Short abstract
Prompt diagnosis and management of community acquired pneumonia saves lives. This article summarises the latest key recommendations in the management of pneumonia and is intended for junior doctors managing this common condition
Why is it important?
Community acquired pneumonia is an important healthcare concern. The annual incidence rate is 6/1000 in the 18-39 age group. This rises to 34/1000 in people aged 75 years and over. Admission to hospital is needed in 20-40% of patients with community acquired pneumonia. About 5-10% of these patients are admitted to intensive care. The overall mortality from community acquired pneumonia is 5-10%, so it is important to identify and treat patients with this disease.1,2 We will concentrate on three aspects of hospital management: assessment of disease severity, investigations, and antibiotic treatment.
What are the symptoms and signs of pneumonia?
Pneumonia is defined as an acute lower respiratory tract infection, together with new radiographic shadowing.1 Anybody can get pneumonia, although it is most common in elderly people. The clinical history of pneumonia may include one or more of:
Pleuritic chest pain
Shortness of breath
Cough
Production of sputum
Rigors or night sweats
Confusion.
On examination the signs may include:
Raised respiratory rate
Fever of > 38°C
Focal chest signs: decreased chest expansion, dullness on percussion, decreased entry of air, bronchial breathing, and crackles (none, some, or all of these may be present).
In elderly people, fever may not be present and new onset of mental confusion is more common.3
Summary points
Pneumonia is common and has high mortality
Simple scoring systems help to distinguish between patients who can be managed at home and those who may need intensive care
Antibiotic treatment is guided by the severity of disease
Newer antibiotics have their place, but penicillin and macrolides (such as erythromycin) are still first line drugs
What investigations should we do?
Table 1 lists the other diagnoses that should be considered when patients present with focal chest signs and increasing shortness of breath. A chest x ray is crucial to making the diagnosis of pneumonia. New chest signs on examination are helpful but not specific. One clinical study conducted in primary care in the United Kingdom showed that only 40% of patients with new lower respiratory tract symptoms and focal chest signs had radiological evidence of pneumonia.4
Table 1.
Differential diagnosis in community acquired pneumonia
| Alternative diagnosis | Supporting clinical feature |
|---|---|
| Exacerbation of chronic obstructive pulmonary disease | History of the disease or heavy smoking; polyphonic wheeze on examination |
| Exacerbation of asthma | Patient known to have asthma; wheeze on examination |
| Pulmonary oedema | Third heart sound and abnormal electrocardiogram |
| Fibrosing alveolitis | Long history of chronic cough, fine inspiratory crackles on examination |
| Lung cancer | Long history of chronic cough, haemoptysis, weight loss, and history of smoking |
| Bronchiectasis | Long history of chronic cough that produces large amounts of purulent sputum |
| Inhaled foreign body | History of inhalation or coughing when eating |
| Pulmonary emboli | Sudden onset of shortness of breath and chest pain; occasional haemoptysis |
About 40% of patients have a pleural effusion, but the amount of fluid is usually small.1 A microbiological diagnosis can be made on routine microbiological tests in only about 15% of inpatients; this percentage is even lower in patients with mild or moderate pneumonia and no comorbid illnesses.5 The following tests are recommended for patients admitted with non-severe community acquired pneumonia:
Full blood count
Urea and electrolytes
Liver function tests
Sputum culture
Chest x ray
Blood cultures.
In patients with severe pneumonia, tests for atypical pathogens (Mycoplasma pneumoniae, Chlamydia sp, Coxiella burnetii, Legionella sp) and viruses should also be carried out. These are:
Legionella urinary antigen test
Direct immunofluorescence on respiratory samples
Serological tests on acute and convalescent serum samples.
Testing for pneumococcal urinary antigen is also recommended in severe pneumonia.
How can we identify patients with severe pneumonia?
Severe pneumonia has a high mortality, so it is important to identify patients at high risk of complications and death. Many studies have looked at features associated with poor prognosis. More than 40 indicators of poor prognosis have been identified, and complex scoring systems have been developed.6 The most widely studied one is a North American 20 point system,7 but this system is not practical in many clinical settings and is not used widely in the UK.
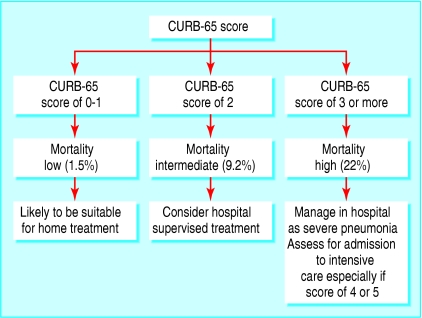
The British Thoracic Society recommends the CURB-65 scoring system.8,9 This is a 6 point score (range 0-5) that gives one point each for confusion (abbreviated mental test score ≤ 8 or new disorientation in person, place, or time); urea > 7 mmol/l; respiratory rate ≥ 30/min; low blood pressure (systolic blood pressure < 90 mm Hg or diastolic blood pressure ≤ 60 mm Hg); and age 65 years or more. The score relates to mortality, and severe pneumonia is defined as a CURB-65 score of 3 or more. The British Thoracic Society advocates management strategies based on this score (fig 1).
Clinical judgment is needed when using the scoring system. If the score is low but the patient is unwell he or she could still have severe pneumonia. For example, a young person with normal blood pressure and urea but low oxygen saturation despite supplemental oxygen could have severe pneumonia and may need to be reviewed by the intensive care team.
How do we treat it?
Pneumonia must be treated with the appropriate antibiotics. Table 2 shows the current recommendations of the British Thoracic Society for empirical treatment of community acquired pneumonia.
Table 2.
Current treatment regimens for pneumonia
| Severity of pneumonia | Treatment |
|---|---|
| Non-severe (home treated or hospital treated) and admitted for non-clinical reasons or previously untreated in the community | Oral amoxicillin 500-1000 mg three times a day, erythromycin 500 mg four times a day, or clarithromycin 500 mg twice a day |
| Non-severe, hospital treated | Oral amoxicillin 500-1000 mg three times a day plus either erythromycin 500 mg four times a day or clarithromycin 500 mg twice a day. If intravenous treatment is needed, ampicillin 500 mg four times a day or benzylpenicillin 1200 mg four times a day, plus either erythromycin 500 mg four times a day or clarithromycin 500 mg twice a day |
| Alternative treatment for non-severe hospital treated | Oral levofloxacin 500 mg once daily or moxifloxacin 400 mg once daily |
| Severe, hospital treated | Intravenous broad spectrum β lactam antibiotics (co-amoxiclav 1.2 g three times a day, cefuroxime 1.5 g three times a day, cefotaxime 1 g three times a day, or ceftriaxone 2 g once daily), plus either intravenous erythromycin 500 mg four times a day or clarithromycin 500 mg twice a day |
| Alternative treatment for severe, hospital treated | Intravenous levofloxacin* 500 mg twice a day plus benzylpenicillin 1200 mg four times a day |
Other new fluoroquinolones (such as intravenous moxifloxacin) are not currently licensed in severe community acquired pneumonia in the UK.
Figure 1.
Assessment of severity of pneumonia with the CURB-65 scoring system. Reproduced and adapted with permission1
Since the development of new fluoroquinolones with enhanced activity against Gram positive organisms (such as Streptococcus pneumoniae), the choice of antibiotic for respiratory tract infections has broadened. Two such agents currently available in the UK are levofloxacin and moxifloxacin. These antimicrobials are active against atypical pathogens and Streptococcus pneumoniae. However, concerns exist about the widespread use of these drugs as they have been associated with the emergence of fluoroquinolone resistant streptococci, an increase in the development of methicillin resistant Staphylococcus aureus (MRSA), and diarrhoea associated with Clostridium difficile infection.10,11
The new fluoroquinolones are not recommended for use in the community but should be reserved for the hospital setting. Currently in the UK, only levofloxacin has a licensed intravenous preparation. This is expensive and not available in many hospitals.
Who should receive intravenous antibiotics?
Patients should receive intravenous antibiotics if they have:
Severe pneumonia (CURB-65 score ≥ 3)
Functional or anatomical reasons for malabsorption
Impaired consciousness
Impaired swallowing reflex.1
Sample questions
-
A 70 year old man is admitted to intensive care with severe community acquired pneumonia. Which of the following regimens would you recommend?
- Intravenous cefotaxime 1 g three times a day
- Intravenous cefotaxime 1 g three times a day plus clarithromycin 500 mg twice a day
- Intravenous ceftriaxone 2 g once daily plus erythromycin 250 mg four times a day
- Intravenous co-amoxiclav 1.2 g three times a day plus oral clarithromycin 500 mg twice a day
-
A 52 year old man who smokes and has pneumonia has been taking antibiotics for five days. He is improving clinically. His observations are: temperature 37.3°C, heart rate 80/min, blood pressure 120/80 mm Hg, respiratory rate 14/min. Which of these statements are correct?
- It is appropriate to discharge him home
- He should stay in hospital
- He should stop his antibiotics
- He does not need a repeat chest x ray
- He needs to be seen in clinic in two weeks
Intravenous antibiotics should be changed to oral as soon as possible. Resolution of the patient's fever, improved oxygen status, and haemodynamic stability are indicators for oral treatment.
In non-severe pneumonia, antibiotics should be given for seven days. Patients with severe pneumonia but no microbiological confirmation usually receive 10 days of intravenous drugs. Patients who are infected with Legionella sp, S aureus, and Gram negative bacteria should receive 14-21 days of antimicrobial treatment.
C reactive protein
Measuring C reactive protein (an acute phase protein) concentrations is useful for managing pneumonia. Ninety five percent of patients admitted with community acquired pneumonia have a C reactive protein value > 50 mg/l.12 The initial concentration of this protein does not correlate closely with the severity of disease, but it can be used as an indicator of response to treatment. Treatment failure or complications (such as an empyema) should be considered if C reactive protein is not 50% lower by the fourth day.13
When should patients be discharged home?
It is important to know when it is safe to discharge patients. Features of clinical instability are:
Temperature > 37.8°C
Heart rate > 100/min
Respiratory rate > 24/min
Systolic blood pressure < 90 mm Hg
Oxygen saturation < 90%
Abnormal mental status
Inability to take oral drugs.
One study showed that 40% of patients who had two or more of these features within 24 hours before they were discharged died or were readmitted within 30 days, compared with 11% of those with none of these features.14
Every patient with pneumonia should be reviewed about six weeks after discharge. In patients with poor clinical recovery, a chest x ray should be done to identify those with possible underlying malignancy. Patients with a high risk of malignancy, such as those who smoke or who are aged over 50 years, should also have a repeat chest x ray at six weeks.
Competing interests: None declared.
Editorial by Goossens and Little
This article is based on a module that is available on BMJ Learning (www.bmjlearning.com)
References
- 1.British Thoracic Society. Guidelines for the management of community acquired pneumonia in adults. Thorax 2001;56(suppl 4): 1-64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Macfarlane JT, Boldy D. 2004 update of BTS guidelines: what's new? Thorax 2004;59: 364-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Metlay JP, Schulz R, Li YH, Singer DE, Marrie TJ, Coley CM, et al. Influence of age on symptoms at presentation in patients with community-acquired pneumonia in the community. Arch Intern Med 1997;157: 1453-9. [PubMed] [Google Scholar]
- 4.Woodhead MA, Macfarlane JT, McCracken JS, Rose DH, Finch RG. Prospective study of the aetiology and outcome of pneumonia in the community. Lancet 1987;I: 671-4. [DOI] [PubMed] [Google Scholar]
- 5.Woodhead MA, Arrowsmith J, Chamberlain-Webber R, Wooding S, Williams I. The value of routine microbial investigation in community-acquired pneumonia. Respir Med 1991;85: 313-7. [DOI] [PubMed] [Google Scholar]
- 6.Metlay JP, Fine MJ. Testing strategies in the initial management of patients with community-acquired pneumonia. Ann Intern Med 2003;138: 109-18. [DOI] [PubMed] [Google Scholar]
- 7.Fine MJ, Auble TE, Yearly DM, Hanuse BH, Weissfeld LA, Singer DE, et al. A prediction rule to identify low-risk patients with community-acquired pneumonia. N Engl J Med 1997;336: 243-50. [DOI] [PubMed] [Google Scholar]
- 8.Lim WS, Van der Eerden MM, Laing R, Boersma WG, Karalus N, Town GI, et al. Defining community acquired pneumonia severity on presentation to hospital: an international derivation and validation study. Thorax 2003;58: 377-82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ewig S, Torres A, Woodhead M. Assessment of pneumonia severity: a European perspective. Eur Respir J 2006;27: 6-8. [DOI] [PubMed] [Google Scholar]
- 10.Weber SG, Gold HS, Hoopers DC, Karchmer AW, Carmeoli Y. Fluoroquinolones and the risk of methicillin-resistant Staphylococcus aureus in hospitalized patients. Emerg Infect Dis 2003;9: 1415-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Loo VE, Poirer L, Miller MA, Oughton M, Libman MD, Michaud S, et al. A predominantly clonal multi-institutional outbreak of Clostridium difficile-associated diarrhea with high morbidity and mortality. N Engl J Med 2005;353: 2442-9. [DOI] [PubMed] [Google Scholar]
- 12.Hansson LO, Hedlund JU, Ortqvist A. Sequential changes of inflammatory and nutritional markers in patients with community acquired pneumonia. Scan J Clin Lab Invest 1997;57: 11-8. [DOI] [PubMed] [Google Scholar]
- 13.Smith RP, Lipworth BJ, Cree IA, Spiers EM, Winter JH, et al. C-reactive protein. A clinical marker in community acquired pneumonia. Chest 1995;108: 1288-91. [DOI] [PubMed] [Google Scholar]
- 14.Halm EA, Fine MJ, Kapoor WN, Singer DE, Marrie TJ, Siu AC. Instability on hospital discharge and the risk of adverse outcome in patients with pneumonia. Arch Intern Med 2002;162: 1278-84. [DOI] [PubMed] [Google Scholar]