Abstract
The occurrence of Campylobacter pylori (CP) was examined in 179 subjects representing a sample collected from the population of South Finland. In a normal antral and body mucosa CP was present in 5% and 11% and in superficial gastritis (SG) in 71% and 91% of subjects, respectively. In atrophic gastritis (AG) of antrum and body the prevalence of CP decreased significantly with an increasing degree of atrophy, so that CP was not found in severe body AG. Different combinations of antral and body gastritis revealed a characteristic pattern. Campylobacter pylori was lacking when antral and body mucosa were normal, but was present in 41% when normal mucosa was associated with gastritis in the opposite area. In SG affecting diffusely antrum and body, the bacterium was present in every case, but when SG was associated with AG in the opposite area it was lacking in 29% of the subjects. When SG affecting both areas was compared with SG accompanied by different degrees of AG in the body, there was a highly significant decrease of the prevalence of CP in antrum and body along with an increasing degree of AG in the body. This decrease showed a highly significant positive correlation with the acid output. On the whole, acid output correlated well with the occurrence of CP in both antrum and body. Thus the prevalence of CP was 10% in achlorhydria and rose up to 100% in cases with acid output above 30 mmol/h. The presence of CP did not correlate with signs of acute inflammation, but correlated significantly with those of chronic inflammation. No correlation was found in the antrum and a significant negative one in the body, between CP infestation and the extension of intestinal metaplasia. It is concluded that increased pH of gastric contents and mucus secreted by intestinalised glands may create unfavourable conditions for survival of the bacteria and might explain the decrease in the prevalence of CP in the more severe degrees of AG. The present results, however, give no definite answer to the question of the pathogenic significance of CP in the development of chronic gastritis.
Full text
PDF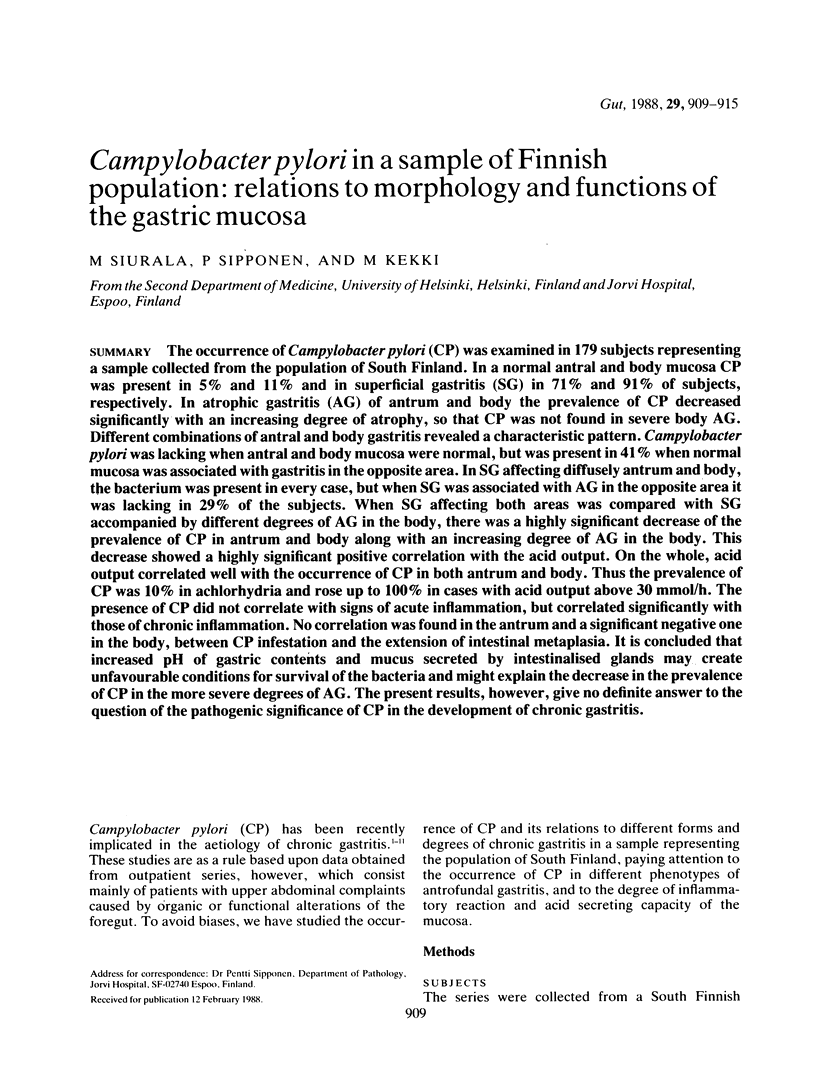





Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Bonney G. E., Elston R. C., Correa P., Haenszel W., Zavala D. E., Zarama G., Collazos T., Cuello C. Genetic etiology of gastric carcinoma: I. Chronic atrophic gastritis. Genet Epidemiol. 1986;3(4):213–224. doi: 10.1002/gepi.1370030402. [DOI] [PubMed] [Google Scholar]
- Booth L., Holdstock G., MacBride H., Hawtin P., Gibson J. R., Ireland A., Bamforth J., DuBoulay C. E., Lloyd R. S., Pearson A. D. Clinical importance of Campylobacter pyloridis and associated serum IgG and IgA antibody responses in patients undergoing upper gastrointestinal endoscopy. J Clin Pathol. 1986 Feb;39(2):215–219. doi: 10.1136/jcp.39.2.215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buck G. E., Gourley W. K., Lee W. K., Subramanyam K., Latimer J. M., DiNuzzo A. R. Relation of Campylobacter pyloridis to gastritis and peptic ulcer. J Infect Dis. 1986 Apr;153(4):664–669. doi: 10.1093/infdis/153.4.664. [DOI] [PubMed] [Google Scholar]
- Campylobacter-like organisms in the stomach of patients and healthy individuals. Lancet. 1984 Jun 16;1(8390):1348–1349. [PubMed] [Google Scholar]
- Gastric spiral bacteria. Lancet. 1984 Jul 14;2(8394):100–101. [PubMed] [Google Scholar]
- Goodwin C. S., Armstrong J. A., Marshall B. J. Campylobacter pyloridis, gastritis, and peptic ulceration. J Clin Pathol. 1986 Apr;39(4):353–365. doi: 10.1136/jcp.39.4.353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gray S. F., Wyatt J. I., Rathbone B. J. Simplified techniques for identifying Campylobacter pyloridis. J Clin Pathol. 1986 Nov;39(11):1279–1279. doi: 10.1136/jcp.39.11.1279-a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ihamäki T., Varis K., Siurala M. Morphological, functional and immunological state of the gastric mucosa in gastric carcinoma families. Comparison with a computer-matched family sample. Scand J Gastroenterol. 1979;14(7):801–812. doi: 10.3109/00365527909181408. [DOI] [PubMed] [Google Scholar]
- Jerzy Glass G. B., Pitchumoni C. S. Structural and ultrastructural alterations, exfoliative cytology and enzyme cytochemistry and histochemistry, proliferation kinetics, immunological derangements and other causes, and clinical associations and sequallae. Hum Pathol. 1975 Mar;6(2):219–250. [PubMed] [Google Scholar]
- Jones D. M., Eldridge J., Whorwell P. J. Antibodies to Campylobacter pyloridis in household contacts of infected patients. Br Med J (Clin Res Ed) 1987 Mar 7;294(6572):615–615. doi: 10.1136/bmj.294.6572.615-a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones D. M., Lessells A. M., Eldridge J. Campylobacter like organisms on the gastric mucosa: culture, histological, and serological studies. J Clin Pathol. 1984 Sep;37(9):1002–1006. doi: 10.1136/jcp.37.9.1002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karttunen T., Niemelä S., Lehtola J., Heikkilä J., Mäentausta O., Räsänen O. Campylobacter-like organisms and gastritis: histopathology, bile reflux, and gastric fluid composition. Scand J Gastroenterol. 1987 May;22(4):478–486. doi: 10.3109/00365528708991494. [DOI] [PubMed] [Google Scholar]
- Marshall B. J., Armstrong J. A., McGechie D. B., Glancy R. J. Attempt to fulfil Koch's postulates for pyloric Campylobacter. Med J Aust. 1985 Apr 15;142(8):436–439. doi: 10.5694/j.1326-5377.1985.tb113443.x. [DOI] [PubMed] [Google Scholar]
- Marshall B. J., McGechie D. B., Rogers P. A., Glancy R. J. Pyloric Campylobacter infection and gastroduodenal disease. Med J Aust. 1985 Apr 15;142(8):439–444. doi: 10.5694/j.1326-5377.1985.tb113444.x. [DOI] [PubMed] [Google Scholar]
- Marshall B. J., Warren J. R. Unidentified curved bacilli in the stomach of patients with gastritis and peptic ulceration. Lancet. 1984 Jun 16;1(8390):1311–1315. doi: 10.1016/s0140-6736(84)91816-6. [DOI] [PubMed] [Google Scholar]
- McLean A. J., Harrison P. M., Ioannides-Demos L. L., Byrne A. J., McCarthy P., Dudley F. J. Microbes, peptic ulcer, and relapse rates with different drugs. Lancet. 1984 Sep 1;2(8401):525–526. doi: 10.1016/s0140-6736(84)92607-2. [DOI] [PubMed] [Google Scholar]
- McNulty C. A., Gearty J. C., Crump B., Davis M., Donovan I. A., Melikian V., Lister D. M., Wise R. Campylobacter pyloridis and associated gastritis: investigator blind, placebo controlled trial of bismuth salicylate and erythromycin ethylsuccinate. Br Med J (Clin Res Ed) 1986 Sep 13;293(6548):645–649. doi: 10.1136/bmj.293.6548.645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McNulty C. A., Watson D. M. Spiral bacteria of the gastric antrum. Lancet. 1984 May 12;1(8385):1068–1069. doi: 10.1016/s0140-6736(84)91469-7. [DOI] [PubMed] [Google Scholar]
- O'Connor H. J., Axon A. T., Dixon M. F. Campylobacter-like organisms unusual in type A (pernicious anaemia) gastritis. Lancet. 1984 Nov 10;2(8411):1091–1091. doi: 10.1016/s0140-6736(84)91523-x. [DOI] [PubMed] [Google Scholar]
- Price A. B., Levi J., Dolby J. M., Dunscombe P. L., Smith A., Clark J., Stephenson M. L. Campylobacter pyloridis in peptic ulcer disease: microbiology, pathology, and scanning electron microscopy. Gut. 1985 Nov;26(11):1183–1188. doi: 10.1136/gut.26.11.1183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rao S. S., Krasner N., Thomson T. J. Chronic gastritis--a simple classification. J Pathol. 1975 Oct;117(2):93–96. doi: 10.1002/path.1711170206. [DOI] [PubMed] [Google Scholar]
- Rathbone B. J., Wyatt J. I., Worsley B. W., Shires S. E., Trejdosiewicz L. K., Heatley R. V., Losowsky M. S. Systemic and local antibody responses to gastric Campylobacter pyloridis in non-ulcer dyspepsia. Gut. 1986 Jun;27(6):642–647. doi: 10.1136/gut.27.6.642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rollason T. P., Stone J., Rhodes J. M. Spiral organisms in endoscopic biopsies of the human stomach. J Clin Pathol. 1984 Jan;37(1):23–26. doi: 10.1136/jcp.37.1.23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sipponen P., Varis K., Cederberg A., Salmi H. A., Seppälä K., Ihamäki T., Kosunen T. U. Campylobacter pylori is associated with chronic gastritis but not with active peptic ulcer disease. APMIS. 1988 Jan;96(1):84–88. doi: 10.1111/j.1699-0463.1988.tb05272.x. [DOI] [PubMed] [Google Scholar]
- Steer H. W. Surface morphology of the gastroduodenal mucosa in duodenal ulceration. Gut. 1984 Nov;25(11):1203–1210. doi: 10.1136/gut.25.11.1203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Strickland R. G., Mackay I. R. A reappraisal of the nature and significance of chronic atrophic gastritis. Am J Dig Dis. 1973 May;18(5):426–440. doi: 10.1007/BF01071995. [DOI] [PubMed] [Google Scholar]
- Tytgat G. N., Rauws E., Langenberg W. The role of colloidal bismuth subcitrate in gastric ulcer and gastritis. Scand J Gastroenterol Suppl. 1986;122:22–29. doi: 10.3109/00365528609102582. [DOI] [PubMed] [Google Scholar]
- Wyatt J. I., Rathbone B. J., Dixon M. F., Heatley R. V. Campylobacter pyloridis and acid induced gastric metaplasia in the pathogenesis of duodenitis. J Clin Pathol. 1987 Aug;40(8):841–848. doi: 10.1136/jcp.40.8.841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- von Wulffen H., Heesemann J., Bützow G. H., Löning T., Laufs R. Detection of Campylobacter pyloridis in patients with antrum gastritis and peptic ulcers by culture, complement fixation test, and immunoblot. J Clin Microbiol. 1986 Nov;24(5):716–720. doi: 10.1128/jcm.24.5.716-720.1986. [DOI] [PMC free article] [PubMed] [Google Scholar]


