management centres in the NHS, notably in Merseyside,14 Hounslow,15 Greater Manchester,16 North Somerset,17 and the Vale of Glamorgan.18 Some of these centres will also integrate their work with the “choose and book” system (Kevin Hudson, Somerset Coast Primary Care Trust, personal communication).
The choose and book system is designed to help patients, in discussion with their general practitioner, to choose between hospitals and to book a suitable appointment. The system provides a directory of services and information such as waiting times linked to online or call centre systems for booking appointments.19 Reports from existing referral management centres indicate that integrating the choose and book system that is being implemented throughout England with locally organised referral management will be challenging.
Given current developments in information technology, referral management will inevitably become embedded into new systems. The key to success will be access to accurate directories of services at the local level and sensitive means to assess the nature and quality of referrals.
Implications
Referral management centres are being heralded as a means to achieve a more efficient referral process that controls demand and improves quality. A valuable byproduct could be valid data about referral patterns, which has been previously difficult to obtain. However, these initiatives could also have negative effects on the referral process, and there are reports that clinical assessment of referrals at these centres has been abandoned. A recent press release by the BMA in the UK also raised many concerns about safety and confidentiality which are still debated.20 The centres will impose a second tier of administration, and their costs may be difficult to predict. Many would want to be assured that the benefits outweigh the transaction costs.
If referral centres decide where and if patients are referred, doctors may worry that their clinical freedom is being eroded and patients may worry about the lack of choice. Some hospitals may also find that patients are being directed away from their services, which could have financial implications. Possible secondary effects of this move will be loss of communication between generalists and specialists and a decrease in the continuity of patient care. In addition, medicolegal accountability for any errors or delays that occur during assessment is unclear.
Policy assumptions
The rationale for referral centres is based on assumptions that may not hold true once these initiatives are in operation. Firstly, existing systems are viewed as inefficient and it is assumed that technological developments will help improve efficiency while also providing data about demand. Secondly, counting, assessing, and redirecting referrals is assumed to be cost effective and best done by an intermediary organisation. In the UK, these centres are funded by NHS primary care organisations, which have to reallocate resources from other services. Thirdly, secondary care organisations are assumed to be willing for others to intervene in the flow of referrals.
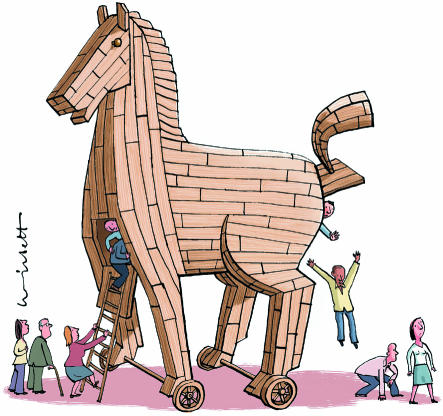
Referral management centres signal an increasing role of management in decisions about patient care, and perhaps present more evidence of increasing management interest in clinical decisions. We do not know whether referral management centres will increase or decrease risk, efficiency, or choice, and little research evidence exists to support predictions of performance. Sceptics might perceive these centres as Trojan horses, seeming to offer benefits while silently eroding aspects of clinical practice. Others are likely to welcome these initiatives as a means to manage and perhaps, eventually, to introduce quality control to a referral system that has remained largely unchanged since the inception of formal gatekeeper systems.21 In the final analysis, as demand rises, the status quo does not seem sustainable, and although these centres seem to have appeared overnight in an evidence-free zone, they are an expression of something akin to the view that many patients pass on to doctors: “Something needs to be done.”
Summary points
The volume of referrals to secondary care has become a concern in the NHS and other health systems using primary care gatekeepers
Referral management centres have been developed to monitor, assess, and redirect referrals
Evidence that the centres are effective is lacking, and costs are difficult to predict
Assessment of referrals has the potential to introduce error and delay
Patient flow may be influenced by managers rather than by clinicians
Contributors and sources: GE has worked on referral assessment and is involved in evaluating service developments on demand management. MD is currently evaluating a referral management initiative in Wales and has a background in informatics and health services research. Both authors initiated the work and reviewed the literature. Both authors drafted the article. GE acts as the guarantor.
Competing interests: None declared.
References
- 1.Rogers A, Entwistle V, Pencheon D. A patient led NHS: managing demand at the interface between lay and primary care. BMJ 1998;316: 1816-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Pencheon D. Matching demand and supply fairly and efficiently. BMJ 1998;316: 1665-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bunn F, Byrne G, Kendall S. Telephone consultation and triage: effects on health care use and patient satisfaction: Cochrane Database Syst Rev 2004;(4): CD004180. [DOI] [PubMed]
- 4.Roland MO, Bartholomew J, Morrell DC, McDermott A, Paul E. Understanding hospital referral rates: a user's guide. BMJ 1990;301: 98-102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Reynolds GA, Chitnis JG, Roland MO. General practitioner outpatient referrals: do good doctors refer more patients to hospital? BMJ 1991;302: 1250-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Grimshaw JM, Winkens RAG, Shirran L, Cunningham C, Mayhew A, Thomas R, et al. Interventions to improve outpatient referrals from primary care to secondary care. Cochrane Database Syst Rev 2005;(3): CD005471. [DOI] [PubMed]
- 7.Holleran M. Who needs a needs assessment? You do! J Health Care Marketing 1996;16: 32-3. [PubMed] [Google Scholar]
- 8.Gillam S, Pencheon D. Managing demand in general practice. BMJ 1998;316: 1895-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Aish H, Didsbury P, Cressey P, Grigor J, Gribben B. Primary options for acute care: general practitioners using their skills to manage “avoidable admission” patients in the community. N Z Med J 2003;116: U326. [PubMed] [Google Scholar]
- 10.Ruston A. Risk, anxiety and defensive action: general practitioners' referral decisions for women presenting with breast problems. Health, Risk and Society 2004;6: 25-38. [Google Scholar]
- 11.Shaw I, Smith KM, Middleton H, Woodward L. A letter of consequence: referral letters from general practitioners to secondary mental health services. Qual Health Res 2005;15: 116-28. [DOI] [PubMed] [Google Scholar]
- 12.Faulkner A, Mills N, Bainton D, Baxter K, Kinnersley P, Peters T, et al. A systematic review of the effect of primary care-based service innovations on quality and patterns of referral to specialist secondary care. Br J Gen Pract 2003;53: 878-84. [PMC free article] [PubMed] [Google Scholar]
- 13.Improve referral management to reduce specialty utilization. Capitation Manag Rep 1997;4: 140-4. [PubMed] [Google Scholar]
- 14.Cheshire and Merseyside Strategic Health Authority. Local delivery plan 2003-2006. www.cmha.nhs.uk/LDP/ldp03.htm (accessed 20 Mar 2006).
- 15.Hounslow Primary Care Trust. Annual report 2003-4. London: Hounslow Primary Care Trust, 2004.
- 16.Greater Manchester Strategic Health Authority. Annual report 2002-3. http://www.gmsha.nhs.uk/aboutus/annualeport_2003-4.pdf (accessed 20 Mar 2006).
- 17.Somerset Coast Primary Care Trust. Annual report 2003-4. Bridgwater: Somerset Coast Primary Care Trust, 2004.
- 18.Vale of Glamorgan Local Health Board. Referral management centre: strategic overview. Cardiff: Vale of Glamorgan Local Health Board, 2005.
- 19.Department of Health. Choose and book: patient's choice of hospital and booked appointment. London: DoH, 2004.
- 20.BMA. Referral management: frequently asked questions, Jan 2006. www.bma.org.uk/ap.nsf/Content/refmanfaqsjan06?OpenDocument&Login (accessed 23 Mar 2006).
- 21.Oswald N. The history and development of the referral system. In: Roland M, Coulter A, eds. Hospital referrals. Oxford: Oxford University Press, 1992: 15-29.