Abstract
Background
Only about a third of people with asthma attend an annual review. Clinicians need to identify cost-effective ways to improve access and ensure regular review.
Aim
To compare the cost-effectiveness of nurse-led telephone with face-to-face asthma reviews.
Design of study
Cost-effectiveness analysis based on a 3-month randomised controlled trial.
Setting
Four general practices in England.
Methods
Adults due an asthma review were randomised to telephone or face-to-face consultations. Trial nurses recorded proportion reviewed, duration of consultation, and abortive calls/missed appointments. Data on use of healthcare resources were extracted from GP records. Cost-effectiveness was assessed from the health service perspective; sensitivity analyses were based on proportion reviewed and duration of consultation.
Results
A total of 278 people with asthma were randomised to surgery (n = 141) or telephone (n = 137) review. One-hundred-and-one (74%) of those with asthma in the telephone group were reviewed versus 68 (48%) in the surgery group (P <0.001). Telephone consultations were significantly shorter (mean duration telephone = 11.19 minutes [standard deviation {SD} = 4.79] versus surgery = 21.87 minutes [SD = 6.85], P < 0.001). Total respiratory healthcare costs per patient over 3 months were similar (telephone = 64.49 [SD = 73.33] versus surgery = 59.48 [SD = 66.02], P = 0.55). Total costs of providing 101 telephone versus 68 face-to-face asthma reviews were also similar (telephone = 725.84 versus surgery = 755.70), but mean cost per consultation achieved was lower in the telephone arm (telephone = 7.19 [SD = 2.49] versus surgery = 11.11 [SD = 3.50]; mean difference = −3.92 [95% confidence interval = −4.84 to 3.01], P < 0.001).
Conclusions
Telephone consultations enable a greater proportion of asthma patients to be reviewed at no additional cost to the health service. This mode of delivering care improves access and reduces cost per consultation achieved.
Keywords: asthma, cost-effectiveness, primary care, telephone
INTRODUCTION
Regular review of people with asthma improves morbidity and is a key recommendation of the British Thoracic Society/Scottish Intercollegiate Guidelines Network guideline on asthma management.1,2 However, despite the provision of proactive care within general practice, only about a third of people with asthma attend for their annual review appointments.3,4 Practices will need to respond to this challenge by developing efficient services that improve access to care.
In a trial comparing telephone with face-to-face reviews, we demonstrated that use of the telephone can increase the proportion of asthma patients reviewed from 48% to 74%, an improvement of 26% (95% confidence interval [CI] = 14% to 37%).5 The significantly shorter duration of telephone consultations (mean duration = 11.19 versus 21.87 minutes; 95% CI = 12.59 to 8.77; P <0.001) suggests that this model of delivering routine asthma care may be an efficient strategy, reflected in cost savings for the health service. Asthma-related quality of life and morbidity at 3 months were similar and patients were equally satisfied with the consultations.
We report here a cost-effectiveness analysis performed from the perspective of the health service on data from this trial, which aims to compare the overall cost of respiratory care, the total cost of providing the review service, and the cost per consultation achieved in the two groups.
How this fits in
Regular review of people with asthma is an evidence-based recommendation of the British Thoracic Society/Scottish Intercollegiate Guidelines Network guideline on asthma management, and reflects good clinical practice. Despite the provision of proactive care in UK general practice, only around one-third of patients with asthma attend their annual review in the asthma clinic. Nurse-led telephone consultations can cost-effectively increase the proportion of patients reviewed when compared with face-to-face consultations (74% versus 48%), at an average saving of 3.92 per consultation achieved. Sensitivity analyses suggest that the cost-effectiveness of telephone consultations is a robust finding that is potentially generalisable beyond the four practices involved in this study.
METHOD
Trial procedures
The trial was undertaken during 2001 with the fully informed consent of all participants. Full details of the trial procedure are published elsewhere.5 In summary, symptomatic asthma patients (defined as patients who had requested a prescription for a bronchodilator inhaler in the previous 6 months) who had not been reviewed in the previous 12 months were recruited from four UK general practices and centrally randomised to telephone review or face-to-face consultation with the asthma nurse.
Participants reported symptoms consistent with a broad spectrum of asthma severity, and were using treatment plans reflecting the range of recommended therapeutic steps.2 Nurses made up to four attempts to call patients in the telephone-review group. Patients in the surgery-review group were invited to make an appointment in the nurse-led asthma clinic in the usual way. The content of the review consultation and follow-up arrangements were at the nurses' discretion according to clinical need, excluding a telephone option for patients in the surgery group. Trial nurses collected data on the use of healthcare resources by searching electronic and paper general practice records at the end of the 3-month study period. A researcher, blinded to allocation, visited each of the practices and validated a random 20% sample of consultation data and data retrieved from records.
Costs and resource use
Costs were assessed from the perspective of the health service. Data on healthcare resource use were available at an individual patient level. Health service costs were calculated using unit cost estimates from published UK sources6-9 multiplied by the use of healthcare resources recorded during the 3-month trial. Unit costs for each intervention are listed in Table 1; parameters included:
trial asthma review consultations (including nurse time and telephone costs for the timed duration of consultations). It was noted whether calls were local, national, or made to mobile phones;
abortive telephone calls were recorded as well as appointments missed because patients did not attend for the surgery appointment they had booked;
primary care consultations with GPs or practice nurses (surgery, telephone and home visits, including ‘out-of-hours’) for respiratory conditions as recorded in the patients' general practice records (paper and electronic);
secondary care contacts (out-patient, accident and emergency attendances, hospital admissions) identified from patients' general practice records;
all prescriptions for respiratory drugs and devices issued during the 3-month trial identified from patients' paper and electronic records;
prescriptions for antibiotics and oral steroids given for exacerbations of asthma or ‘chest infections’.
Table 1.
Unit costs and sources.
| Unit | Cost/unit (£) | Source | |
|---|---|---|---|
| Trail asthma reviews | |||
| Asthma specialist practice nurse | Personal Social Services Research Unit6 | ||
| Clinic time | 1 minute | 0.48 | |
| Non-attendance | 21.87 minutesa | 10.50 | |
| Abortive calls | 2 minutesb | 0.96 | |
| Telephone costs (peak rates) | British Telecom7 | ||
| British Telecom local rate | 1 minute | 0.04 | |
| British Telecom national rate | 1 minute | 0.08 | |
| Average mobile rate | 1 minute | 0.18 | |
| Healthcare professionals | |||
| GP | Personal Social Services Research Unit6 | ||
| Surgery consultation | 9.4 minutes15 | 19.00 | |
| Telephone consultation | 4.7 minutesc | 9.69 | |
| GP visit (including travel time) | 25.2 minutes | 59.00 | |
| Practice nurse | Personal Social Services Research Unit6 | ||
| Clinic consultation | per consultationd | 10.00 | |
| Telephone consultation | per consultatione | 5.40 | |
| Hospital costs | |||
| Respiratory out-patients | per out-patient clinic | 88.00 | Personal Social Services Research Unit6 |
| Prescribing costs | |||
| Bronchodilators | per inhaler, device, or tablet | British National Formulary9 | |
| Inhaled steroids | |||
| Add-on therapyf | |||
| Combination inhalersg | |||
| Antibiotics (for chest infections) | |||
| Devices (peak flow meters, spacers) | |||
| Prednisolone (for acute asthma) | |||
Prices are in £ sterling for the year 2000–2001.
Mean duration of surgery reviews.5
Estimated time for an abortive call.
Assuming the telephone consultation at half the duration of a surgery consultation + telephone cost at £0.04/minute.
Assuming 20-minute clinic appointments.
Assuming the telephone consultation at half the duration of a surgery consultation + telephone cost at £0.04/minute.
Long-acting bronchodilators, leukotriene receptor antagonists, theophyllines, anticholinergics, cromones.
Combination inhalers: inhaled steroids + long-acting β2 agonists.
A number of assumptions were made in order to estimate costs and resource use. We estimated the time taken for each abortive call as 2 minutes, based on a sample of unsuccessful calls. The time wasted if a patient did not attend a surgery appointment they had made was assumed to be equal to the mean duration for face-to-face consultations in our trial. These costs were added to the total costs of telephone or surgery consultations.
Telephone consultations undertaken by GPs or nurses outside the timed trial reviews were assumed to be half the length of average surgery consultations. This is based on the recognised tendency, substantiated by our trial, for telephone consultations to be shorter than face-to-face reviews.5,10 All costs are in pounds sterling (£) for the year 2000–2001.
Outcome measures
Our primary outcome measure was the proportion of patients with asthma reviewed within 3 months of randomisation. Details of the consultation, including abortive attempts at telephone calls, missed appointments, and the duration of the consultation, were noted immediately after the review onto a piloted consultation record. We also assessed asthma-related quality-of-life, asthma morbidity, and consultation satisfaction using validated instruments.5,11-13
Statistical analyses
Data were analysed using SPSS version 10. Mean healthcare costs were calculated and compared with independent sample t-tests. The use of mean costs is now recommended for economic evaluations of pragmatic randomised controlled trials, as despite the usual skewness in the distribution of cost data, the arithmetic mean is the most economically meaningful descriptive statistic.14 In contrast, other summary measures do not provide the information needed to inform health policy decisions, such as the total cost of treating all patients. Standard t-tests and t-test based CIs are adequate in most realistic situations for comparing mean costs.14
Sensitivity analysis
The two parameters most likely to influence the cost-effectiveness to the health service are the proportion reviewed and the duration of the consultation. To test the robustness of our data, sensitivity analyses were performed using the 95% CIs for these parameters, and data was extrapolated to include likely extremes. In our calculation of the cost per telephone consultation achieved, we included the cost of abortive calls. We calculated the cost per surgery consultation in two ways: firstly including the cost of non-attendances as ‘wasted’ nurse time and, secondly, omitting the cost of non-attendance on the assumption that the nurse would be able to use his/her time constructively.
RESULTS
Of the 278 patients recruited to the trial, 137 were allocated to telephone reviews and 141 to surgery reviews. Baseline characteristics were comparable.5
Overall cost of respiratory care
The cost of respiratory care over the 3-month trial is shown in Table 2. In short, there were no significant differences in overall healthcare resource use, the cost of consultations, or drug use.
Table 2.
Overall healthcare costs per patient for respiratory care over the 3 months of the trial.
| Mean cost in £ sterling (SD) | Telephone (n = 137) | Surgery (n = 141) | Difference (95% CI) | P-value |
|---|---|---|---|---|
| Cost of trial asthma consultation | 5.30 (2.94) | 5.36 (6.00) | −0.06 (−1.18 to 1.06) | 0.91 |
| Cost of trial nurse | 4.95 (2.70) | 5.36 (6.00) | −0.41 (−1.51 to 0.69) | 0.46 |
| Telephone costs | 0.35 (0.32) | NA | ||
| Overall respiratory healthcare costs (including trial consultation) | 64.49 (73.33) | 59.48 (66.02) | 5.01 (−11.45 to 21.48) | 0.55 |
| Healthcare delivery costs (including trial consultation) | 11.42 (19.44) | 11.21 (16.10) | 0.21 (−4.00 to 4.42) | 0.92 |
| Primary care costs: | ||||
| GP | 3.47 (10.81) | 4.40 (12.60) | −0.93 (−3.70 to 1.85) | 0.51 |
| Nurse (excluding trial consultation) | 1.37 (4.10) | 1.46 (3.90) | −0.09 (−1.04 to 0.85) | 0.85 |
| Secondary care costs: | ||||
| Out-patient attendance | 1.28 (15.04)a | 0 | 1.28 (−1.21 to 3.78) | 0.31 |
| Inpatient | 0 | 0 | ||
| Accident and emergency visit | 0 | 0 | ||
| Drugs | 53.08 (66.81) | 48.27 (61.11) | 4.81 (−10.30 to 19.92) | 0.53 |
| Bronchodilators | 4.24 (7.69) | 4.11 (5.42) | 0.13 (−1.44 to 1.70) | 0.87 |
| Inhaled steroids | 27.31 (33.27) | 28.00 (36.93) | −0.69 (−8.99 to 7.62) | 0.87 |
| Add-on therapy | 20.09 (43.60) | 11.26 (30.26) | 8.83 (−0.01 to 17.67) | 0.05 |
| Combinationsb | 0.58 (6.73) | 4.08 (26.45) | −3.50 (−8.09 to 1.08) | 0.13 |
| Antibiotics | 0.29 (1.24) | 0.46 (1.77) | −0.17 (−0.54 to 0.19) | 0.34 |
| Devices | 0.51 (1.69) | 0.28 (1.25) | 0.22 (−0.13 to 0.57) | 0.21 |
| Oral steroids | 0.07 (0.38) | 0.08 (0.42) | −0.01 (−0.11 to 0.08) | 0.79 |
One patient who had two outpatient visits.
Combinations of inhaled steroids and a long-acting β2 agonist. NA = not applicable.
Total cost of the asthma review services
The costs to practices of providing the asthma review services are shown in Table 3. The total cost was similar for each group: telephone €725.84 versus surgery €755.70. Therefore, on an intention-to-treat basis, there was no significant difference in the mean costs per eligible patient.
Table 3.
Cost to the practices of providing the asthma review services.
| Cost in £ sterling | Telephone n = 137 | Surgery n = 141 | Difference (95% CI) | P-value |
|---|---|---|---|---|
| Total nurse costs | 677.76 | 755.70 | ||
| Telephone costs | 48.08 | 0 | ||
| Total cost of abortive calls/non-attendersa | 135.36 | 52.49 | ||
| Total cost of trial consultations (£) | 725.84 | 755.70 | ||
| Mean cost of trial consultation per eligible patient (SD) [Intention to treat analysis] | 5.30 (2.94) | 5.36 (6.00) | −0.06 (−1.18 to 1.06) | 0.914 |
| Mean cost of trial consultation per consultation achieved (SD) [101 telephone consultations versus 68 surgery consultations] | 7.19 (2.49) | 11.11 (3.50) | −3.92 (−4.84 to −3.01) | <0.001 |
Abortive call/did-not-attend cost/consultation achieved was calculated as follows: telephone group, cost of 141 abortive calls at 2 minutes of nurse time (£0.48/min) = £135.36; surgery group, cost of five did-not-attends at 21.87 minutes of nurse time (£0.48/min) = £52.49. SD = standard deviation.
Cost per consultation achieved
As more patients achieved a review in the telephone group, the cost per consultation achieved was significantly lower for telephone consultations: telephone = 7.19 (SD = 2.49) per consultation versus surgery = 11.11 (SD = 3.50); mean difference = −3.92 (95% CI = −4.84 to 3.01) P <0.001 (Table 3).
Sensitivity analyses
Sensitivity analyses were undertaken based on the 95% CIs for the proportion reviewed in each group (Supplementary Table 1) and the duration of consultation for telephone and surgery consultations (Supplementary Table 2). In all scenarios, the cost per consultation achieved favoured the telephone review. In cases of missed appointments, if it is assumed that the nurse will be able to make use of the available time so that the cost of non-attendance is taken to be zero, the cost saving is between 2.38 and 4.30. (Supplementary Table 2). Combining the least favourable scenarios from both analyses (lowest telephone review rate + longest calls versus highest surgery review rate + shortest consultations) estimated a cost saving per consultation of 2.87. Combining the most favourable scenarios from both analyses (highest telephone review rate + shortest calls versus lowest surgery review rate + longest consultations) estimated a cost saving per consultation of 5.36.
Further sensitivity analyses confirm the cost-effectiveness of telephone consultation across a wide range of proportions reviewed and duration of consultation (Figures 1 and 2).
Figure 1.
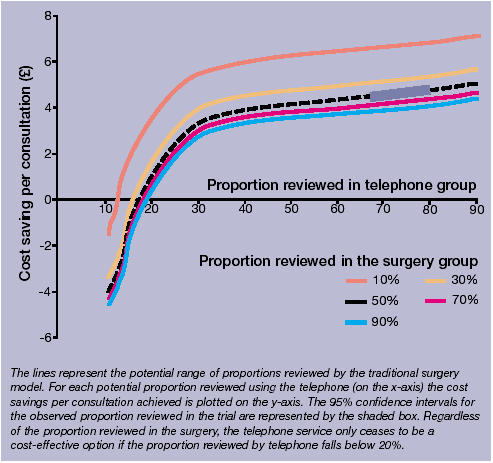
Sensitivity analysis I: Cost saving per consultation achieved by telephone compared to proportion reviewed in the surgery.
Figure 2.
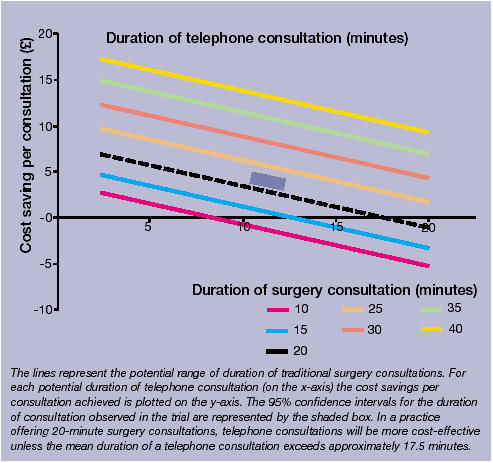
Sensitivity analysis II: Cost saving per consultation achieved by duration of telephone consultation compared to duration of surgery review.
DISCUSSION
Summary of main findings
Our trial demonstrates that telephone consultations for the nurse-led routine review of asthma cost-effectively increased the proportion of people receiving a review, saving an average of 3.92 per consultation achieved. The total cost of providing the asthma review service and the overall cost of providing respiratory care was the same in both groups.
Strengths and limitations of the study
Several factors limit the generalisability of our findings.5 Our study population (a third of those invited to participate) were slightly older than the total eligible population, although the sex ratio was similar. In addition, we focused on patients with ‘active’ asthma who we defined as having requested a bronchodilator inhaler in the previous 6 months. Patients using even less medication may be even more reluctant to attend the surgery for a review, possibly increasing the advantage of opportunistic phone calls. Our nurses were all experienced in providing asthma care, which may have affected the efficiency with which they undertook reviews both in the surgery and on the telephone.
The short duration of our study may have reduced the chance of demonstrating a difference between the two groups in total respiratory care costs. Even a small difference in the number of patients requiring emergency care over the subsequent year could substantially affect outcomes over a longer timeframe, although this seems unlikely as asthma control was similar in both groups at 3 months.5 Furthermore, any effect (for example, on drug usage or follow-up reviews) would be likely to have occurred soon after the consultation and dissipate over the subsequent months. Self-management education, which is known to reduce morbidity,1 was provided in two-thirds of reviews in both groups, potentially favouring the telephone group for whom more consultations were achieved.5 Extending the duration of follow-up may have allowed more consultations to be achieved in both groups. This may have affected the costs of undertaking the trial reviews, but our sensitivity analyses suggest that this would not have altered our conclusions.
A major strength of our study is that we had detailed individual patient data collected from the general practice records, which should have ensured a comprehensive assessment of healthcare costs over the trial period. Our quality control check validated the accuracy of data transfer.5
Comparison with existing literature
Shorter duration is the principle factor influencing the cost-effectiveness of telephone consultations in our trial. This has been described previously10,15 and probably reflects the recognised tendency for telephone interactions to be more focussed and less subject to digressions, while achieving the same tasks.16 Despite the different duration, telephone and surgery asthma reviews appear to cover a similar content and are equally effective and acceptable,5 stimulating speculation about the dynamics of these different modes of consultation and their potential role in providing routine care for patients with chronic disease.
There are possible disadvantages of telephone contacts with some reports suggesting that telephone triage of requests for same-day appointments may lead to an increase in subsequent surgery consultations and, therefore, costs — perhaps because the focused telephone call did not deal with all of the issues that the patient hoped to address.10,17 This may be less important in routine telephone reviews as the need for a consultation is clinician led.
The British Asthma Guideline recommendation that people with asthma should be reviewed regularly in primary care focuses attention on the importance of ensuring an efficient recall service.2 Currently, around one third of people with asthma are reviewed annually.3-5 Use of the telephone offers the potential to increase cost-effectively the review rate towards the 74% achieved in our trial. The sensitivity analyses suggest that the cost-effectiveness of telephone consultations is a robust finding applicable within a wide range of proportions reviewed and duration of consultation and, therefore, potentially generalisable beyond the four UK practices involved in the trial. These findings will be of interest to practices seeking to increase the efficiency of their asthma reviews within the constraints of a primary care service with little spare capacity.18
Telephone consultations enable a greater proportion of asthma patients to be reviewed at no additional cost to the health service. This mode of delivering care, therefore, not only improves access but also reduces cost per consultation achieved. A telephone option, as part of an asthma review service, has the potential to increase access to asthma care cost-effectively.
Supplementary Material
Acknowledgments
This study was originally developed at a research meeting of the General Practice Airways Group, which was organised by Mark Levy and funded by an educational grant from AstraZeneca. Jane Scullion undertook quality control visits to the practices. Victoria Madden was the lay advisor. The study was undertaken by Robert Bawden and Frances Yates, Botesdale Health Centre, Diss; Dr Stephen Proctor and Carol Howard, Clarendon Medical Centre, Hyde; Stephanie Wolfe, Thorpewood Surgery, Norwich; and Caroline Snellgrove, Kathy Ellis and Toni Bowey, Whitstable Health Centre, Whitstable.
Supplementary information
Additional information accompanies this article at http://www.rcgp.org.uk/journal/index.asp
Ethics committee and reference number
South East Multi-Centre Research Ethics Committee (MREC 00/1/17), and Local Research Ethics Committees: East Kent (LREC 0109/08/00), Tameside and Glossop (LREC O/385), West Suffolk (LREC 00/059), Norwich District (LREC 2000/168M)
Funding body and reference number
British Lung Foundation (Grant No P00/9). AS was supported by an NHS/PPP National Primary Care Award
Conflicts of interest
None
REFERENCES
- 1.Gibson PG, Powell H, Coughlan J, et al. The Cochrane Library. Issue 4. Chichester: John Wiley and Son; 2004. Self-management education and regular practitioner review for adults with asthma (Cochrane Review) [DOI] [PubMed] [Google Scholar]
- 2.The British Thoracic Society/Scottish Intercollegiate Guideline Network. British guideline on the management of asthma. Thorax. 2003;58(S1):i1–94. doi: 10.1136/thorax.58.suppl_1.1i. http://www.sign.ac.uk/guidelines/fulltext/63/index.html (accessed 10 Jan 2005) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Price D, Wolfe S. Delivery of asthma care: patient's use of and views on healthcare services, as determined from a nationwide interview survey. Asthma J. 2000;5:141–144. [Google Scholar]
- 4.Gruffydd-Jones K, Nicholson I, Best L, Connell E. Why don't patients attend the asthma clinic? Asthma in General Practice. 1999;7:36–38. [Google Scholar]
- 5.Pinnock H, Bawden R, Proctor S, et al. Accessibility, acceptability, and effectiveness in primary care of routine telephone review of asthma: pragmatic, randomised controlled trial. BMJ. 2003;326:477–479. doi: 10.1136/bmj.326.7387.477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Netten A, Dennett J, Knight J. Unit costs of health and social care 2001. Canterbury: University of Kent at Canterbury Personal Social Services Research Unit; 2001. [Google Scholar]
- 7.British Telecom. Call charges for 2001. http://www.serviceview.bt.com/list/current/docs/Gen_Notes.boo/0001.htm (accessed Dec 2002)
- 8.29th Report 2000, Cm4562. London: The Stationery Office; 2000. Review body on Doctor's and Dentist's remuneration. [Google Scholar]
- 9.British Medical Association. British national formulary. London: British Medical Association and Royal Pharmaceutical Society of Great Britain; 2001. Royal Pharmaceutical Society of Great Britain. [Google Scholar]
- 10.McKinstry B, Walker J, Campbell C, et al. Telephone consultations to manage requests for same-day appointments: a randomised controlled trial in two practices. Br J Gen Pract. 2002;52:306–310. [PMC free article] [PubMed] [Google Scholar]
- 11.Juniper EF, Guyatt GH, Cox FM, et al. Development and validation of the Mini Asthma Quality of Life Questionnaire. Eur Respir J. 1999;14:32–38. doi: 10.1034/j.1399-3003.1999.14a08.x. [DOI] [PubMed] [Google Scholar]
- 12.Rimmington LD, Aronoffsky L, Mowatt A, et al. Use of a simple patient focussed asthma morbidity score. Eur Resp J. 1997;10:194. [Google Scholar]
- 13.Poulton BC. Use of the consultation satisfaction questionnaire to examine patients' satisfaction with general practitioners and community nurses: reliability, replicability and discriminant validity. Br J Gen Pract. 1996;46:26–31. [PMC free article] [PubMed] [Google Scholar]
- 14.Thompson SG, Barber JA. How should cost data in pragmatic randomised trials be analysed? BMJ. 2000;320:1197–2000. doi: 10.1136/bmj.320.7243.1197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Jiwa M, Mathers N, Campbell M. The effect of GP telephone triage on numbers seeking same-day appointments. Br J Gen Pract. 2002;52:390–391. [PMC free article] [PubMed] [Google Scholar]
- 16.Rutter DR. Communicating by telephone. Oxford: Pergamon Press; 1987. [Google Scholar]
- 17.Richards DA, Meakins J, Tawfik J, et al. Nurse telephone triage for same day appointments in general practice: multiple interrupted time series trial of effect on workload and costs. BMJ. 2002;325:1214. doi: 10.1136/bmj.325.7374.1214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Chisholm J. BMA, General Practitioners Committee annual report 2003. London: British Medical Association; 2003. A message from the Chairman. www.bma.org.uk/ap.nsf/Content/GPCannrep03 (accessed 10 Dec 2004) [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


