Abstract
Indole-3-carbinol (I3C) is a phytochemical (derived from broccoli, cabbage, and other cruciferous vegetables) with proven anticancer efficacy including the reduction of cervical intraepithelial neoplasia (CIN) and its progression to cervical cancer. In a breast cancer cell line, I3C inhibited cell adhesion, spreading, and invasion associated with an upregulation of the tumor suppressor gene PTEN, suggesting that PTEN is important in inhibition of late stages in the development of cancer. The goal of this study was to determine the expression of PTEN during the development of cervical cancer and whether I3C affected expression of PTEN in vivo. We show diminished PTEN expression during the progression from low-grade to high-grade cervical dysplasia in humans and in a mouse model for cervical cancer, the K14HPV16 transgenic mice promoted with estrogen. The implication is that loss of PTEN function is required for this transition. Additionally, dietary I3C increased PTEN expression in the cervical epithelium of the transgenic mouse, an observation that suggests PTEN upregulation by I3C is one mechanism by which I3C inhibits development of cervical cancer.
INTRODUCTION
Indole-3-carbinol (I3C) is a promising cancer-preventive phytochemical found abundantly in cruciferous vegetables, such as broccoli and Brussels sprouts. In animal models, I3C prevents the development of a plethora of malignancies, including cervical cancer (1), breast cancer (2), prostate cancer (3), endometrial cancer (4), and skin cancer (5). Diindolylmethane (DIM), the congener of I3C formed in the stomach, alters the expression of many genes (6). As a result, I3C alters estrogen signaling (7–9), inactivates many carcinogens (10,11), causes growth arrest (12–14), induces the endoplasmic reticulum response (15), and induces apoptosis (16,17). Relevant to this study with PTEN, it is clear that I3C inactivates Akt in tumor cells (18,19).
The ability of I3C to upregulate the tumor suppressor PTEN is controversial, however. Meng et al. (20) reported that I3C upregulated PTEN in T47-D human breast cancer cells, whereas Howells et al. (21) observed no change of PTEN levels in response to I3C in a different breast cancer cell line. We therefore sought to determine the effect of I3C on PTEN in relation to I3C’s ability to prevent the development of cervical cancer in vivo.
Cervical cancer and precancerous lesions are well characterized (for example, hyperplasia, low-grade dysplasia, high-grade dysplasia [with intermediate gradations], and cancer). Additionally, a mouse model with HPV transgenes (cofactor for cervical cancer) develops cervical cancer when given estrogen chronically (22). The mouse’s development of cervical cancer resembles the development of cervical abnormalities and progression to cancer as seen in humans (1,22). I3C prevents cervical cancer in this mouse model (1) and has efficacy in the treatment of cervical dysplasia in both mice and humans (1,23).
Mutations in PTEN are common in many human cancers (24–26) but not in cervical cancer (27–29); however, inactivation by methylation of the promoter does occur (30–33). PTEN is a dual-specificity phosphatase capable of dephosphorylating phospholipids as well as phosphoproteins (34). The in vivo lipid substrate of PTEN is believed to be phosphatidylinositol-3,4,5-triphosphate (PIP3) (35), a PI3 kinase product that recruits Akt to the plasma membrane (36,37) where it is phosphorylated by the activating kinases PDK1 (38) and PDK2/ILK (39,40). The C3-specific lipid phosphatase activity of PTEN generates PIP2. PTEN, therefore, is a negative regulator of the Akt branch of PI3 kinase pathway (41). Negative regulation of Akt signaling by PTEN decreases both the level and the nuclear localization of cyclin D1, thereby markedly reducing Rb phosphorylation and increasing cell-cycle arrest at G1 (42). Reducing Akt signaling by PTEN also activates the Forkhead family of transcription factors (43) as well as Bad (44); both are pro-death regulators. As a protein phosphatase, PTEN mediates, either directly or indirectly, the dephosphorylation, and hence the inactivation, of phosphoSTAT3 (45). Other phosphoprotein substrates for PTEN include focal adhesion kinase (FAK) and adaptor protein Shc (46). As PTEN functions to tilt survival/death toward the pro-death side, the consequence of inactivating PTEN is tumor promotion, and the consequence of increasing functional PTEN expression is tumor suppression.
In this study, we demonstrated the loss of PTEN during the development of cervical cancer in humans and in a mouse model of cervical cancer. We show that dietary I3C upregulated PTEN in the mouse model.
MATERIALS AND METHODS
Human Tissues
Archived human specimens from patients with condyloma, varying degrees of cervical intraepithelial neoplasia (CIN), and cervical cancer were from the pathology archive of Long Island Jewish Medical Center. Use of these surgical discards—paraffin-embedded fixed specimens from patients diagnosed with condyloma, low-grade dysplasia, high-grade dysplasia, and invasive squamous carcinoma (more than 20 in each category)—was approved by the Institutional Review Board of the North Shore Long Island Jewish Health System.
Mouse Tissues
Archived mouse specimens were from a study that compared the K14HPV16 transgenic mice and its nontransgenic littermates given control diet or diet supplemented with 2000 ppm I3C (1). Briefly, 5-month-old female mice were given slow release of 17β-estradiol at a dosage of 0.125 mg subcutaneously every 60 days to promote cervical dysplasia. Groups received AIN76a diet with or without I3C from 5 weeks to 7 months of age. Additional paraffin-embedded fixed specimens were from mice at each stage of CIN. The study had the approval of the Institutional Animal Care and Use Committee at Long Island Jewish Medical Center.
Evaluation of Specimens for PTEN
Serial sections (5 μm) were prepared, and pathology was evaluated using H&E-stained sections. Immunohistochemistry was used to visualize PTEN. Briefly, sections were air-dried overnight, rehydrated with graded alcohol and PBS, and treated with 0.1% H2O2 and 20 μg/mL proteinase K to block endogenous peroxidase activity and to expose antigens. Horse serum (1.5% in PBS) was used to block nonspecific antibody binding. PTEN monoclonal antibody A2B1 (Santa Cruz) was used at a dilution of 1:100. Immunoreactivity was detected using the Vectastain ABC system (Vector Laboratories). These slides were evaluated by each investigator, including 2 pathologists and 2 others.
Quantitative Evaluation for PTEN
The relative intensity of staining of PTEN in a measured section representing the full width of the epithelium (equivalent to that of the images shown) was performed using Image-Pro Plus 5.0 software (Media Cybernetics, Silver Springs, MD, USA). Briefly, a defined measured area from a ×400 magnification image was displayed in Adobe Photoshop, and the intensity of the staining was evaluated. Imaging was performed on a subset of tissues (minimum of 3) picked at random based on pathology. Immunohistochemistry processing was performed at the same time in these subsets to ensure comparable staining between tissues. Statistical analysis used Student t test.
RESULTS
PTEN Expression Decreases as Cervical Dysplasia Increases and Is Absent in Cervical Cancer
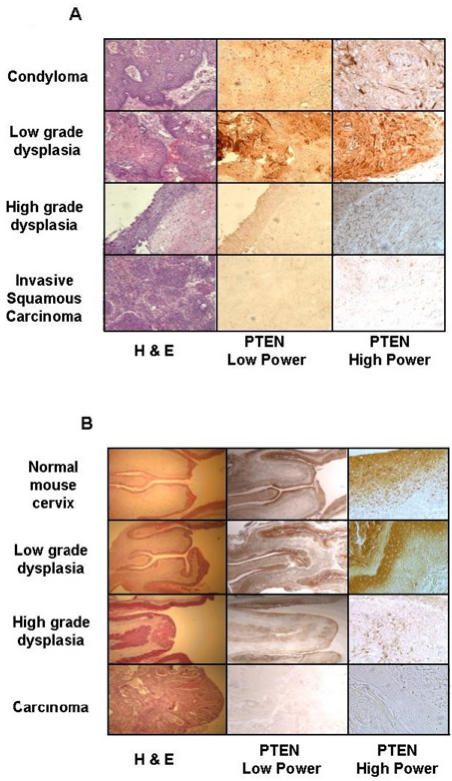
To gain insight into the role of PTEN in the development of cervical cancer, we followed its expression in the development of cervical cancer. We evaluated PTEN in various cervical abnormalities including cervical cancer samples obtained from humans. As shown in Figure 1A, cells from condylomata (genital warts or benign tumors caused by infection with an HPV, having very low potential of becoming cancer) expressed PTEN. This observation is consistent with previous findings in similar lesions caused by low-risk HPVs in the larynx (45). Similarly, cells in low-grade cervical dysplasia were PTEN-positive. In contrast, little or no PTEN was detected in cells in high-grade cervical dysplasia or in invasive squamous cell carcinoma. This observation indicated that elimination of PTEN expression was associated with progression from low-grade to high-grade cervical dysplasia, a transition when increased angiogenesis is required (47–50).
Figure 1.
Inhibition of PTEN expression during the development of cervical cancer in humans and in HPV16 transgenic mice. (A) Human condyloma, low-grade cervical dysplasia, high-grade cervical dysplasia, and cervical carcinoma specimens were stained with H&E or immunostained by PTEN monoclonal antibody A2B1 (PTEN) and visualized under low-power (×100) or high-power (×400) magnification. (B) Tissue sections of normal, low-grade dysplasia, high-grade dysplasia, and carcinoma from HPV16 transgenic mice were stained and visualized as in panel A. Images are representative of more than 20 specimens per group.
More exact conclusions can be made with lesions found in the K14HPV16 transgenic mouse, the murine model for human cervical cancer, because of its genetic homogeneity. As shown in Figure 1B, cells in normal cervical epithelium or in low-grade dysplasia expressed PTEN, whereas expression of PTEN was mostly undetectable when the dysplasia progressed to high grade or to carcinoma. These observations validated results seen in human lesions and supported our hypothesis that reduction in PTEN expression was required for transition from low-grade to high-grade dysplasia.
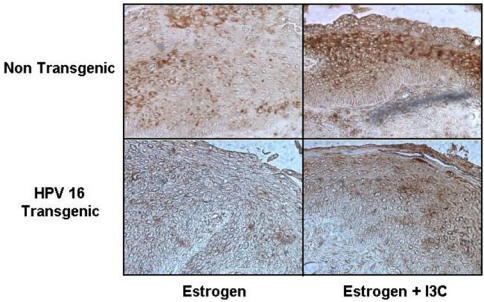
I3C Promotes PTEN Expression in K14HPV16 Transgenic Mice
I3C suppresses the formation of cervical cancer in K14 HPV16 mice (1). Additionally, I3C greatly reduced the incidence of progression to high-grade dysplasia in the background mouse given estradiol (1). More specifically, downstream products of I3C, such as diindolylmethane, formed in the stomach or tissue culture would be responsible for its effects. This observation led to the belief that I3C may exert its antitumor effects, at least in part, by increasing the expression of PTEN, an observation in breast cancer cells in vitro (20). Our evaluations used tissue from 7-month-old mice that had been fed diets with and without I3C from age 5 weeks. Figure 2 demonstrated that expression of PTEN was upregulated in cervical tissue from both the background mouse and the HPV16 transgenic mouse.
Figure 2.
I3C promotes PTEN expression in HPV16 transgenic mice. HPV-16 transgenic mice and their nontransgenic littermates were given slow-release estrogen to promote dysplasia and fed diets with or without I3C. Cervix sections were prepared and immunostained with PTEN monoclonal antibody A2B1. Controls (no I3C treatment) are high-grade dysplasia. Specimens from the I3C-treated groups are age-matched. Images are representative of 20 per category. Magnification ×100 and ×400.
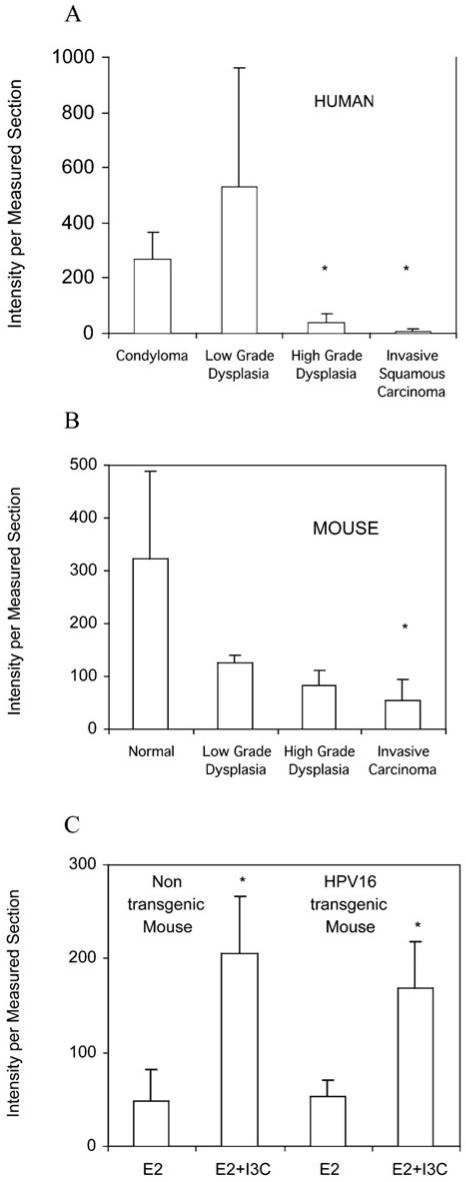
Quantitative determinations more precisely confirmed our observations. Imaging of the human sections, using immunohistochemistry for staining, indicated that very little PTEN was in the high-grade dysplasias or carcinomas in both human and mouse tissues (Figure 3A and B). In the mouse tissue, diminishing PTEN occurred as the cervical disease stages progressed from normal to low-grade dysplasia to high-grade dysplasia to carcinoma. In the mouse, the amount of PTEN was more variable in the normal cervical tissue than in any of the abnormal tissues. The P values comparing the reduced amount of PTEN to normal was significant for the carcinoma (P = 0.04) but not for low-grade dysplasia (P = 0.08) or high-grade dysplasia (P = 0.09), although the trend is clear. Because tissues without pathology (normal) were not available for human samples, the amount of PTEN in high-grade dysplasia and invasive carcinomas was compared with the benign tumors (condylomas). P values were highly significant: 0.02 and 0.01 for high-grade lesions and cancers, respectively.
Figure 3.
Quantitation confirms inhibition of PTEN expression during development of cervical cancer, and I3C increases PTEN expression. Imaging and quantitation of PTEN immunohistochemistry were done on a minimum of 3 tissues per group for cervix specimens from humans (A) and mice (B) with varying degrees of pathology. Quantitation of PTEN (C) was performed on specimens from nontransgenic and K14HPV16 transgenic mice treated with estradiol (E2) and diets with and without I3C from 5 weeks to 7 months of age. *P ≤ 0.05.
Evaluations (Figure 3C) of mice treated long term with estradiol and diets with or without I3C indicated that mice treated with I3C had significantly more PTEN. The P values comparing PTEN in the mice treated with I3C were 0.009 and 0.011 for the background mouse and the HPV16 transgenic mouse, respectively.
The timing of the upregulation of PTEN—i.e., the transition from low-grade dysplasia to high-grade dysplasia (most evident in the human specimens)—coincides with the timing when angiogenesis occurs in the K14HPV16 mouse not treated with I3C (50). Consistently, the I3C congener diindolylmethane (formed from I3C in the stomach) inhibited angiogenesis in a transplantable human breast carcinoma (51).
DISCUSSION
In our in vivo study, PTEN is diminished during the transition from a low-grade to a high-grade dysplasia. I3C prevents this loss of PTEN and appears to increase its expression.
As a tumor suppressor, PTEN is often inactivated during tumorigenesis, thereby giving progeny tumor cells growth and survival advantages. In endometrial cancer, PTEN is mutated with high probability (30% to 50%) (26,27). In cervical cancer, however, genetic alteration that obliterates PTEN’s activity appears to be a rare event (28,29). Instead, elimination of PTEN expression is achieved in epigenetic ways, such as promoter methylation (32,33). I3C has been shown to inhibit tumor development from low-grade to high-grade dysplasia (1), a process that accompanies the downregulation of PTEN, in the K14HPV16 transgenic mouse model of cervical cancer. This is consistent with the present finding that I3C upregulates PTEN. Our results also suggest that the ability of I3C to upregulate PTEN contributes to its ability to prevent cervical carcinoma.
PTEN could retard tumor progression by inhibiting proliferation and by increasing tumor cell apoptosis. This is supported by our previous findings that I3C decreased proliferating cell nuclear antigen (PCNA)-positive cells (1) and increased TdT-mediated dUTP nick-end labeling (TUNEL)-positive cells (16) in abnormal cervical epithelium of HPV16 mice. PTEN is a known negative regulator of angiogenesis (52). Inhibition of angiogenesis by PTEN can be mediated by reducing the level of activated Akt or STAT3, which leads to diminished transactivation of the VEGF promoter (53). Vascularization has been shown in many in vivo systems to be crucial for tumor progression. Reducing neovasculature restrains tumor growth, and increasing microvasculature is associated with progression from low-grade to high-grade CIN and to cervical carcinoma in humans (47,48,54) as well as in estrogen-induced dysplasia in mice (1). This is also consistent with our result in that I3C induces PTEN and retards progression to high-grade dysplasia.
The mechanism by which I3C upregulates PTEN is unknown. I3C is a phytoestrogen that can bind to the estrogen receptor and in some cases be an agonist (55), albeit it functions as an antiestrogen in the presence of estrogen by both competing with estrogen for the estrogen receptor (9) and altering estrogen metabolism (7). Other phytoestrogens, for example, genistein, have been shown to increase PTEN message (56). Genistein reverses hypermethylation, resulting in reactivation of methylation-silenced genes (57). Thus promoter demethylation of PTEN by I3C, which would be very relevant for cervical cancer, might be proposed as a mechanism. Another possibility is the upregulation of Egr-1, a transcription factor known to positively regulate PTEN expression (58).
As inactivation of PTEN has been implicated in a variety of cancers, upregulation of PTEN by I3C should be beneficial in the prevention and adjunctive therapy of a significant number of cancers. Mutations in PTEN resulting in a dysfunctional protein would negate this benefit. Nonetheless, I3C should be helpful in increasing PTEN levels that result from its underexpression due to a hemizygous deletion or hypermethylation.
Acknowledgments
This study is supported by NCI grant R01CA73385 to K.A.
Footnotes
Online address: http://www.molmed.org
REFERENCES
- 1.Jin L, et al. Indole-3-carbinol prevents cervical cancer in human papilloma virus type 16 (HPV16) transgenic mice. Cancer Res. 1999;59:3991–7. [PubMed] [Google Scholar]
- 2.Grubbs CJ, et al. Chemoprevention of chemically-induced mammary carcinogenesis by indole-3-carbinol. Anticancer Res. 1995;15:709–16. [PubMed] [Google Scholar]
- 3.Garikapaty VP, et al. Anti-carcinogenic and anti-metastatic properties of indole-3-carbinol in prostate cancer. Oncol Rep. 2005;13:89–93. [PubMed] [Google Scholar]
- 4.Kojima T, Tanaka T, Mori H. Chemoprevention of spontaneous endometrial cancer in female Donryu rats by dietary indole-3-carbinol. Cancer Res. 1994;54:1446–9. [PubMed] [Google Scholar]
- 5.Srivastava B, Shukla Y. Antitumour promoting activity of indole-3-carbinol in mouse skin carcinogenesis. Cancer Lett. 1998;134:91–5. doi: 10.1016/s0304-3835(98)00247-x. [DOI] [PubMed] [Google Scholar]
- 6.Carter TH, et al. Diindolylmethane alters gene expression in human keratinocytes in vitro. J Nutr. 2002;132:3314–24. doi: 10.1093/jn/132.11.3314. [DOI] [PubMed] [Google Scholar]
- 7.Jellinck PH, et al. Ah receptor binding properties of indole carbinols and induction of hepatic estradiol hydroxylation. Biochem Pharmacol. 1993;45:1129–36. doi: 10.1016/0006-2952(93)90258-x. [DOI] [PubMed] [Google Scholar]
- 8.Chen I, McDougal A, Wang F, Safe S. Aryl hydrocarbon receptor-mediated antiestrogenic and antitumorigenic activity of diindolylmethane. Carcinogenesis. 1998;19:1631–9. doi: 10.1093/carcin/19.9.1631. [DOI] [PubMed] [Google Scholar]
- 9.Auborn KJ, et al. Indole-3-carbinol is a negative regulator of estrogen. J Nutr. 2003;133:2470S–5S. doi: 10.1093/jn/133.7.2470s. [DOI] [PubMed] [Google Scholar]
- 10.Nho CW, Jeffery E. The synergistic upregulation of phase II detoxification enzymes by glucosinolate breakdown products in cruciferous vegetables. Toxicol Appl Pharmacol. 2001;174:146–52. doi: 10.1006/taap.2001.9207. [DOI] [PubMed] [Google Scholar]
- 11.Aggarwal BB, Ichikawa H. Molecular targets and anticancer potential of indole-3-carbinol and its derivatives. Cell Cycle. 2005;4:1201–15. doi: 10.4161/cc.4.9.1993. [DOI] [PubMed] [Google Scholar]
- 12.Cover CM, et al. Indole-3-carbinol inhibits the expression of cyclin-dependent kinase-6 and induces a G1 cell cycle arrest of human breast cancer cells independent of estrogen receptor signaling. J Biol Chem. 1998;273:3838–47. doi: 10.1074/jbc.273.7.3838. [DOI] [PubMed] [Google Scholar]
- 13.Cram EJ, Liu BD, Bjeldanes LF, Firestone GL. Indole-3-carbinol inhibits CDK6 expression in human MCF-7 breast cancer cells by disrupting Sp1 transcription factor interactions with a composite element in the CDK6 gene promoter. J Biol Chem. 2001;276:22332–40. doi: 10.1074/jbc.M010539200. [DOI] [PubMed] [Google Scholar]
- 14.Hong C, Kim HA, Firestone GL, Bjeldanes LF. 3,3′-Diindolylmethane (DIM) induces a G(1) cell cycle arrest in human breast cancer cells that is accompanied by Sp1-mediated activation of p21(WAF1/CIP1) expression. Carcinogenesis. 2002;23:1297–1305. doi: 10.1093/carcin/23.8.1297. [DOI] [PubMed] [Google Scholar]
- 15.Sun S, et al. Endoplasmic reticulum stress as a correlate of cytotoxicity in human tumor cells exposed to diindolylmethane in vitro. Cell Stress Chaperones. 2004;9:76–87. doi: 10.1379/CSC-2R.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Chen DZ, Qi M, Auborn KJ, Carter TH. Indole-3-carbinol and diindolyl-methane induce apoptosis of human cervical cancer cells and in murine HPV16-transgenic preneoplastic cervical epithelium. J Nutr. 2001;131:3294–302. doi: 10.1093/jn/131.12.3294. [DOI] [PubMed] [Google Scholar]
- 17.Bonnesen C, Eggleston IM, Hayes JD. Dietary indoles and isothiocyanates that are generated from cruciferous vegetables can both stimulate apoptosis and confer protection against DNA damage in human colon cell lines. Cancer Res. 2001;61:6120–30. [PubMed] [Google Scholar]
- 18.Rahman KM, Li Y, Sarkar FH. Inactivation of akt and NF-kappaB play important roles during indole-3-carbinol-induced apoptosis in breast cancer cells. Nutr Cancer. 2004;48:84–94. doi: 10.1207/s15327914nc4801_12. [DOI] [PubMed] [Google Scholar]
- 19.Chinni SR, Sarkar FH. Akt inactivation is a key event in indole-3-carbinol-induced apoptosis in PC-3 cells. Clin Cancer Res. 2002;8:1228–36. [PubMed] [Google Scholar]
- 20.Meng Q, Goldberg ID, Rosen EM, Fan S. Inhibitory effects of Indole-3-carbinol on invasion and migration in human breast cancer cells. Breast Cancer Res Treat. 2000;63:147–52. doi: 10.1023/a:1006495824158. [DOI] [PubMed] [Google Scholar]
- 21.Howells LM, Gallacher-Horley B, Houghton CE, Manson MM, Hudson EA. Indole-3-carbinol inhibits protein kinase B/Akt and induces apoptosis in the human breast tumor cell line MDA MB468 but not in the nontumorigenic HBL100 line. Mol Cancer Ther. 2002;1:1161–72. [PubMed] [Google Scholar]
- 22.Arbeit JM, Howley PM, Hanahan D. Chronic estrogen-induced cervical and vaginal squamous carcinogenesis in human papillomavirus type 16 transgenic mice. Proc Natl Acad Sci U S A. 1999;93:2930–5. doi: 10.1073/pnas.93.7.2930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Bell MC, et al. Placebo-controlled trial of indole-3-carbinol in the treatment of CIN. Gynecol Oncol. 2000;78:123–9. doi: 10.1006/gyno.2000.5847. [DOI] [PubMed] [Google Scholar]
- 24.Cantley LC, Neel BG. New insights into tumor suppression: PTEN suppresses tumor formation by restraining the phosphoinositide 3-kinase/AKT pathway. Proc Natl Acad Sci U S A. 1999;96:4240–5. doi: 10.1073/pnas.96.8.4240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Li J, et al. PTEN, a putative protein tyrosine phosphatase gene mutated in human brain, breast, and prostate cancer [see comments] Science. 1997;275:1943–7. doi: 10.1126/science.275.5308.1943. [DOI] [PubMed] [Google Scholar]
- 26.Risinger JI, Hayes AK, Berchuck A, Barrett JC. PTEN/MMAC1 mutations in endometrial cancers. Cancer Res. 1997;57:4736–8. [PubMed] [Google Scholar]
- 27.Tashiro H, et al. Mutations in PTEN are frequent in endometrial carcinoma but rare in other common gynecological malignancies. Cancer Res. 1997;57:3935–40. [PubMed] [Google Scholar]
- 28.Su TH, et al. Mutation analysis of the putative tumor suppressor gene PTEN/MMAC1 in cervical cancer. Gynecol Oncol. 2000;76:193–9. doi: 10.1006/gyno.1999.5659. [DOI] [PubMed] [Google Scholar]
- 29.Cheung TH, et al. Epigenetic and genetic alternation of PTEN in cervical neoplasm. Gynecol Oncol. 2004;93:621–7. doi: 10.1016/j.ygyno.2004.03.013. [DOI] [PubMed] [Google Scholar]
- 30.Salvesen HB, et al. PTEN methylation is associated with advanced stage and microsatellite instability in endometrial carcinoma. Int J Cancer. 2001;91:22–6. doi: 10.1002/1097-0215(20010101)91:1<22::aid-ijc1002>3.0.co;2-s. [DOI] [PubMed] [Google Scholar]
- 31.Kang YH, Lee HS, Kim WH. Promoter methylation and silencing of PTEN in gastric carcinoma. Lab Invest. 2002;82:285–91. doi: 10.1038/labinvest.3780422. [DOI] [PubMed] [Google Scholar]
- 32.Garcia JM, et al. Promoter methylation of the PTEN gene is a common molecular change in breast cancer. Genes Chromosomes Cancer. 2004;41:117–24. doi: 10.1002/gcc.20062. [DOI] [PubMed] [Google Scholar]
- 33.Goel A, et al. Frequent inactivation of PTEN by promoter hypermethylation in microsatellite instability-high sporadic colorectal cancers. Cancer Res. 2004;64:3014–21. doi: 10.1158/0008-5472.can-2401-2. [DOI] [PubMed] [Google Scholar]
- 34.Myers MP, Stolarov JP, Eng C. P-TEN, the tumor suppressor from human chromosome 10q23, is a dual-specificity phosphatase. Proc Natl Acad Sci U S A. 1997;94:9052–7. doi: 10.1073/pnas.94.17.9052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Maehama T, Dixon JE. The tumor suppressor, PTEN/MMAC1, dephosphorylates the lipid second messenger, phosphatidylinositol 3,4,5-trisphosphate. J Biol Chem. 1998;273:13375–8. doi: 10.1074/jbc.273.22.13375. [DOI] [PubMed] [Google Scholar]
- 36.Stokoe D, et al. Dual role of phosphatidylinositol-3,4,5-trisphosphate in the activation of protein kinase B. Science. 1997;277:567–70. doi: 10.1126/science.277.5325.567. [DOI] [PubMed] [Google Scholar]
- 37.Andjelkovic M, et al. Role of translocation in the activation and function of protein kinase B. J. Biol. Chem. 1997;272:31515–24. doi: 10.1074/jbc.272.50.31515. [DOI] [PubMed] [Google Scholar]
- 38.Alessi DR, et al. 3-Phosphoinositide-dependent protein kinase-1 (PDK1): structural and functional homology with the Drosophila DSTPK61 kinase. Curr Biol. 1997;7:776–89. doi: 10.1016/s0960-9822(06)00336-8. [DOI] [PubMed] [Google Scholar]
- 39.Delcommenne M, et al. Phosphoinositide-3-OH kinase-dependent regulation of glycogen synthase kinase 3 and protein kinase B/AKT by the integrin-linked kinase. Proc Natl Acad Sci U S A. 1998;95:11211–6. doi: 10.1073/pnas.95.19.11211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Hresko RC, Murata H, Mueckler M. Phosphoinositide-dependent kinase-2 is a distinct protein kinase enriched in a novel cytoskeletal fraction associated with adipocyte plasma membranes. J Biol Chem. 2003;278:21615–22. doi: 10.1074/jbc.M302937200. [DOI] [PubMed] [Google Scholar]
- 41.Myers MP, et al. The lipid phosphatase activity of PTEN is critical for its tumor suppressor function. Proc Natl Acad Sci U S A. 1998;95:13513–8. doi: 10.1073/pnas.95.23.13513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Radu A, Neubauer V, Akagi T, Hanafusa H, Georgescu MM. PTEN induces cell cycle arrest by decreasing the level and nuclear localization of cyclin D1. Mol Cell Biol. 2003;23:6139–49. doi: 10.1128/MCB.23.17.6139-6149.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Nakamura N, et al. Forkhead transcription factors are critical effectors of cell death and cell cycle arrest downstream of PTEN. Mol Cell Biol. 2000;20:8969–82. doi: 10.1128/mcb.20.23.8969-8982.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Lu Y, et al. The PTEN/MMAC1/TEP tumor suppressor gene decreases cell growth and induces apoptosis and anoikis in breast cancer cells. Oncogene. 1999;18:7034–45. doi: 10.1038/sj.onc.1203183. [DOI] [PubMed] [Google Scholar]
- 45.Sun S, Steinberg BM. Identification of PTEN as a negative regulator of STAT3 activation. J Gen Virol. 2002;83:1651–8. doi: 10.1099/0022-1317-83-7-1651. [DOI] [PubMed] [Google Scholar]
- 46.Gu J, et al. Shc and FAK differentially regulate cell motility and directionality modulated by PTEN. J Cell Biol. 1999;146:389–403. doi: 10.1083/jcb.146.2.389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Dellas A, et al. Angiogenesis in cervical neoplasia: microvessel quantitation in precancerous lesions and invasive carcinomas with clinicopathological correlations. Gynecol Oncol. 1997;67:27–33. doi: 10.1006/gyno.1997.4835. [DOI] [PubMed] [Google Scholar]
- 48.Davidson B, Goldberg I, Kopolovic J. Angiogenesis in uterine cervical intraepithelial neoplasia and squamous cell carcinoma: an immunohistochemical study. Int J Gynecol Pathol. 1997;16:335–8. doi: 10.1097/00004347-199710000-00007. [DOI] [PubMed] [Google Scholar]
- 49.Lee JS, Kim HS, Jung JJ, Lee MC, Park CS. Angiogenesis, cell proliferation and apoptosis in progression of cervical neoplasia. Anal Quant Cytol Histol. 2002;24:103–13. [PubMed] [Google Scholar]
- 50.Smith-McCune K, Zhu YH, Hanahan D, Arbeit J. Cross-species comparison of angiogenesis during the premalignant stages of squamous carcinogenesis in the human cervix and K14-HPV16 transgenic mice. Cancer Res. 1997;57:1294–300. [PubMed] [Google Scholar]
- 51.Chang X, et al. 3,3′-Diindolylmethane inhibits angiogenesis and the growth of transplantable human breast carcinoma in athymic mice. Carcinogenesis. 2005;26:771–8. doi: 10.1093/carcin/bgi018. [DOI] [PubMed] [Google Scholar]
- 52.Wen S, et al. PTEN controls tumor-induced angiogenesis. Proc Natl Acad Sci U S A. 2001;98:4622–7. doi: 10.1073/pnas.081063798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Pore N, Liu S, Haas-Kogan DA, O’Rourke DM, Maity A. PTEN mutation and epidermal growth factor receptor activation regulate vascular endothelial growth factor (VEGF) mRNA expression in human glioblastoma cells by trans-activating the proximal VEGF promoter. Cancer Res. 2003;63:236–41. [PubMed] [Google Scholar]
- 54.Smith-McCune KK, Weidner N. Demonstration and characterization of the angiogenic properties of cervical dysplasia. Cancer Res. 1994;54:800–4. [PubMed] [Google Scholar]
- 55.Riby JE, Chang GH, Firestone GL, Bjeldanes LF. Ligand-independent activation of estrogen receptor function by 3,3′-diindolylmethane in human breast cancer cells. Biochem Pharmacol. 2000;60:167–77. doi: 10.1016/s0006-2952(00)00307-5. [DOI] [PubMed] [Google Scholar]
- 56.Waite KA, Sinden MR, Eng C. Phytoestrogen exposure elevates PTEN levels. Hum Mol Genet. 2005;14:1457–63. doi: 10.1093/hmg/ddi155. [DOI] [PubMed] [Google Scholar]
- 57.Fang MX, et al. Reversal of hypermethylation and reactivation of P161NK4a, RARbeta, and MGMT genes by genistein and other isoflavones from soy. Clin Cancer Res. 2005;11:7033–41. doi: 10.1158/1078-0432.CCR-05-0406. [DOI] [PubMed] [Google Scholar]
- 58.Virolle T, et al. The Egr-1 transcription factor directly activates PTEN during irradiation-induced signaling. Nat Cell Biol. 2001;3:1124–8. doi: 10.1038/ncb1201-1124. [DOI] [PubMed] [Google Scholar]