Abstract
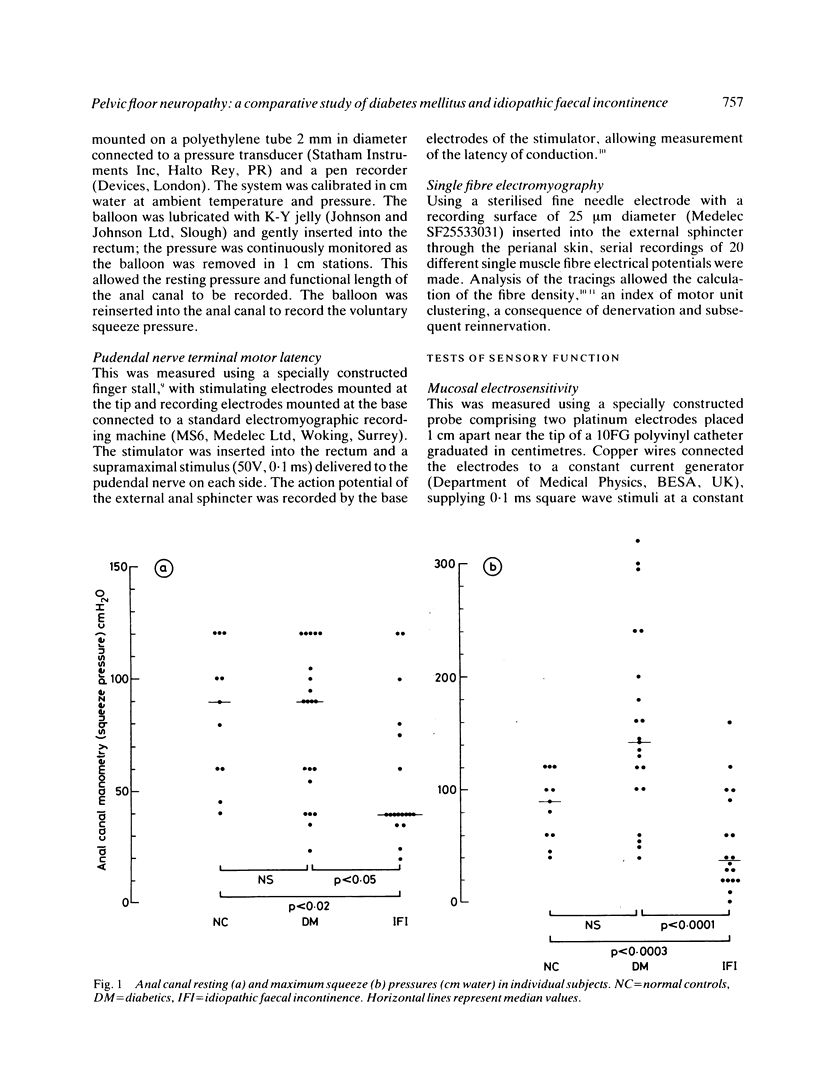
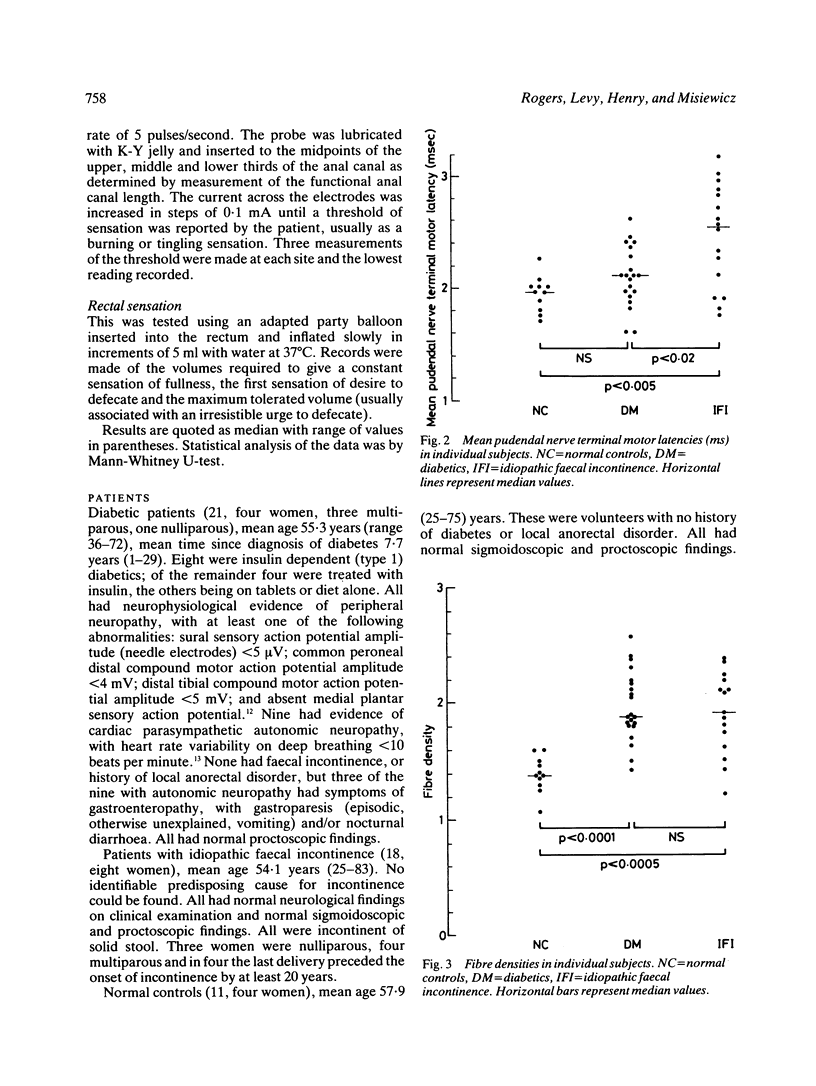
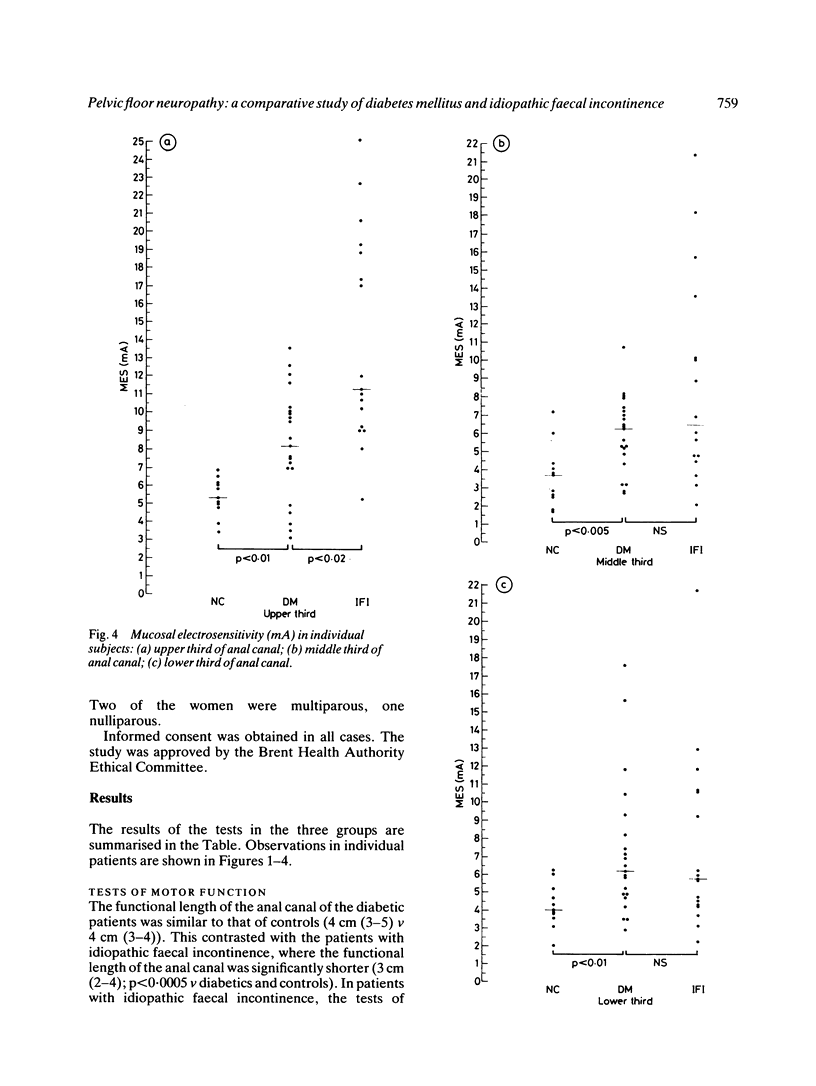
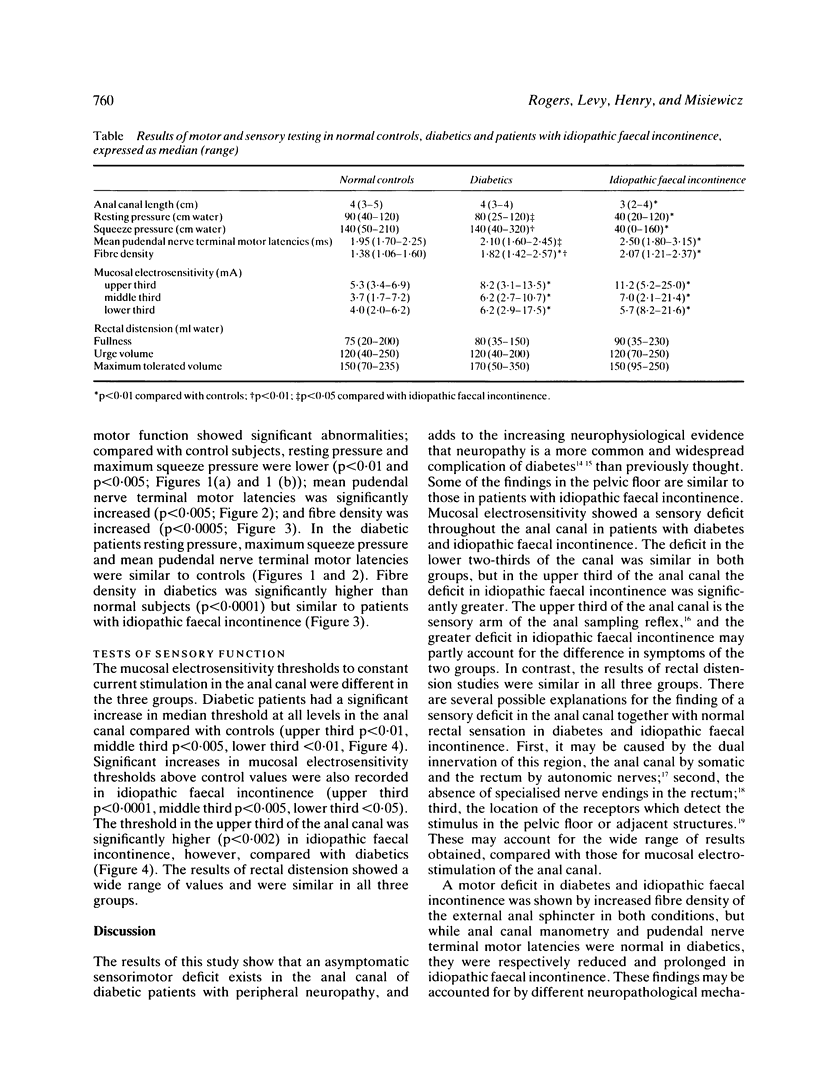
Twenty one patients with diabetic peripheral neuropathy, 18 with idiopathic faecal incontinence and 11 normal controls were studied with techniques of mucosal electrosensitivity, rectal distension for the quantitative assessment of anorectal sensation, and manometric and electromyographic tests for the assessment of anorectal motor function. An asymptomatic sensorimotor deficit was found in the anal canal of patients with diabetic peripheral neuropathy. Mucosal electrosensitivity thresholds in the anal canal were significantly higher (p less than 0.01 v controls) and fibre density of the external anal sphincter significantly raised (p less than 0.0001 v controls). Anal manometry and pudendal nerve terminal motor latencies were similar to controls. In patients with idiopathic faecal incontinence the tests of sensory and motor function also showed a sensorimotor neuropathy; compared with controls, mucosal electrosensitivity thresholds were significantly higher (p less than 0.002), anal canal resting and maximum squeeze pressures were significantly lower (p less than 0.05 and p less than 0.002 respectively), and pudendal nerve terminal motor latencies and fibre density of the external anal sphincter were significantly raised (both p less than 0.05). Sensory thresholds to rectal distension were similar in all groups. Pelvic floor sensorimotor neuropathy in diabetic patients has several features in common with that of patients with idiopathic faecal incontinence but its functional significance remains uncertain.
Full text
PDF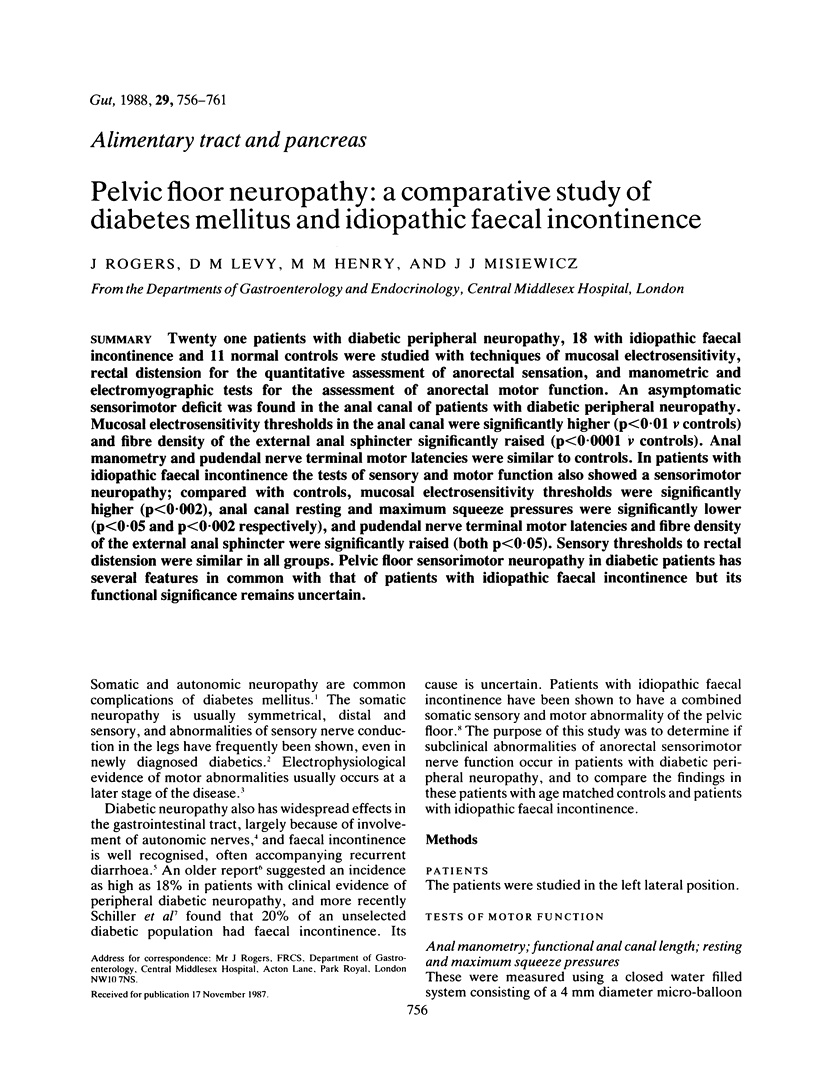
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Abraham R. R., Abraham R. M., Wynn V. Autonomic and electrophysiological studies in patients with signs or symptoms of diabetic neuropathy. Electroencephalogr Clin Neurophysiol. 1986 Mar;63(3):223–230. doi: 10.1016/0013-4694(86)90088-x. [DOI] [PubMed] [Google Scholar]
- DUTHIE H. L., GAIRNS F. W. Sensory nerve-endings and sensation in the anal region of man. Br J Surg. 1960 May;47:585–595. doi: 10.1002/bjs.18004720602. [DOI] [PubMed] [Google Scholar]
- Duthie H. L., Bennett R. C. The relation of sensation in the anal canal to the functional anal sphincter: a possible factor in anal continence. Gut. 1963 Jun;4(2):179–182. doi: 10.1136/gut.4.2.179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ewing D. J., Clarke B. F. Diagnosis and management of diabetic autonomic neuropathy. Br Med J (Clin Res Ed) 1982 Oct 2;285(6346):916–918. doi: 10.1136/bmj.285.6346.916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gupta P. R., Dorfman L. J. Spinal somatosensory conduction in diabetes. Neurology. 1981 Jul;31(7):841–845. doi: 10.1212/wnl.31.7.841. [DOI] [PubMed] [Google Scholar]
- Katz L. A., Spiro H. M. Gastrointestinal manifestations of diabetes. N Engl J Med. 1966 Dec 15;275(24):1350–1361. doi: 10.1056/NEJM196612152752406. [DOI] [PubMed] [Google Scholar]
- Kiff E. S., Swash M. Slowed conduction in the pudendal nerves in idiopathic (neurogenic) faecal incontinence. Br J Surg. 1984 Aug;71(8):614–616. doi: 10.1002/bjs.1800710817. [DOI] [PubMed] [Google Scholar]
- Lamontagne A., Buchthal F. Electrophysiological studies in diabetic neuropathy. J Neurol Neurosurg Psychiatry. 1970 Aug;33(4):442–452. doi: 10.1136/jnnp.33.4.442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lane R. H., Parks A. G. Function of the anal sphincters following colo-anal anastomosis. Br J Surg. 1977 Aug;64(8):596–599. doi: 10.1002/bjs.1800640820. [DOI] [PubMed] [Google Scholar]
- Levy D. M., Abraham R. R., Abraham R. M. Small- and large-fiber involvement in early diabetic neuropathy: a study with the medial plantar response and sensory thresholds. Diabetes Care. 1987 Jul-Aug;10(4):441–447. doi: 10.2337/diacare.10.4.441. [DOI] [PubMed] [Google Scholar]
- MARTIN M. M. Diabetic neuropathy; a clinical study of 150 cases. Brain. 1953;76(4):594–624. doi: 10.1093/brain/76.4.594. [DOI] [PubMed] [Google Scholar]
- Neill M. E., Swash M. Increased motor unit fibre density in the external anal sphincter muscle in ano-rectal incontinence: a single fibre EMG study. J Neurol Neurosurg Psychiatry. 1980 Apr;43(4):343–347. doi: 10.1136/jnnp.43.4.343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rogers J., Henry M. M., Misiewicz J. J. Combined sensory and motor deficit in primary neuropathic faecal incontinence. Gut. 1988 Jan;29(1):5–9. doi: 10.1136/gut.29.1.5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scarpello J. H., Sladen G. E. Diabetes and the gut. Gut. 1978 Dec;19(12):1153–1162. doi: 10.1136/gut.19.12.1153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schiller L. R., Santa Ana C. A., Schmulen A. C., Hendler R. S., Harford W. V., Fordtran J. S. Pathogenesis of fecal incontinence in diabetes mellitus: evidence for internal-anal-sphincter dysfunction. N Engl J Med. 1982 Dec 30;307(27):1666–1671. doi: 10.1056/NEJM198212303072702. [DOI] [PubMed] [Google Scholar]
- Stålberg E., Thiele B. Motor unit fibre density in the extensor digitorum communis muscle. Single fibre electromyographic study in normal subjects at different ages. J Neurol Neurosurg Psychiatry. 1975 Sep;38(9):874–880. doi: 10.1136/jnnp.38.9.874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thiele B., Stålberg E. Single fibre EMG findings in polyneuropathies of different aetiology. J Neurol Neurosurg Psychiatry. 1975 Sep;38(9):881–887. doi: 10.1136/jnnp.38.9.881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Young R. J., Ewing D. J., Clarke B. F. Nerve function and metabolic control in teenage diabetics. Diabetes. 1983 Feb;32(2):142–147. doi: 10.2337/diab.32.2.142. [DOI] [PubMed] [Google Scholar]


