Abstract
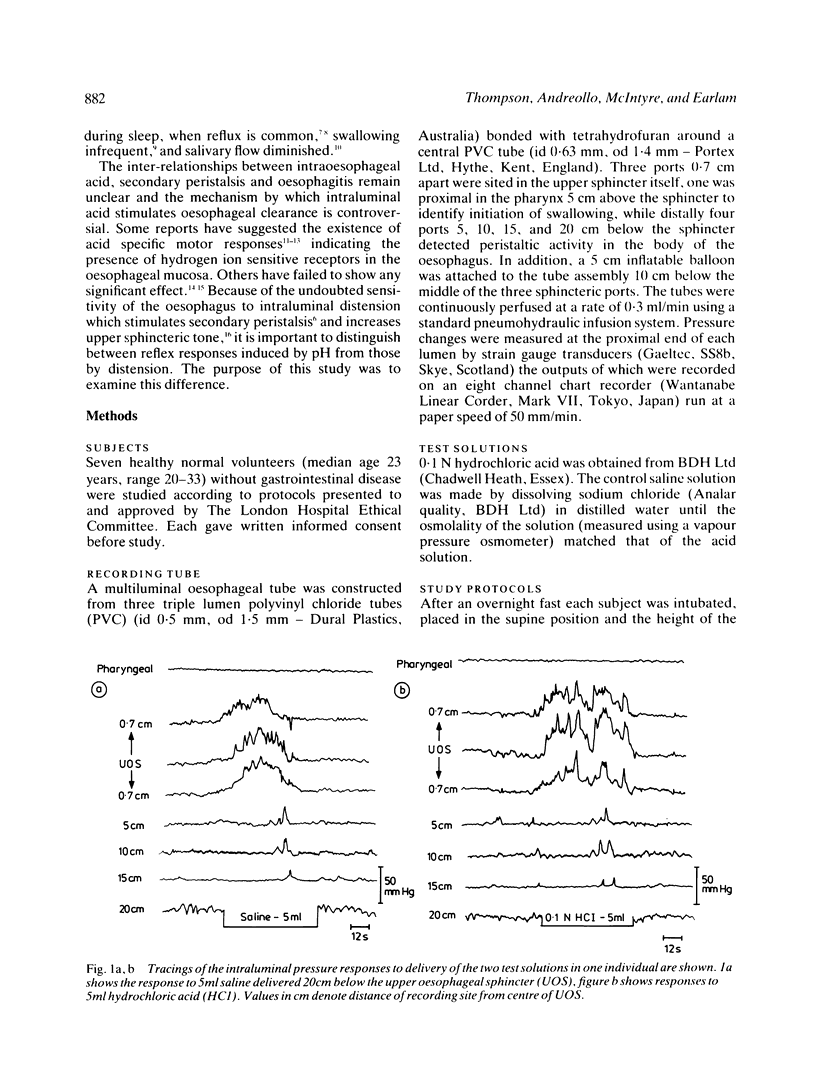
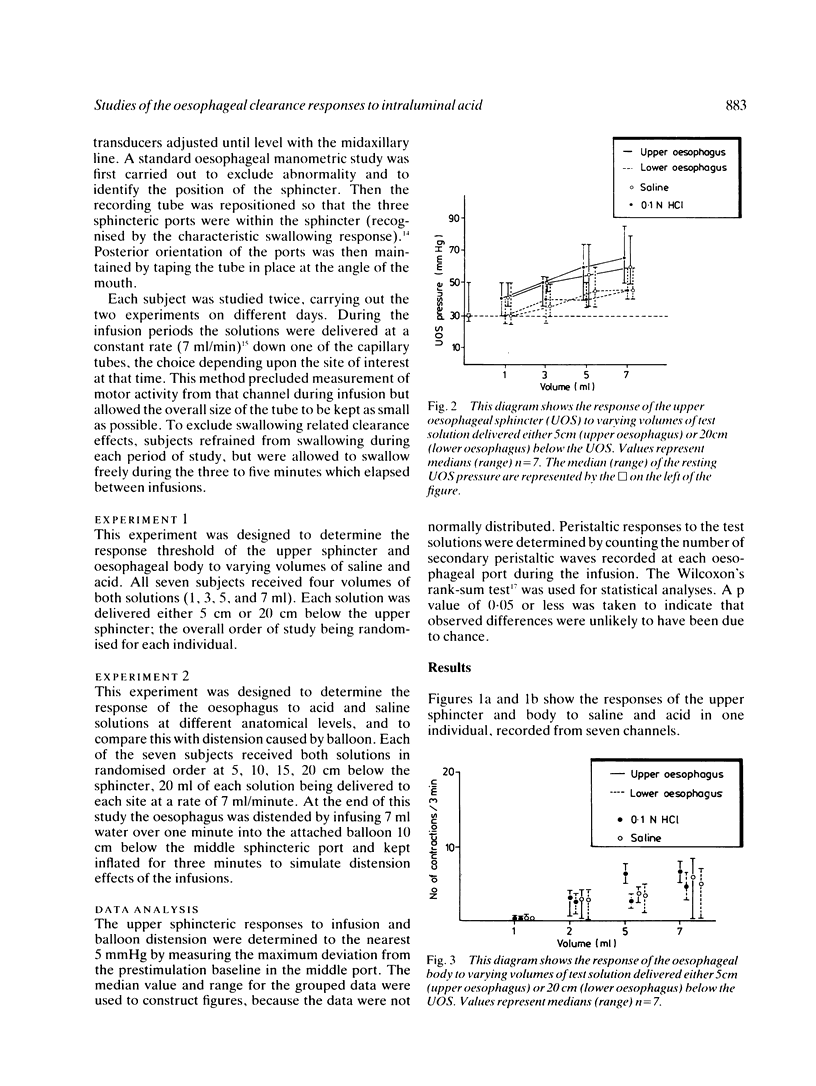
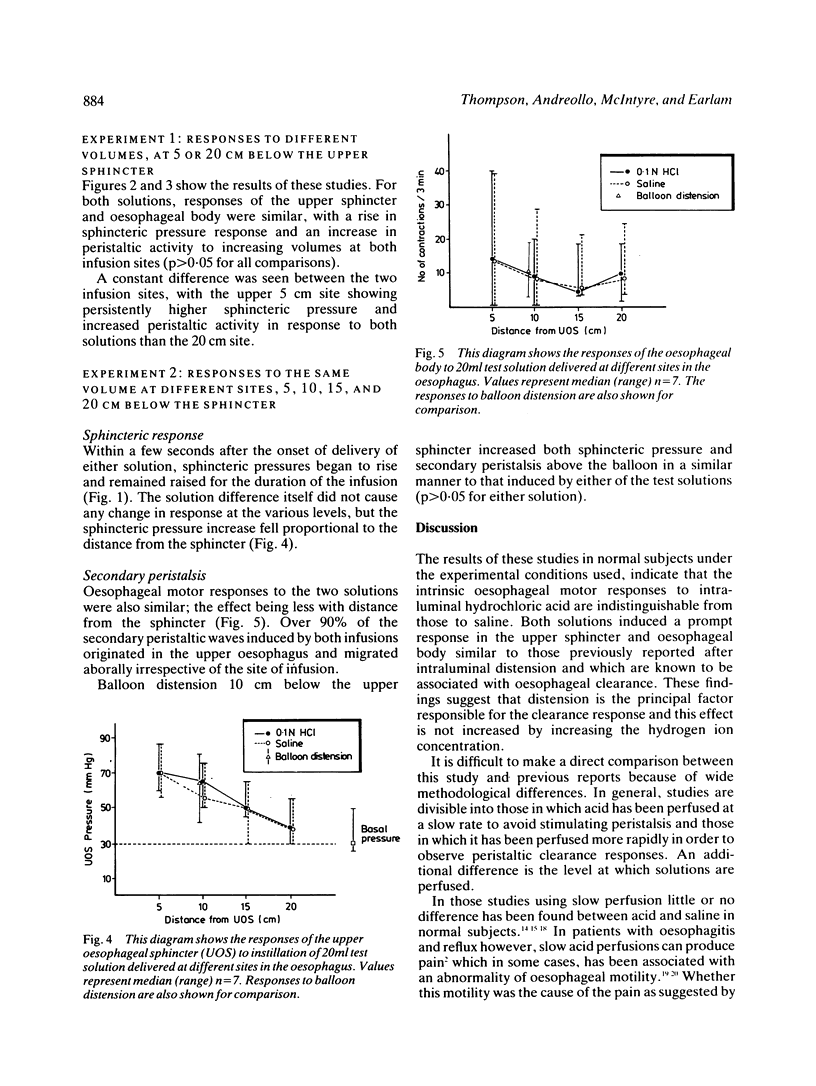
Contraction of the upper oesophageal sphincter combined with secondary peristalsis clears the oesophagus of refluxed gastric contents and protects the trachea, but the nature of these reflex stimuli remains controversial. Secondary peristaltic and sphincteric responses were measured during intraluminal infusion of 0.1 N hydrochloric acid and equiosmolar saline solutions in seven normal volunteers. Responses to a single volume infused at varying sites in the oesophagus and to progressively increasing volumes of test solution were measured. In addition oesophageal responses to similar degrees of distension induced by inflation of an intraluminal balloon were also recorded. The sphincteric responses to both stimuli were similar, decreasing in value with distance from the sphincter from values of 70 (68-85) mmHg (median (range] for HCl; and 70 (55-85) mmHg for NaCl at 5 cm below the sphincter to 40 (30-60) mmHg for both HCl and NaCl at 20 cm. As the volume of the solution infused into the proximal oesophagus was increased, the sphincter pressure also rose from a median basal value of 30 (25-50) mmHg to 40 (30-50) mmHg for HCl and NaCl after 1 ml, while after 7 ml infusion, the responses were greater, 65 (45-85) mmHg for HCl, and 60 (45-80) mmHg for NaCl. In the more distal oesophagus, responses were qualitatively similar but quantitatively smaller than proximally, being 30 (25-40) mmHg for HCl and 30 (25-50) mmHg for NaCl following 1 ml and 45 (40-55) mmHg for HCl and NaCl after 7 ml. Secondary peristalsis was also induced equally by both solutions and varied with volumes infused and site of infusion in a manner similar to the sphincter responses. After a 7 ml/min acid infusion 14 (1- 40) secondary contractions/three min were recorded at 5 cm and eight (2 - 18)/three min were recorded at 20 cm. Values for saline were similar, 13 (1- 38)/three min at 5 cm and eight (4 - 25)/three min at 20 cm. Oesophageal distension by a balloon positioned 10 cm below the sphincter induced identical clearance responses to those seen after similar volumes of either acid or saline infused at the same site. These results suggest that the principal stimulus for upper oesophageal clearance is intraluminal distension and do not support the idea that the oesophagus is pH sensitive.
Full text
PDF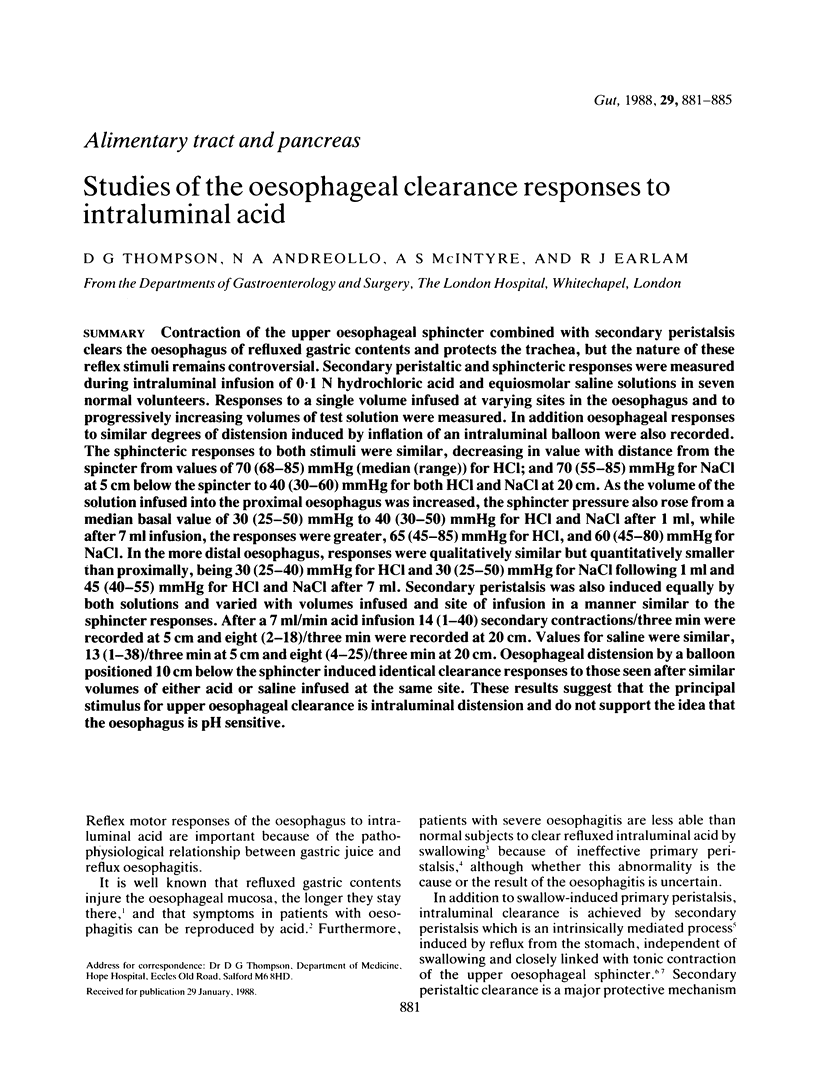
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- BERNSTEIN L. M., BAKER L. A. A clinical test for esophagitis. Gastroenterology. 1958 May;34(5):760–781. [PubMed] [Google Scholar]
- Burns T. W., Venturatos S. G. Esophageal motor function and response to acid perfusion in patients with symptomatic reflux esophagitis. Dig Dis Sci. 1985 Jun;30(6):529–535. doi: 10.1007/BF01320258. [DOI] [PubMed] [Google Scholar]
- Christensen J., Lund G. F. Esophageal responses to distension and electrical stimulation. J Clin Invest. 1969 Feb;48(2):408–419. doi: 10.1172/JCI105998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Christensen J. Origin of sensation in the esophagus. Am J Physiol. 1984 Mar;246(3 Pt 1):G221–G225. doi: 10.1152/ajpgi.1984.246.3.G221. [DOI] [PubMed] [Google Scholar]
- Corazziari E., Pozzessere C., Dani S., Anzini F., Torsoli A. Intraluminal pH esophageal motility. Gastroenterology. 1978 Aug;75(2):275–277. [PubMed] [Google Scholar]
- Freiman J. M., El-Sharkawy T. Y., Diamant N. E. Effect of bilateral vagosympathetic nerve blockade on response of the dog upper esophageal sphincter (UES) to intraesophageal distention and acid. Gastroenterology. 1981 Jul;81(1):78–84. [PubMed] [Google Scholar]
- Gerhardt D. C., Shuck T. J., Bordeaux R. A., Winship D. H. Human upper esophageal sphincter. Response to volume, osmotic, and acid stimuli. Gastroenterology. 1978 Aug;75(2):268–274. [PubMed] [Google Scholar]
- Goldberg H. I., Dodds W. J., Gee S., Montgomery C., Zboralske F. F. Role of acid and pepsin in acute experimental esophagitis. Gastroenterology. 1969 Feb;56(2):223–230. [PubMed] [Google Scholar]
- Kahrilas P. J., Dodds W. J., Hogan W. J., Kern M., Arndorfer R. C., Reece A. Esophageal peristaltic dysfunction in peptic esophagitis. Gastroenterology. 1986 Oct;91(4):897–904. doi: 10.1016/0016-5085(86)90692-x. [DOI] [PubMed] [Google Scholar]
- Kendall G. P., Thompson D. G., Day S. J., Garvie N. Motor responses of the oesophagus to intraluminal distension in normal subjects and patients with oesophageal clearance disorders. Gut. 1987 Mar;28(3):272–279. doi: 10.1136/gut.28.3.272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lichter I., Muir R. C. The pattern of swallowing during sleep. Electroencephalogr Clin Neurophysiol. 1975 Apr;38(4):427–432. doi: 10.1016/0013-4694(75)90267-9. [DOI] [PubMed] [Google Scholar]
- Olsen A. M., Schlegel J. F. Motility disturbances caused by esophagitis. J Thorac Cardiovasc Surg. 1965 Nov;50(5):607–612. [PubMed] [Google Scholar]
- Orr W. C., Robinson M. G., Johnson L. F. Acid clearance during sleep in the pathogenesis of reflux esophagitis. Dig Dis Sci. 1981 May;26(5):423–427. doi: 10.1007/BF01313584. [DOI] [PubMed] [Google Scholar]
- SCHNEYER L. H., PIGMAN W., HANAHAN L., GILMORE R. W. Rate of flow of human parotid, sublingual, and submaxillary secretions during sleep. J Dent Res. 1956 Feb;35(1):109–114. doi: 10.1177/00220345560350010301. [DOI] [PubMed] [Google Scholar]
- SIEGEL C. I., HENDRIX T. R. Esophageal motor abnormalities induced by acid perfusion in patients with heartburn. J Clin Invest. 1963 May;42:686–695. doi: 10.1172/JCI104760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stanciu C., Bennett J. R. Oesophageal acid clearing: one factor in the production of reflux oesophagitis. Gut. 1974 Nov;15(11):852–857. doi: 10.1136/gut.15.11.852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stanciu C., Bennett J. R. Upper oesophageal sphincter yield pressure in normal subjects and in patients with gastro-oesophageal reflux. Thorax. 1974 Jul;29(4):459–462. doi: 10.1136/thx.29.4.459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wallin L., Boesby S., Madsen T. The effect of HCl infusion in the lower part of the oesophagus on the pharyngo-oesophageal sphincter pressure in normal subjects. Scand J Gastroenterol. 1978;13(7):821–826. doi: 10.3109/00365527809182197. [DOI] [PubMed] [Google Scholar]


