Abstract
Hemolytic uremic syndrome, the leading cause of kidney failure in children, often follows infection with enterohemorrhagic Escherichia coli and is mediated by the Shiga type toxins, particularly type 2 (Stx2), produced by such strains. The challenge in protecting against this life-threatening syndrome is to stimulate an immune response at the site of infection while also protecting against Shiga intoxication at distal sites such as the kidney. As one approach to meeting this challenge, we sought to develop and characterize a prototypic orally delivered, plant-based vaccine against Stx2, an AB5 toxin. First, we genetically inactivated the Stx2 active A subunit gene and then optimized both subunit genes for expression in plants. The toxoid genes were then transformed into the Nicotiana tabacum (tobacco) cell line NT-1 by Agrobacterium tumefaciens-mediated transformation. Toxoid expression was detected in NT-1 cell extracts, and the assembly of the holotoxoid was confirmed. Finally, mice were immunized by feeding with the toxoid-expressing NT-1 cells or by parenteral immunization followed by oral vaccination (prime–boost strategy). The immunized mice produced Stx2-specific mucosal IgA and Stx2-neutralizing serum IgG. The protective efficacy of these responses was assessed by challenging the immunized mice with E. coli O91:H21 strain B2F1, an isolate that produces an activatable variant of Stx2 (Stx2d) and is lethal to mice. The oral immunization fully protected mice from the challenge. Results of this study demonstrated that a plant-based oral vaccine can confer protection against lethal systemic intoxication.
Keywords: enterohemorrhagic Escherichia coli, hemolytic uremic syndrome
Shiga toxin-producing Escherichia coli (STEC) cause an estimated 100,000 cases of hemorrhagic colitis per year in the United States (1). Disease is most often associated with enterohemorrhagic E. coli, a subset of STEC that includes serotype O157:H7. Six percent of these infections progress to the life-threatening systemic disease called hemolytic uremic syndrome, which is characterized by thrombocytopenia, hemolytic uremia, and kidney failure. Hemolytic uremic syndrome occurs as a consequence of the action of members of the Shiga toxin (Stx) family (2). Stxs are AB5 holotoxins that consist of one catalytic A subunit, a 28S rRNA N-glycosidase polypeptide (3), which is noncovalently associated with a pentameric B subunit that binds to the widely distributed globotriaosyl ceramide (Gb3) cellular receptor (4, 5). STEC that infect humans produce two major types of Stx: Stx1 and Stx2. These Stxs are only 55% identical by amino acid sequence and consequently are antigenically distinct. Antibodies raised against one type do not cross-neutralize the other (6–8). Although STEC strains may produce one or both types of Stx, Stx2 is associated with the most severe disease in humans. Therefore, we began our efforts to develop a vaccine against Stx intoxication by focusing on Stx2.
Plant-based vaccines have several advantages: (i) they provide a convenient, safe, and familiar vehicle for oral delivery (9); (ii) they are inexpensive to produce in large quantities (10); (iii) they are unlikely to be contaminated with animal pathogens, a potential problem with tissue culture-derived vaccines (11); and, (iv) encapsulation of immunizing proteins in plant tissue protects the antigens destined for delivery to the gut (12). We recently described the construction of an orally delivered plant-based vaccine against the primary adherence factor of enterohemorrhagic E. coli, intimin (13). In that study, the Nicotiana tabacum cell line NT-1 was modified by means of Agrobacterium-mediated transformation to express the C-terminal binding domain of intimin. Upon oral challenge with a wild-type enterohemorrhagic E. coli strain, colonization was reduced in the mice that had been fed a regimen of intimin-expressing NT-1 cells.
In the work described here, we used the same strategy to express a genetically inactivated Stx2 toxoid in NT-1 cells, to stimulate an immune response in the gut against Stx2 and, more importantly, to protect against systemic Stx2 intoxication. The efficacy of the vaccine was tested in the streptomycin-treated mouse model of STEC infection. In that model, oral challenge with an E. coli O91:H21 strain, B2F1, that produces an activatable variant of Stx2 (Stx2d) results in tubular necrosis and death (14, 15). That this toxin is entirely responsible for kidney lesions and death of infected mice is indicated by the repeated finding that, with passive administration of neutralizing monoclonal anti-Stx2 antibodies, the infected animals survive with no evidence of renal pathology (16, 17).
Results
Expression of Stx2 Genes in NT-1 Cells.
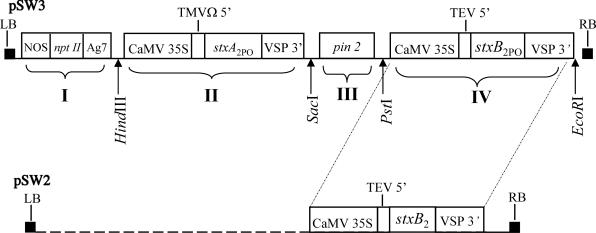
First, the bacterial Stx2 toxoid-encoding sequences were modified, or plant-optimized (indicated by subscript PO), to eliminate sequences that might be recognized as eukaryotic mRNA termination sites, splice sites, or polyadenylation sequences in NT-1 cells and thus alter antigen expression (18–20). Three such silent mutations were introduced into the toxoid A subunit gene to yield stxA2PO. A plant-optimized stxB2 (stxB2PO) was synthesized by ligase chain reaction to incorporate a total of 37 silent mutations. Next, the modified StxA2 and StxB2 subunit genes, which are transcribed in one operon by bacteria, were cloned as individual ORFs flanked with plant or viral elements to facilitate transcription of each protein in NT-1 cells (Fig. 1). Then, two dual-expression cassettes were assembled. One consisted of the plant-optimized stxA2 toxoid gene and the plant-optimized stxB2 gene, separated by a terminator sequence to ensure the independent expression of both toxoid subunits. The other cassette contained the plant-optimized StxA2 toxoid gene, the intergenic terminator, and the native StxB2 gene. Finally, each dual-expression cassette was cloned into the binary vector pGPTV-Kan (21) between the left and right border sequences that define the region that is transferred to plants [transferred DNA (T-DNA)] during Agrobacterium infection. The resulting plasmids, pSW2 (toxoided stxA2PO/native stxB2) or pSW3 (toxoided stxA2PO/stxB2PO), were transformed into Agrobacterium tumefaciens that was then used to infect NT-1 cells as described (13).
Fig. 1.
Diagram of the plant transformation vectors pSW3 and pSW2. Shown are the genetic elements in pGPTV-Kan between the left border (LB) and right border (RB) sequences that define the transferred DNA. I: npt II, the neomycin phosphotransferase gene for kanamycin resistance, flanked by the nopaline synthase promoter (NOS) and the nopaline synthase polyadenylation signal (Ag7). II: the toxoid stxA2PO, flanked by the cauliflower mosaic virus (CaMV) 35S RNA promoter, followed by the 5′ untranslated region (UTR) from tobacco mosaic virus (TMVΩ) and the soybean vegetative storage protein (VSP) 3′ polyadenylation sequence. III: an intergenic terminator sequence derived from the potato proteinase inhibitor II gene, pin2. IV: the plant-optimized stxB2PO (pSW3) or native stxB2 (pSW2) eukaryotic expression cassette with the tobacco etch virus (TEV) 5′ UTR. Restriction sites used for ligations are indicated below the diagram.
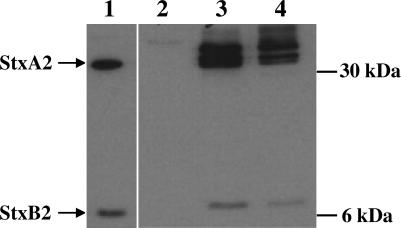
Because Agrobacterium-mediated transformation results in random insertions of the transferred DNA into plant chromosomes, the levels of expression of transferred genes may vary among recipient clones, depending on the site of insertion. Western blot analysis was used to identify kanamycin-resistant transformants that expressed detectable levels of Stx2 toxoid (Fig. 2). Ten of the 17 kanamycin-resistant NT-1 clones derived from pSW2, and 6 of the 10 derived from pSW3, yielded detectable Stx2 expression by Western blot analysis (data not shown). Two representative clones, NT#2 transformed with stxA2PO/stxB2 and NT#3 transformed with stxA2PO/stxB2PO toxoid genes, were selected for further study because they maintained stable toxoid expression. Another NT-1 clone that was transformed with the pGPTV-Kan vector that encodes the kanamycin resistance marker npt II but no other ORFs in the transferred-DNA region, was renamed NT-1KanR and served as negative vaccine control material.
Fig. 2.
Western blot analysis of the Stx2 holotoxoid expressed by transformed NT-1 clones. The positive control consisted of 10 ng of the wild-type Stx2 purified from E. coli DH5α that harbored pMJ100 (39) (lane 1). Sonic lysates of 50 mg of fresh plant cells were used to load lanes 2–4. Lane 2, NT-1KanR clone served as the negative control; lane 3, NT#2 clone; and lane 4, NT#3 clone. Stx2A and Stx2B subunit positions are indicated by arrows.
The antigen concentrations expressed by NT-1 cells were estimated from Western blots by comparison of pixel densities of bands observed from known concentrations of purified Stx2 with those observed from NT-1 cell extracts. The NT#2 clone yielded 8.2 ± 0.5 μg of Stx2 toxoid per gram of tobacco cells, and NT#3 yielded 6.5 ± 2.5 μg per gram of NT-1 cells. The sequence changes in the plant-optimized B subunit gene did not seem to improve protein expression; however, the chromosomal sites of toxoid gene insertion may also have influenced the relative levels of toxoid expression in these two candidate clones. We chose to continue the immunization studies with the fully plant-optimized clone NT#3, with the consideration that toxoid expression in other plant types may require such optimization.
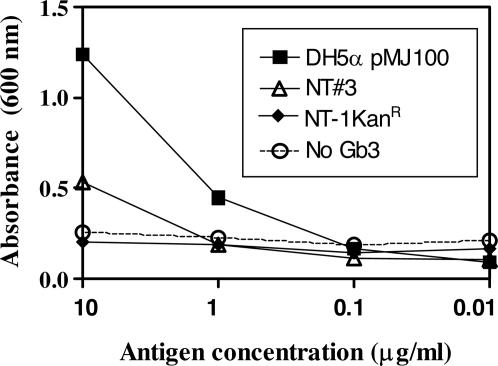
A Gb3-based ELISA was used to determine whether the plant-derived toxoid subunits assembled into the native holotoxin configuration. Because the N terminus of the A subunit is critical for pentamerization of the B subunits (22) and the B pentamer of Stx binds Gb3 (23), antibody specific to the A subunit of Stx2 was used to verify the binding of both toxin components to Gb3. We observed a positive reaction, in a dose-dependent fashion, with lysates from NT#3 (Fig. 3). From that finding, we concluded that the tobacco-cell-expressed A and B subunits were associated.
Fig. 3.
Assessment of plant-derived Stx2 holotoxoid assembly by the Gb3-binding assay. Serially diluted sonic lysates of E. coli DH5α (pMJ100) that expressed wild-type Stx2, NT#3, or NT-1KanR were added to Gb3-coated wells. Wells without Gb3 were also treated with E. coli DH5α (pMJ100) to serve as controls for nonspecific binding by Stx2. The experiment was done in triplicate, and each datum point represents the mean value of replicates ± 1 SD.
Immunogenicity of Plant-Derived Toxoid.
To first assess whether the plant-derived toxoid was functionally immunogenic against Stx2, we compared the immune responses in mice immunized i.p. with either the plant-derived toxoid or a plasmid-encoded, E. coli-derived toxoid known to be protective against Stx2 (24). The geometric mean titers of Stx2-neutralizing antibody from animals immunized with plant- or E. coli-derived toxoid were 46 and 356, respectively. Despite this nearly 10-fold difference, the titers from these i.p.-immunized mice were significantly higher than those of groups mock-immunized with NT-1KanR or with E. coli that carried the pBluescribe vector alone. Furthermore, 10 of 10 mice immunized with the plant-derived toxoid and 8 of 8 mice immunized with E. coli-derived toxoid survived a parenteral challenge of 10 times the LD50 (10 LD50) of Stx2. None of the mock-immunized animals survived such a challenge.
Oral Immunization with Transgenic Tobacco Cells.
Preliminary studies were done to determine the optimal NT-1 toxoid dose, feeding conditions, and boosting schedule. Sera collected after these different vaccination regimes were assessed by ELISA to detect Stx2-specific IgG (data not shown). The vaccination strategies for each immunization group are presented in Table 1. The strategy for group A, in which mice were fed plant material once per week for 5 weeks, was found to consistently elicit anti-Stx2 antibody and, therefore, was adopted for the remaining experiments. In addition, a prime–boost strategy that combined an initial i.p. immunization with plant extract, followed by two oral feedings of NT-1 cells that expressed Stx2 toxoid (group C), was adopted based on the success of such a strategy in eliciting an improved response to enterohemorrhagic E. coli intimin and the heat-labile enterotoxin B subunit of enterotoxigenic E. coli in similar studies (13, 25).
Table 1.
Oral immunization groups and protocols
| Group | Immunization protocol |
|---|---|
| A. Oral | 5 g of NT#3 cells fed on days 0, 7, 14, 21, and 28 |
| B. Mock oral | 5 g of NT-1KanR cells fed on days 0, 7, 14, 21, and 28 |
| C. Prime–boost | Sonic lysate from 0.5 g of NT#3 + TiterMax i.p. on day 0; 5 g of NT#3 cells fed on days 21 and 28 |
| D. Prime–mock boost | Sonic lysate from 0.5 g of NT#3 + TiterMax i.p. on day 0; 5 g of NT-1KanR cells fed on days 21 and 28 |
| E. Mock prime–mock boost | Sonic lysate from 0.5 g of NT-1KanR + TiterMax i.p. on day 0; 5 g of NT-1KanR cells fed on days 21 and 28 |
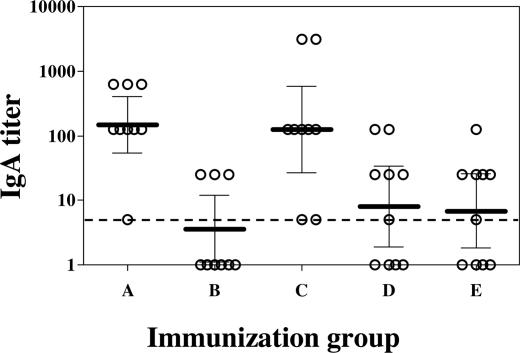
Fecal anti-Stx2 IgA was detected by ELISA. The geometric mean IgA titer of group A was statistically significantly higher than that of the mock-immunized group B (Fig. 4), and all mice in group A produced detectable anti-Stx2 IgA. We concluded that elevated fecal IgA titers in the immunized mice reflected a mucosal immune response. Although the geometric mean IgA titer of group C (parenterally primed and orally boosted) was not statistically significantly higher than the geometric mean IgA titers of groups D (parenterally primed and mock orally boosted) and E (mock primed and mock boosted), the observed differences were noticeable. Furthermore, all of the mice in group C produced detectable levels of anti-Stx2 IgA, whereas only 6 of 10 mice in group D did. No difference was observed between groups D and E; a finding that suggested that i.p. priming did not enhance development of a mucosal immune response. Of note, both groups B and E were immunized with NT-1KanR only, yet some mice in these groups showed anti-Stx2 fecal antibodies. Although purified Stx2 was used to coat the microtiter plates, it is not unusual to have some residual E. coli products in such toxin preparations (24). We suspect that the mock-immunized mice had antibodies against components of E. coli found among the gut flora that recognized such antigens in the purified recombinant Stx2, and that those antibodies contributed to background titers in these ELISAs.
Fig. 4.
Stx2-specific fecal IgA as measured by ELISA. Each circle represents the IgA titer of an individual mouse; the bar represents the geometric mean of the titers obtained from the group. The dashed line indicates the limit of detection, and the error bracket represents the 95% confidence interval. Unpaired t tests were performed between group pairs (see Table 1): A–B (P < 0.05), C–D (P > 0.05), C–E (P > 0.05), and D–E (P > 0.05).
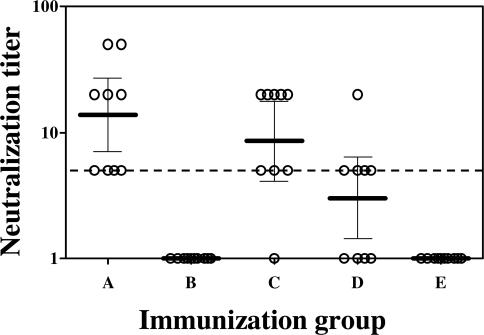
A more correlative in vitro indicator of the protective immune response is the toxin neutralization in the Vero cell cytotoxicity assay (38). The production of Stx2-neutralizing antibodies was assessed by incubation of mouse sera with wild-type Stx2 and the subsequent neutralization of Vero cell cytotoxicity by Stx2-specific antibodies in immune sera (Fig. 5). None of the mock orally immunized mice produced detectable Stx2-neutralizing antibodies, whereas all of the orally immunized mice showed evidence of toxin-neutralizing antibodies. Furthermore, all of the mice in group A were responders. The prime–boost method was also effective in eliciting production of neutralizing antibodies. The significantly higher neutralization titer of group C (i.p.-primed and orally boosted) compared with group D (i.p.-primed and mock orally boosted) showed that oral feeding was important in eliciting the systemic response. Nonetheless, those mice that received only the parenteral plant extract vaccine (group D) showed a statistically significant neutralization titer compared with the mock-immunized mice (group E) (P < 0.05).
Fig. 5.
Neutralization of Stx2 Vero cell cytotoxicity with mouse antisera. Each circle represents the neutralization titer of the serum from an individual mouse. The dashed line represents the limit of detection. The bar represents the geometric mean of neutralization titers obtained from each group, and the error bracket represents the 95% confidence interval. Unpaired t tests were performed between group pairs (see Table 1): A–B (P < 0.05), C–D (P < 0.05), C-E (P < 0.05), and D–E (P < 0.05).
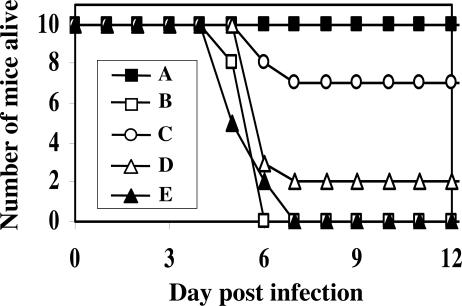
To examine the protective efficacy of the plant-based toxoid vaccine against Shiga intoxication during an orally acquired STEC infection, the streptomycin-treated mouse model was used. In that model, infection with STEC is established through reduction of normal intestinal flora by pretreatment of mice with streptomycin (15). In our study, mice were so treated and then fed a streptomycin-resistant isolate of E. coli serotype O91:H21 strain B2F1 that produces the highly toxic Stx2d-activatable variant of Stx2. Results are shown in Fig. 6. All of the mice in immunization group A survived challenge with B2F1. The prime–boost group C was partially protected (70% survival rate), whereas only 20% of the mice in group D that received only one i.p. immunization with plant-derived toxoid survived. None of the mock-immunized mice from groups B and E survived infection with B2F1. Deaths occurred between 5 and 7 days after infection, a pattern that is consistent with previous observations in our laboratory. Therefore, no delay in time to death was notable among the immunized mice.
Fig. 6.
Survival of streptomycin-treated mice after systemic toxin challenge by oral infection with B2F1. Letters in the legend box indicate immunization groups (Table 1). Statistical analysis was done on day 12 after oral infection to compare between groups A–B, C–D, C–E, and D–E by using Fisher’s exact test (P < 0.05).
Discussion
Our strategy for development of a safe and effective anti-Stx2 vaccine was to start with a genetically inactivated StxA2 subunit and to preserve the holotoxin structure by inclusion of the B subunit, to maximize the epitopes available for immunization. Previous work has shown that the StxA2 subunit elicits protective antibody production in animals, whereas the StxB2 subunit alone does not (26, 27). This result is probably attributable to the requirement for the A2 portion (N terminus) of the StxA2 subunit for pentamerization and proper presentation of the StxB2 binding domain (22). In addition, we suspect that StxA2 is immunodominant to StxB2, from our recent observation that anti-StxB2 antibodies are not detected in mice that are immunized parenterally with Stx2 holotoxoid, yet the mice are protected by Stx2 toxin challenge (24). Nonetheless, because of the important role of the StxB2 pentamer in binding Gb3 on susceptible cells, we chose to incorporate both the A toxoid and B subunits into the plant-based vaccine.
The expression of Shiga AB5 holotoxins in bacteria is achieved through transcription of a single mRNA that encodes the stxA and stxB genes, followed by translation initiated at two separate ribosomal binding sites. The site at which translation of the B subunit begins is stronger than the A subunit binding site, which accounts for the synthesis of more B than A proteins from the Stx transcript. To express the Stx2 toxoid in plants, two distinct ORFs (each with the cauliflower mosaic virus 35S promoter) were constructed, but no provision was made for enhanced expression of the B subunit. Western blot analysis showed that both subunits were produced in detectable amounts in NT-1 cells, but proportionally more StxA2 was expressed than StxB2. Because the A subunit is a larger protein, it may have provided more antigenic epitopes recognizable by polyclonal antibodies than did the B subunit. It is also likely that the B subunit was not expressed in excess of A, as seen in bacteria, because the dual-expression cassettes used the same strong promoter. In NT-1 cells, a protein of the expected size of StxA2 was detected, but a larger band of equal intensity was also seen by Western blotting. We suspected that StxA2 was modified by glycosylation, as was observed when the bacterial protein intimin was expressed in NT-1 cells (13). An examination of the stxA2 sequence revealed three potential Asn-linked glycosylation sites at eukaryotic N-X-S/T motifs. Furthermore, enzymatic deglycosylation specific for the N- and O-linked sugar residues reduced the size of the larger A subunit protein bands (data not shown). Another explanation for this observed larger StxA2 protein is that the bacterial signal peptidase cleavage site in the A subunit may not be consistently recognized and cleaved in eukaryotic cells, as suggested by Yu and Haslam (28). Nonetheless, the toxoid structure was immunogenic and provided systemic protection against Stx2-producing bacteria.
Although it is not possible to be sure that plant-derived toxoid has the native conformation without direct evidence from crystallography, we demonstrated association of the plant-derived toxoid A and B subunits by using a Gb3-based ELISA. Less plant-derived holotoxoid was detected by Gb3 ELISA than was bacterially derived toxoid. This reduction may be indicative of less-efficient assembly of plant-derived holotoxoid because subunits were not synthesized in the optimal 1A:5B ratio. Another explanation is that detection of holotoxoid with anti-StxA2 antibody was reduced because of glycosylation of the A subunit.
To test the immunogenicity of the plant-derived toxoid, we first administered plant extracts i.p. to mice and found that the mice were protected against lethal toxin challenge. Then, the transformed plant material was given orally over several feedings, and protection against challenge with a lethal oral infection of STEC was achieved. In contrast to other work (29), the prime–boost approach of combined parenteral and oral immunization did not seem to have a benefit in this study. In fact, the prime–boost method was shown to be less protective than the feeding method alone. However, the parenteral priming was effective by comparison between the prime–mock boost group (D) and the negative control group (E). Similarly, the two oral boosts were effective, as shown by the comparison between groups C and D. These results, taken together, suggest that the suboptimal level of protection afforded by the prime–boost method probably reflects the fact that the prime–boost group received fewer boosts overall than the orally vaccinated mice. Others have shown that prime–boost strategy in reverse order (oral priming followed by i.p. boosts) has worked well to elicit systemic immunity (30). However, multiple parenteral boosts would defeat one of our initial goals in development of a plant-based vaccine, which was to minimize the use of needles.
Some mice in the mock-immunized groups (B and E) exhibited fecal antibodies that were reactive by ELISA. This finding raises an important consideration for the evaluation of orally administered vaccines in general. The gut provides an effective but very nonselective path by which to introduce antigens. Production of fecal antibodies may indicate sensitization to the immunizing antigen or a nonspecific reaction to previously encountered related antigens. Here, fecal IgA titers did not necessarily predict the development of a protective response against the systemic effects of Stx2. In contrast, the Vero cell cytotoxicity neutralization assay, a functional assay conducted with sera that represented a broader antibody class response, was far more indicative of in vivo protection.
Although subunits of other bacterial toxins of the AB5 family, such as heat-labile toxin of enterotoxingenic E. coli and cholera toxin of Vibrio cholerae, have been expressed in plant systems for vaccine purposes (31, 32), we know of no precedent for the expression of an AB5 holotoxoid of bacterial origin in a plant system. In contrast to heat-labile toxin and cholera toxin that act locally at the gastrointestinal level where mucosal immunization is most likely to be effective, Stxs enter the circulation and act systemically to target tissues that express Gb3. Therefore, systemic immunity is needed to protect against hemolytic uremic syndrome. The streptomycin-treated mouse model of STEC infection is not completely representative of human STEC infection because mice do not experience diarrhea and they suffer renal tubular damage as opposed to the glomerular necrosis seen in humans. Nonetheless, the prevention of deaths, the usual outcome of such an infection in mice, serves as proof-of-concept that oral immunization with Stx2 toxoid administered by means of plant-based vaccine is protective against systemic toxin-mediated disease. Additional steps are needed to prepare Stx2 holotoxoid for use as an oral plant-based vaccine for humans. A more suitable host plant, such as tomatoes or bananas, would be desirable, and different promoters would likely be required for optimal expression in other fruits or vegetables. In addition to fresh plant-based vaccines, dried or lyophilized plant materials also provide a good vaccine vehicle in which antigens are stably preserved and concentrated (9). By reducing the mass of the plant vaccine, such as by encapsulating the material into pill form, oral intake would be easier and uniform doses would be better controlled. Moreover, the inclusion of a similar Stx1 toxoid would be necessary to provide protection against Stx- and Stx1-producing organisms such as Shigella dysenteriae type 1 and many other STECs, respectively. A composite approach to plant vaccines against several diarrheal agents would be ideal. We feel that the systemic immunity against Stx2 that we observed indicates that an oral plant-based vaccine shows promise for protection against the severe, sometimes life-threatening, consequences of STEC infection, against which no other suitable treatments or therapies are currently available.
Materials and Methods
Plant-Optimization of Stx2 Toxoid Genes.
The Stx2 toxoid gene was derived from pNR100 (24). Three additional mutations were introduced to eliminate the destabilization motifs in the stxA2 region, with the mutagenic primers listed in Table 2 (which is published as supporting information on the PNAS web site). The plant-optimized StxA2 toxoid subunit gene was amplified by PCR with primers designed to introduce 5′ XbaI (GGAACACCTCTAGATGAAGTG) and 3′ SacI (GCTGAGCTCCTTTATTTACCCG) sites flanking the stxA2PO. The XbaI–SacI fragment was cloned into pIBT210 (33) to create pNAJ65. The entire stxB2 was resynthesized by ligase chain reaction (Table 2) and ligated into the NcoI–SmaI site of pBTI210.3 (13) to create pNAJ73. The sequence of stxB2PO was submitted to the GenBank database (accession no. DQ231140).
Construction of Plant Expression Vectors.
Two dual-expression cassettes were designed (Fig. 1). First, pNAJ65, which contained stxA2PO, was restriction-digested to obtain a HindIII–SacI fragment. Second, pNAJ73, which contained the synthetic stxB2PO, was digested to obtain a PstI–EcoRI fragment. Third, pRT38 (34), which contained the potato proteinase inhibitor II gene (pin2), was digested to obtain a SacI–PstI fragment. Fourth, pGPTV-Kan was digested with HindIII and EcoRI. All four fragments were ligated together to yield pSW3 (Fig. 1). To evaluate the effect of plant-optimization, a second dual-expression cassette (pSW2) was generated. That cassette contained stxA2PO and the native stxB2 and was constructed in a similar fashion to pSW3.
Agrobacterium-Mediated Transformation of NT-1 Cells.
The method used for transformation of NT-1 cells was originally described by An (34). In brief, pSW2 or pSW3 was electroporated into A. tumefaciens strain EHA105 (35). The resulting strains of A. tumefaciens were then used to transform NT-1 cells as described by Judge et al. (13). Transformed NT-1 cells were selected on kanamycin-containing 50 μg/ml NT medium.
Immunoblot Analysis.
Plant-derived Stx2 toxoid expression was assessed by Western blot analysis, as described (13). Rabbit anti-Stx2 polyclonal antibodies at a titer of 10,000 were used as the primary antibody. Quantitation of Stx2 toxoid produced per gram of NT-1 cells was extrapolated from a standard curve in which pixel density, measured by nih image v.1.61 software (http://rsb.info.nih.gov/nih-image), was plotted against known concentrations of Stx2 (36).
Gb3 Binding Assay.
The Gb3 binding assay described by Ashkenazi and Cleary (23) was used to check assembly of the plant-derived Stx2 holotoxoid. Gb3 (Matreya, State College, PA) dissolved in chloroform/methanol (2:1) was used to coat 96-well ELISA plates (VWR Scientific, Bridgeport, NJ) at 1 μg per well. Wells were blocked with 5% (wt/vol) BSA in 0.05% Tween/PBS, and serially diluted NT-1 or E. coli sonic lysates were added. The primary antibody, a monoclonal anti-Stx2, 11E10 (16), was diluted 1:1,000, and a horseradish peroxidase-conjugated goat anti-mouse IgG (Bio-Rad, Richmond, CA) served as the secondary antibody (37). The antigen–antibody reaction was detected by absorbance at 600 nm.
Parenteral Immunization of Mice.
Female 3- to 4-wk-old BALB/c mice (Charles River Laboratories, Wilmington, MA) in groups of 10 received i.p. injections on days 0 and 21 with 50 μl of cell extract from NT#3, NT-1KanR, E. coli that harbored pNR100, or E. coli that carried the pBluescribe vector alone. Toxoid concentrations were standardized to 1 μg of toxoid per immunization, and the samples were mixed with an equal volume of TiterMax Gold (TiterMax USA, Norcross, GA) adjuvant for administration. Serum samples were collected before and after immunization from tail veins to monitor the production of Stx2-neutralizing serum antibodies. Mice were challenged on day 35 by i.p. injection of 20 μg of Stx2 (≈10 LD50).
Oral Immunization and Infection of Mice.
The immunization protocols are shown in Table 1. Female 3- to 4-wk-old BALB/c mice in five groups of 10 were individually fed 5 g of NT-1 cells (≈30 μg of Stx2 toxoid) mixed with 0.5 g of sucrose. The prime–boost groups first received an i.p. injection of NT-1 cell extract that contained 1 μg of toxoid with adjuvant, as described above, and then were fed NT-1 cells. Serum and fecal pellets were collected before immunization and 7 days after the last dose and tested for Stx2-neutralizing serum antibody and Stx2-specific fecal IgA. On day 41 after initial immunization, all mice were fasted overnight and given streptomycin-containing water (5 g/liter). The next day, they were fed 106 colony-forming units of a spontaneously derived streptomycin-resistant mutant of E. coli strain B2F1 (8).
Serum Neutralization Assay.
The presence of Stx2-neutralizing antibody in serum samples was assessed by the Vero cell cytotoxicity neutralization assay as described in refs. 24 and 38.
Stx2-Specific Fecal IgA and Serum IgG ELISA.
Fecal extracts were prepared in PBS and standardized by weight, as described (13). ELISA plates were coated with purified native Stx2 (100 ng per well). Fecal extracts were serially diluted 10-fold, applied to the Stx2-coated plates, and incubated at 37°C for 2 h. Horseradish peroxidase-conjugated rabbit anti-mouse IgA (Bio-Rad) was used as the secondary antibody. The antigen–antibody reaction was detected as described for the Gb3 binding assay. Titers were defined as the reciprocal of the highest dilution of postimmune fecal extract that contained Stx2-specific antibodies, as determined by optical densities greater than those seen with preimmune fecal extract and blank wells that contained all reagents except fecal extract. Serum anti-Stx2 IgG was also detected by ELISA as described above, except that horseradish peroxidase-conjugated goat anti-mouse IgG (Bio-Rad) was used as the secondary antibody.
Supplementary Material
Acknowledgments
We thank Dr. Hugh S. Mason (Arizona State University) for valuable input in designing the plant constructs and providing the plant expression vectors, as well as for critical review of the manuscript. This work was supported by National Institutes of Health Grant 2R01AI20148-23 and Uniformed Services University of the Health Sciences Grant HO73KD.
Abbreviations
- STEC
Shiga toxin-producing Escherichia coli
- Stx
Shiga toxin
- Gb3
globotriaosyl ceramide
- NT-1
Nicotiana tabacum cell line.
Footnotes
Conflict of interest statement: No conflicts declared.
This paper was submitted directly (Track II) to the PNAS office.
Data deposition: The sequence reported in this paper has been deposited in the GenBank database (accession no. DQ231140).
References
- 1.Mead P. S., Slutsker L., Dietz V., McCaig L. F., Bresee J. S., Shapiro C., Griffin P. M., Tauxe R. V. Emerg. Infect. Dis. 1999;5:607–625. doi: 10.3201/eid0505.990502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Griffin P. M., Tauxe R. V. Epidemiol. Rev. 1991;13:60–98. doi: 10.1093/oxfordjournals.epirev.a036079. [DOI] [PubMed] [Google Scholar]
- 3.Furutani M., Ito K., Oku Y., Takeda Y., Igarashi K. Microbiol. Immunol. 1990;34:387–392. doi: 10.1111/j.1348-0421.1990.tb01019.x. [DOI] [PubMed] [Google Scholar]
- 4.Donohue-Rolfe A., Jacewicz M., Keusch G. T. Mol. Microbiol. 1989;3:1231–1236. doi: 10.1111/j.1365-2958.1989.tb00273.x. [DOI] [PubMed] [Google Scholar]
- 5.Jacewicz M., Clausen H., Nudelman E., Donohue-Rolfe A., Keusch G. T. J. Exp. Med. 1986;163:1391–1404. doi: 10.1084/jem.163.6.1391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Strockbine N. A., Marques L. R., Newland J. W., Smith H. W., Holmes R. K., O’Brien A. D. Infect. Immun. 1986;53:135–140. doi: 10.1128/iai.53.1.135-140.1986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Downes F. P., Barrett T. J., Green J. H., Aloisio C. H., Spika J. S., Strockbine N. A., Wachsmuth I. K. Infect. Immun. 1988;56:1926–1933. doi: 10.1128/iai.56.8.1926-1933.1988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wadolkowski E. A., Sung L. M., Burris J. A., Samuel J. E., O’Brien A. D. Infect. Immun. 1990;58:3959–3965. doi: 10.1128/iai.58.12.3959-3965.1990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Tacket C. O. Expert Opin. Biol. Ther. 2004;4:719–728. doi: 10.1517/14712598.4.5.719. [DOI] [PubMed] [Google Scholar]
- 10.Streatfield S. J., Howard J. A. Expert Rev. Vaccines. 2003;2:763–775. doi: 10.1586/14760584.2.6.763. [DOI] [PubMed] [Google Scholar]
- 11.Cimolai N. Can. J. Microbiol. 2001;47:691–697. [PubMed] [Google Scholar]
- 12.Streatfield S. J. Immunol. Cell Biol. 2005;83:257–262. doi: 10.1111/j.1440-1711.2005.01335.x. [DOI] [PubMed] [Google Scholar]
- 13.Judge N. A., Mason H. S., O’Brien A. D. Infect. Immun. 2004;72:168–175. doi: 10.1128/IAI.72.1.168-175.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ito H., Terai A., Kurazono H., Takeda Y., Nishibuchi M. Microb. Pathog. 1990;8:47–60. doi: 10.1016/0882-4010(90)90007-d. [DOI] [PubMed] [Google Scholar]
- 15.Lindgren S. W., Melton A. R., O’Brien A. D. Infect. Immun. 1993;61:3832–3842. doi: 10.1128/iai.61.9.3832-3842.1993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Melton-Celsa A. R., Rogers J. E., Schmitt C. K., Darnell S. C., O’Brien A. D. Jpn. J. Med. Sci. Biol. 1998;51(Suppl.):S108–S114. doi: 10.7883/yoken1952.51.supplement1_s108. [DOI] [PubMed] [Google Scholar]
- 17.Edwards A. C., Melton-Celsa A. R., Arbuthnott K., Stinson J. R., Schmitt C. K., Wong H. C., O’Brien A. D. In: Escherichia coli O157:H7 and Other Shiga Toxin-Producing E. coli Strains. Kaper J. B., O’Brien A. D., editors. Washington, DC: Am. Soc. Microbiol.; 1998. pp. 388–392. [Google Scholar]
- 18.Adang M. J., Brody M. S., Cardineau G., Eagan N., Roush R. T., Shewmaker C. K., Jones A., Oakes J. V., McBride K. E. Plant Mol. Biol. 1993;21:1131–1145. doi: 10.1007/BF00023609. [DOI] [PubMed] [Google Scholar]
- 19.Perlak F. J., Fuchs R. L., Dean D. A., McPherson S. L., Fischhoff D. A. Proc. Natl. Acad. Sci. USA. 1991;88:3324–3328. doi: 10.1073/pnas.88.8.3324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Newman T. C., Ohme-Takagi M., Taylor C. B., Green P. J. Plant Cell. 1993;5:701–714. doi: 10.1105/tpc.5.6.701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Becker D., Kemper E., Schell J., Masterson R. Plant Mol. Biol. 1992;20:1195–1197. doi: 10.1007/BF00028908. [DOI] [PubMed] [Google Scholar]
- 22.Haddad J. E., Jackson M. P. J. Bacteriol. 1993;175:7652–7657. doi: 10.1128/jb.175.23.7652-7657.1993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ashkenazi S., Cleary T. G. J. Clin. Microbiol. 1989;27:1145–1150. doi: 10.1128/jcm.27.6.1145-1150.1989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Wen S. X., Teel L. D., Judge N. A., O’Brien A. D. Vaccine. 2005;24:1142–1148. doi: 10.1016/j.vaccine.2005.08.094. [DOI] [PubMed] [Google Scholar]
- 25.Lauterslager T. G., Florack D. E., van der Wal T. J., Molthoff J. W., Langeveld J. P., Bosch D., Boersma W. J., Hilgers L. A. Vaccine. 2001;19:2749–2755. doi: 10.1016/s0264-410x(00)00513-2. [DOI] [PubMed] [Google Scholar]
- 26.Padhye V. V., Zhao T., Doyle M. P. J. Med. Microbiol. 1989;30:219–226. doi: 10.1099/00222615-30-3-219. [DOI] [PubMed] [Google Scholar]
- 27.Marcato P., Mulvey G., Read R. J., Vander H. K., Nation P. N., Armstrong G. D. J. Infect. Dis. 2001;183:435–443. doi: 10.1086/318080. [DOI] [PubMed] [Google Scholar]
- 28.Yu M., Haslam D. B. Infect. Immun. 2005;73:2524–2532. doi: 10.1128/IAI.73.4.2524-2532.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kong Q., Richter L., Yang Y. F., Arntzen C. J., Mason H. S., Thanavala Y. Proc. Natl. Acad. Sci. USA. 2001;98:11539–11544. doi: 10.1073/pnas.191617598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Devico A. L., Fouts T. R., Shata M. T., Kamin-Lewis R., Lewis G. K., Hone D. M. Vaccine. 2002;20:1968–1974. doi: 10.1016/s0264-410x(02)00080-4. [DOI] [PubMed] [Google Scholar]
- 31.Mason H. S., Haq T. A., Clements J. D., Arntzen C. J. Vaccine. 1998;16:1336–1343. doi: 10.1016/s0264-410x(98)80020-0. [DOI] [PubMed] [Google Scholar]
- 32.Arakawa T., Chong D. K., Merritt J. L., Langridge W. H. Transgenic Res. 1997;6:403–413. doi: 10.1023/a:1018487401810. [DOI] [PubMed] [Google Scholar]
- 33.Haq T. A., Mason H. S., Clements J. D., Arntzen C. J. Science. 1995;268:714–716. doi: 10.1126/science.7732379. [DOI] [PubMed] [Google Scholar]
- 34.An G. Plant Physiol. 1985;79:568–570. doi: 10.1104/pp.79.2.568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Hood E. E., Gelvin S. B., Melchers L. S., Hoekma A. Transgenic Res. 1993;2:208–218. [Google Scholar]
- 36.Sinclair J. F., O’Brien A. D. J. Biol. Chem. 2002;277:2876–2885. doi: 10.1074/jbc.M110230200. [DOI] [PubMed] [Google Scholar]
- 37.Perera L. P., Marques L. R., O’Brien A. D. J. Clin. Microbiol. 1988;26:2127–2131. doi: 10.1128/jcm.26.10.2127-2131.1988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Gentry M. K., Dalrymple J. M. J. Clin. Microbiol. 1980;12:361–366. doi: 10.1128/jcm.12.3.361-366.1980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Weinstein D. L., Jackson M. P., Perera L. P., Holmes R. K., O’Brien A. D. Infect. Immun. 1989;57:3743–3750. doi: 10.1128/iai.57.12.3743-3750.1989. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.