Abstract
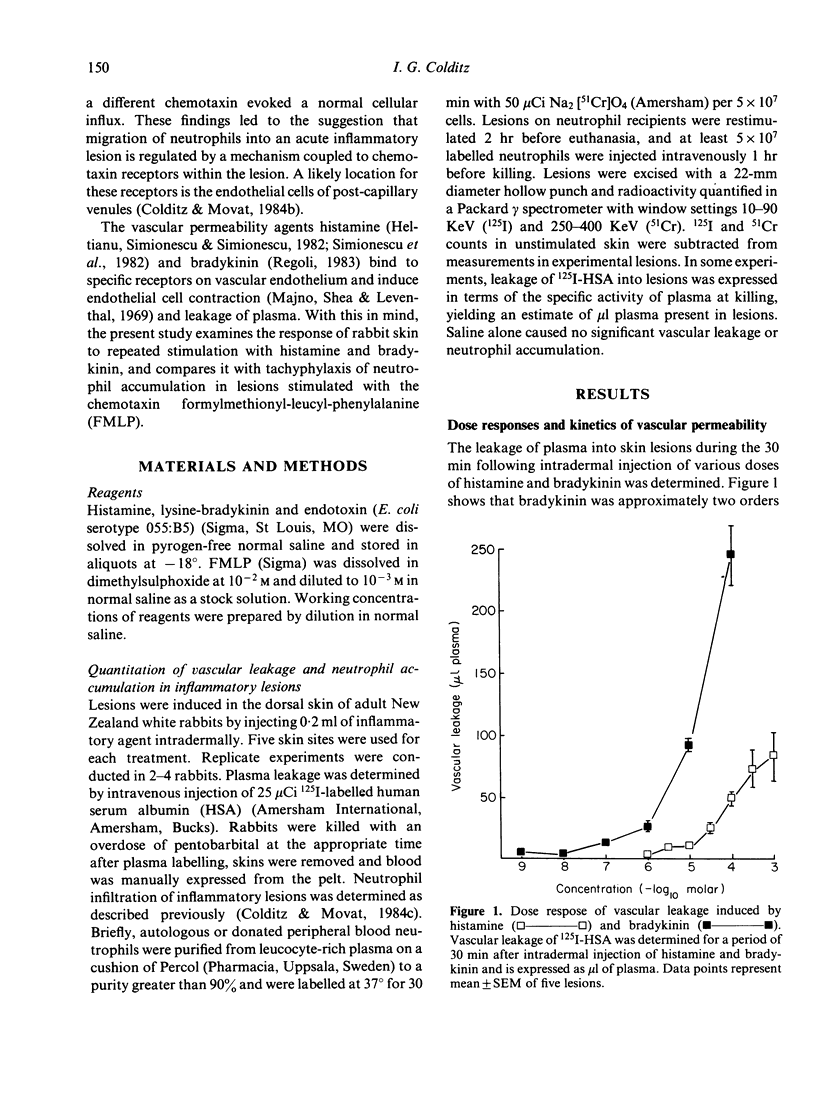
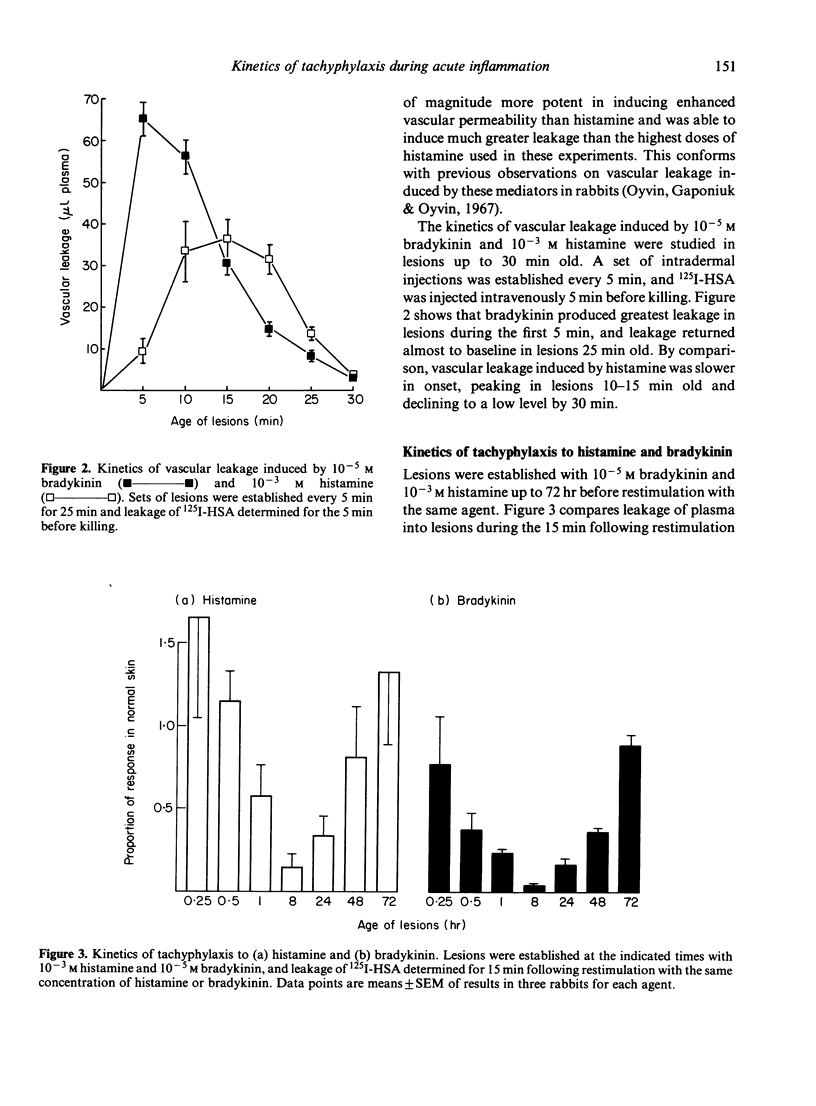
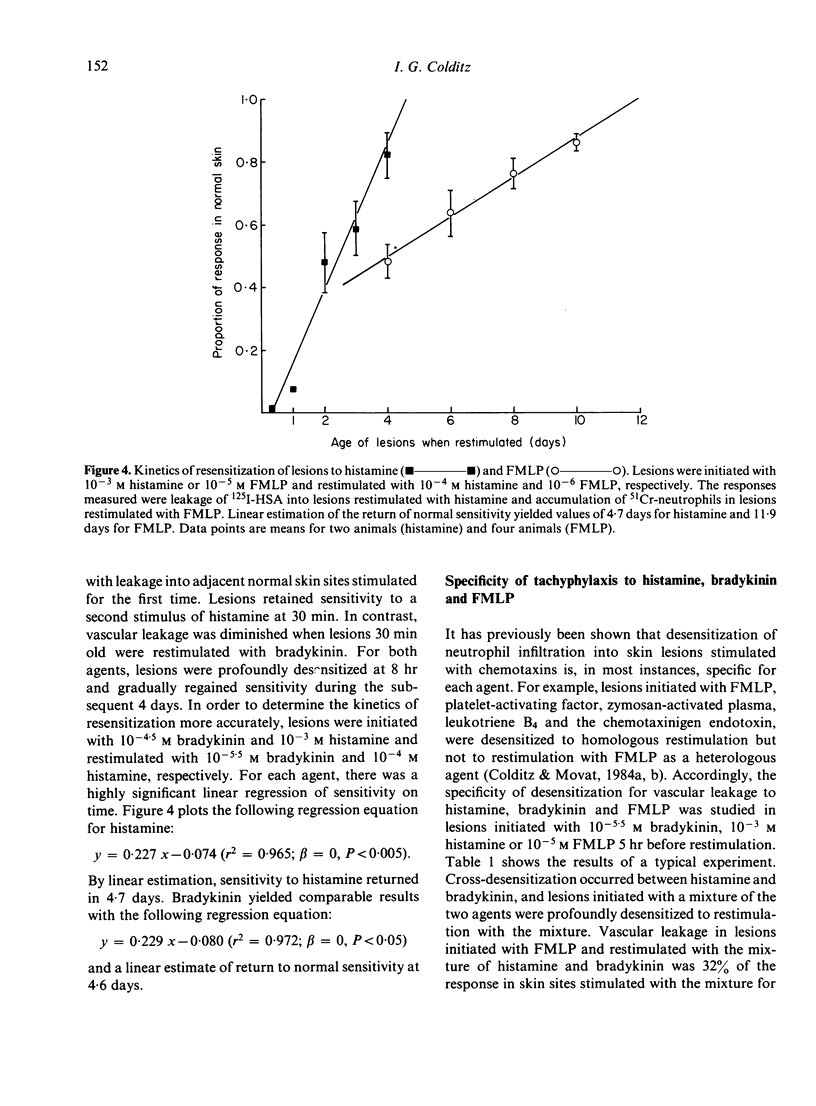
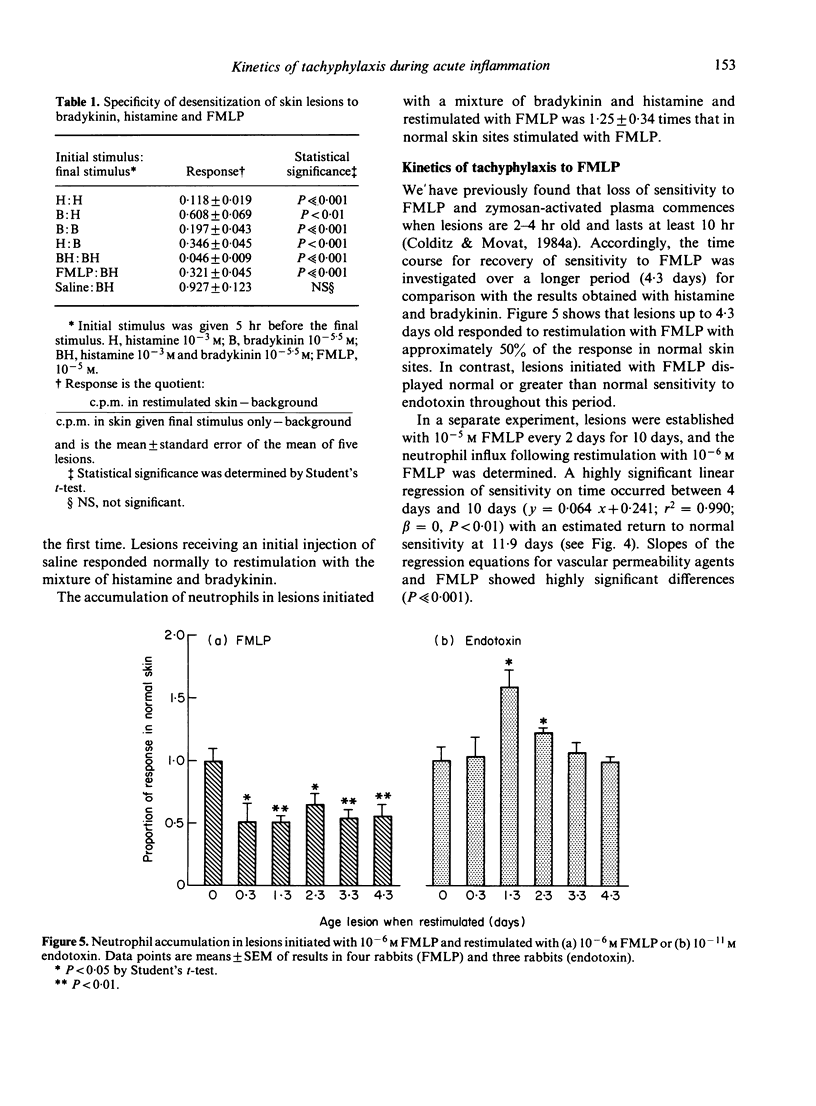
The kinetics of vascular leakage and tachyphylaxis induced by histamine and bradykinin were examined in rabbit skin and were compared with the kinetics of tachyphylaxis of neutrophil accumulation in lesions induced with the chemotaxin formylmethionyl-leucyl-phenylalanine (FMLP). Maximal leakage of 125I-human serum albumin occurred during the first 5 min after injection of bradykinin and from 10 to 20 min after injection of histamine. Tachyphylaxis developed within 30 min of injection of bradykinin and 1 hr after injection of histamine. For both agents, there was a linear regression of sensitivity with time from 8 hr to 4 days, with normal sensitivity estimated to return at 4.6 days for bradykinin and 4.7 days for histamine. Marked cross-desensitization occurred between the two agents, and lesions initiated with the chemotaxin FMLP were desensitized to restimulation with a mixture of histamine and bradykinin. Initiation of lesions with histamine and bradykinin did not diminish the accumulation of neutrophils when lesions were restimulated with FMLP. The kinetics of tachyphylaxis of neutrophil accumulation in lesions stimulated with FMLP exhibited a linear regression of sensitivity on time between 4 days and 10 days, with estimated resensitization at 11.9 days. Histamine and bradykinin induce enhanced vascular permeability when endothelial cells in post-capillary venules contract following stimulation of their membrane receptors for these agents. We have recently proposed that the migration of neutrophils into acute inflammatory lesions is regulated by a mechanism coupled to chemotaxin receptors which may be similarly located on endothelial cells within the lesions. The present experiments indicate that expression of receptors for vascular permeability agents and the chemotaxin FMLP are independent events with distinct kinetics.
Full text
PDF
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Ager A., Gordon J. L. Differential effects of hydrogen peroxide on indices of endothelial cell function. J Exp Med. 1984 Feb 1;159(2):592–603. doi: 10.1084/jem.159.2.592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alhenc-Gelas F., Tsai S. J., Callahan K. S., Campbell W. B., Johnson A. R. Stimulation of prostaglandin formation by vasoactive mediators in cultured human endothelial cells. Prostaglandins. 1982 Nov;24(5):723–742. doi: 10.1016/0090-6980(82)90040-5. [DOI] [PubMed] [Google Scholar]
- Askenase P. W., Metzler C. M., Gershon R. K. Localization of leucocytes in sites of delayed-type hypersensitivity and in lymph nodes: dependence on vasoactive amines. Immunology. 1982 Oct;47(2):239–246. [PMC free article] [PubMed] [Google Scholar]
- Baumgarten A., Melrose G. J., Vagg W. J. interactions between histamine and bradykinin assessed by continuous recording of increased vascular permeability. J Physiol. 1970 Jul;208(3):669–675. doi: 10.1113/jphysiol.1970.sp009141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Catt K. J., Harwood J. P., Aguilera G., Dufau M. L. Hormonal regulation of peptide receptors and target cell responses. Nature. 1979 Jul 12;280(5718):109–116. doi: 10.1038/280109a0. [DOI] [PubMed] [Google Scholar]
- Colditz I. G., Movat H. Z. Chemotactic factor-specific desensitization of skin to infiltration by polymorphonuclear leukocytes. Immunol Lett. 1984;8(2):83–87. doi: 10.1016/0165-2478(84)90055-5. [DOI] [PubMed] [Google Scholar]
- Colditz I. G., Movat H. Z. Desensitization of acute inflammatory lesions to chemotaxins and endotoxin. J Immunol. 1984 Oct;133(4):2163–2168. [PubMed] [Google Scholar]
- Colditz I. G., Movat H. Z. Kinetics of neutrophil accumulation in acute inflammatory lesions induced by chemotaxins and chemotaxinigens. J Immunol. 1984 Oct;133(4):2169–2173. [PubMed] [Google Scholar]
- Engerman R. L., Pfaffenbach D., Davis M. D. Cell turnover of capillaries. Lab Invest. 1967 Dec;17(6):738–743. [PubMed] [Google Scholar]
- Greaves M., Shuster S. Responses of skin blood vessels to bradykinin, histamine and 5-hydroxytryptamine. J Physiol. 1967 Nov;193(2):255–267. doi: 10.1113/jphysiol.1967.sp008356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hay J. B., Hobbs B. B. The flow of blood to lymph nodes and its relation to lymphocyte traffic and the immune response. J Exp Med. 1977 Jan 1;145(1):31–44. doi: 10.1084/jem.145.1.31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heltianu C., Simionescu M., Simionescu N. Histamine receptors of the microvascular endothelium revealed in situ with a histamine-ferritin conjugate: characteristic high-affinity binding sites in venules. J Cell Biol. 1982 May;93(2):357–364. doi: 10.1083/jcb.93.2.357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Issekutz A. C. Effect of vasoactive agents on polymorphonuclear leukocyte emigration in vivo. Lab Invest. 1981 Sep;45(3):234–240. [PubMed] [Google Scholar]
- Issekutz A. C., Movat H. Z. The effect of vasodilator prostaglandins on polymorphonuclear leukocyte infiltration and vascular injury. Am J Pathol. 1982 Jun;107(3):300–309. [PMC free article] [PubMed] [Google Scholar]
- Johnson A. R., Erdös E. G. Release of histamine from mast cells by vasoactive peptides. Proc Soc Exp Biol Med. 1973 Apr;142(4):1252–1256. doi: 10.3181/00379727-142-37219. [DOI] [PubMed] [Google Scholar]
- Johnston M. G., Hay J. B., Movat H. Z. The modulation of enhanced vascular permeability by prostaglandins through alterations in blood flow (hyperemia). Agents Actions. 1976 Nov;6(6):705–711. doi: 10.1007/BF02026092. [DOI] [PubMed] [Google Scholar]
- MILES A. A., MILES E. M. Vascular reactions to histamine, histamine-liberator and leukotaxine in the skin of guinea-pigs. J Physiol. 1952 Oct;118(2):228–257. doi: 10.1113/jphysiol.1952.sp004789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Majno G., Shea S. M., Leventhal M. Endothelial contraction induced by histamine-type mediators: an electron microscopic study. J Cell Biol. 1969 Sep;42(3):647–672. doi: 10.1083/jcb.42.3.647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marceau F., Knap M., Regoli D. Pharmacological characterization of the vascular permeability enhancing effects of kinins in the rabbit skin. Can J Physiol Pharmacol. 1981 Sep;59(9):921–926. doi: 10.1139/y81-142. [DOI] [PubMed] [Google Scholar]
- Moore T. C. The modulation by prostaglandins of increases in lymphocyte traffic induced by bradykinin. Immunology. 1984 Mar;51(3):455–460. [PMC free article] [PubMed] [Google Scholar]
- Moses J. M., Geschickter E. H., Ebert R. H. Pathogenesis of inflammation. The relationship of enhanced permeability to leucocyte mobilization in delayed inflammation. Br J Exp Pathol. 1968 Aug;49(4):385–394. [PMC free article] [PubMed] [Google Scholar]
- Oyvin I. A., Gaponiuk P. Y., Oyvin V. I. The effect of bradykinin on permeability of skin blood vessels. Experientia. 1967 Nov 15;23(11):925–926. doi: 10.1007/BF02136224. [DOI] [PubMed] [Google Scholar]
- Regoli D. Pharmacology of bradykinin and related kinins. Adv Exp Med Biol. 1983;156:569–584. [PubMed] [Google Scholar]
- Sholley M. M., Cotran R. S. Endothelial DNA synthesis in themicrovasculature of rat skin during the hair growth cycle. Am J Anat. 1976 Oct;147(2):243–254. doi: 10.1002/aja.1001470208. [DOI] [PubMed] [Google Scholar]
- Simionescu N., Heltianu C., Antohe F., Simionescu M. Endothelial cell receptors for histamine. Ann N Y Acad Sci. 1982;401:132–149. doi: 10.1111/j.1749-6632.1982.tb25713.x. [DOI] [PubMed] [Google Scholar]


