Abstract
Context
Vitamin K acupuncture point injection, a menstrual pain treatment derived from traditional Chinese medicine, has been a standard treatment in some hospitals in China since the 1980s.
Objectives
To investigate the effects of vitamin K acupuncture point injection on menstrual pain in young women aged 14 to 25 from different countries and cultural backgrounds who have had unmitigated severe primary dysmenorrhea for 6 months or more
Design
Prospective, observational, clinical pilot study
Settings
One site in China (a hospital outpatient clinic in Shanghai) and 2 sites in Italy (a hospital clinic in Milan and a private gynecology practice in Verona)
Interventions
All subjects were treated with bilateral acupuncture point injection of vitamin K on the first or second day of menstrual pain. Vitamin K3 was used in China and vitamin K4 in Italy.
Main Outcome Measures
Pain intensity, total duration, and average intensity of menstrual distress, hours in bed, normal daily activity restrictions, and numbers of analgesic tablets taken to relieve pain were recorded before the treatment and for 4 subsequent menstrual cycles.
Results
Noticeable pain relief was observed 2 minutes after treatment, and subsequent pain reduction occurred at 30 minutes (P < .001). Subjects reported significantly fewer daily life restrictions, fewer hours in bed, less consumption of analgesic tablets, and lower scores of menstrual pain duration and intensity (P < .001). There were no adverse events. Some women experienced mild, self-limited pain at the injection site.
Conclusion
Acupuncture point injection with vitamin K alleviated acute menstrual pain, and relief extended through the nontreatment follow-up cycles in this uncontrolled pilot study conducted in 2 countries. Further investigation employing controlled experimental designs is warranted.
Introduction
Dysmenorrhea is a common gynecologic complaint. A systematic review of the prevalence of chronic pelvic pain summarizing both community and hospital surveys estimated the prevalence in the United Kingdom to range from 45% to 95%.[1] Reports focus on adolescent girls and generally include only primary dysmenorrhea, although this is not always specified. Studies of North American women younger than 24 years of age cite prevalences ranging from 52% to 93% (5% to 18% severe).[2] A big cooperative study that includes more than 130,000 Chinese women of any age have reported a 33% prevalence (13.5% severe).[3] Searching MEDLINE on October 16, 2004, using the keywords "dysmenorrhea" and "Europe, Italian," we found no articles reporting prevalence estimates for dysmenorrhea in Italian women.
Dysmenorrhea has been reported to be one of the most common causes of periodic absenteeism from school or work in young women.[4] Oral nonsteroidal anti-inflammatory drugs (NSAIDs) are at least partly effective in relieving primary dysmenorrhea in about 90% of sufferers and completely effective in 55% to 70%.[5] Oral contraceptives (OCs) are also prescribed for controlling primary dysmenorrhea.[6,7] However, both treatments have side effects, and their use is not without risk.[5] Some women prefer not to use NSAIDs or OCs because of side effects or for personal or cultural reasons.
Only a few articles on the use of acupuncture for the management of menstrual pain exist in Western languages.[8,9] We found 340 publications in the Chinese literature from January 2001 to September 2004 on the treatment of dysmenorrhea with acupuncture, 150 of which have randomized and controlled designs, indicating that acupuncture is a common treatment for menstrual pain in China.
Acupuncture point injection with vitamin K3 is the standard treatment for severe dysmenorrhea in the Menstrual Disorder Clinic of the Department of Integration of Western and Traditional Medicine, Obstetrics & Gynecology Hospital, Fudan University, Shanghai, Peoples Republic of China -- one of the sites where the present pilot study was executed. The department staff uses a combination of disease diagnosis with traditional Chinese medicine (TCM) pattern diagnosis to treat women's disorders with herbs, acupuncture, and Western medicine. Investigators in the department have particular expertise in the effects of TCM on neuroendocrine and immune system function. Researchers at the Menstrual Disorder Clinic first reported that vitamin K3 injection in muscle could relieve primary dysmenorrhea within 30 minutes, that relief continued as vitamin K3 seemed to relax uterine muscle spasm caused by noradrenaline or prostaglandin (PG) F2alpha, and that vitamin K3 injection at an acupuncture point (San Yin Jiao/Spleen 6) could relieve menstrual pain more quickly than in muscle.[10,11]
Acupuncture point injection -- the injection at an acupuncture point of a small amount of a drug, vitamin, saline, or plant extract -- is a recent innovation of traditional acupuncture and aims to enhance and prolong the effect of stimulation of acupuncture points.
The proposed advantages of this technique, as cited in the Chinese literature,[12] are as follows:
Dose reduction of therapeutic agent of injection when compared with usual (oral or intramuscular) modes of administration
Synergistic augmentation of effect of acupuncture point stimulation and agent of injection
Ability to standardize and replicate treatment (which is difficult with classic acupuncture)
The degree to which acupuncture point injection is used to treat menstrual pain in outpatient clinics throughout the rest of China is unknown.
The San Yin Jiao/Spleen 6 acupuncture point is located on the leg, above the inner malleolus, in a depression on the inner-posterior border of the tibial bone. This acupuncture point is widely used for gynecologic indications, including menstrual disorders, menstrual pain, vaginal discharge, urinary retention, induction of labor, acceleration of labor, retention of placenta, and others.[13,14] Acupuncture points are stimulated by inserted needles; by heat generated from a rolled, cured herb burned close to the point (moxibustion); by manual pressure; or, as in the case of this trial, by injecting an agent, intramuscularly, at the site.[15] The location of the acupuncture point San Yin Jiao/Spleen 6 allows for an intramuscular injection.
The aims of this pilot study were to investigate the effects of vitamin K acupuncture point injection on menstrual pain in patients with severe primary dysmenorrhea from different countries and cultural backgrounds, collect preliminary data useful for the design of subsequent multicenter international studies on the same topic, and verify the utility of measurement instruments in different populations.
Materials and Methods
Subjects and Sites of the Study
Forty women with severe primary dysmenorrhea of at least 6 months' duration were recruited and consented to participate in the study; 20 were patients at the outpatient Menstrual Disorder Clinic, Shanghai, China (see above), and 20 were patients at either of 2 sites in Italy -- a hospital clinic in Milan and a private gynecology practice in Verona. Subjects were healthy, nulliparous, 14 to 25 years of age, and had no history or evidence of pathology by pelvic examination. None were using or wanted to use OCs or intrauterine devices. Severe dysmenorrhea was defined as "severe recurrent menstrual pain, with or without general accompanying symptoms, that interrupts normal activities for hours or days and that is not relieved, or not totally relieved, by any previous treatment." Women taking other concomitant therapy for acute or chronic pain due to any cause, receiving treatment with anticoagulant drugs for any reason, or previously treated with vitamin K acupuncture point injection at the San Yin Jiao/Spleen 6 acupuncture point for any reason were excluded.
Intervention
Women who met the inclusion criteria were asked to come to the outpatient clinic during the first day of menstrual pain of their next period. The subject's skin around the San Yin Jiao/Spleen 6 acupuncture point was sterilized, a 22-gauge syringe needle was inserted at the point, and 4 mg of vitamin K3 (menadione sodium bisulfite) was injected bilaterally at the San Yin Jiao/Spleen 6 point at the treatment site in China, and 5 mg of vitamin K4 (menadiol sodium diphosphate) at the 2 centers in Italy. The solution volume of injection was 1 mL per side for each injection. After the injection was administered, the needle was pulled and the acupuncture point was pressed with sterilized pads to prevent infection.
Women were allowed to request an additional treatment for 1 subsequent cycle, for any reason, so some women received the treatment twice.
The study was approved by Human Subjects/Ethical Committees in Shanghai and in Milan before enrollment of subjects began.
Outcome Measures
The short-term effect of the treatment on pain intensity was assessed using a 0- to 10-cm visual analogue pain scale (VAS) before the treatment, and at 2 minutes, 5 minutes, and 30 minutes after the vitamin K injection treatment.
A Retrospective Symptom Scale of Menstrual Distress[16] was selected to evaluate menstrual pain and distress because of its conciseness and simplicity, and because the investigators thought it suitable for use in 2 different social and cultural contexts. The list of symptoms was modified slightly from the original to simplify it and allow better comprehension. The subjects assigned a number from 0 to 4 (0 = not at all, 4 = worst possible) to a list of symptoms experienced during the previous menstrual cycle. The instrument was translated from English to Chinese and Italian and was used for assessing the total duration (Cox 1 score) and average intensity (Cox 2 score) of menstrual distress for a total of 5 cycles (pretreatment cycle, treatment cycle, and 3 post-treatment follow-up cycles). Hours spent in bed, normal daily activity restrictions, and numbers of analgesic tablets or herbal treatments taken were also recorded. Participants could self-administer their preferred treatments for pain (NSAIDs tablets or herbal tablets or decoctions) if they needed to. Side effects were recorded.
Statistics
A student t-test was used to compare mean values of VAS, hours spent in bed, number of NSAID tablets, Cox 1 (pain duration), and Cox 2 (pain intensity). Chi-square tests were used to compare the Chinese and the Italian groups and to compare the women treated once with the women treated twice. Analysis of repeated measures was used to test trends over the follow-up period. In order to test the probability of having a second treatment during the follow-up, 2 survival curves were built and a log-rank test was used to compare the Italian and Chinese groups. Interpolation curves were built in order to estimate the trend of intensity and duration of menstrual pain for the post-treatment period. The statistical processing was performed using SPSS 10.0 for Windows.
Results
Enrollment
By February 2002, 20 women had been enrolled at each site. All Chinese subjects completed the study by September 2002, and all Italian subjects completed the study by April 2003, except 1, who withdrew from the study after 3 cycles because she wished to take OCs. The flow diagram of participants is shown in (Table 1).
Table 1.
Flow Diagram of Participants
| Chinese Subjects (n) | Italian Subjects (n) | |
|---|---|---|
| Completed pretreatment assessment | 20 | 20 |
| Received the first treatment | 20 | 20 |
Received a second treatment:
|
8 0 4 4 |
8 6 1 1 |
| Lost at follow-up | 0 | 0 |
| Withdrawals | 0 | 1 |
Baseline Menstrual Distress Characteristics
(Table 2) shows the baseline menstrual distress characteristics in Chinese and Italian women. There were no statistically significant differences in daily activities, hours in bed, Cox scores for pain duration and intensity, and oral treatments with herbs between Chinese and Italian subjects. The mean number of analgesic tablets taken in China and in Italy was significantly different (P < .001), with Italian women ingesting more.
Table 2.
Baseline Menstrual Distress Characteristics Between Chinese and Italian Women
| Subjects | Daily activities | Hours in Bed | Cox Score 1 (Duration of Pain) |
Cox Score 2 (Intensity of Pain) |
Analgesic Tablets | Consumption of Herbs |
|
|---|---|---|---|---|---|---|---|
| n (%) | Mean ± SD | Mean ± SD | Mean ± SD | Mean ± SD | n (%) | ||
| Limited | Suspended | ||||||
| Chinese (n = 20) |
6 (30) | 14 (70) | 11.9 ± 8.9 | 23.7 ± 5.0 | 19 ± 5.7 | 2.4 ± 2.2* | 9 (45) |
| Italian (n = 20) |
5 (25) | 15 (75) | 9.0 ± 7.5 | 23.8 ± 7.6 | 20.6 ± 8.8 | 5.3 ± 2.6* | 6 (30) |
* P < .001
Treatment Effect on Acute Pain
The VAS trends from before treatment to 30 minutes after for both groups are shown in Figure 1. Because of misunderstandings between the Chinese and the Italian research teams on instructions to participants, the first measure (VAS at baseline) is not comparable. In China, the baseline VAS refers to the most severe pain ever felt before the treatment. In Italy, the baseline VAS refers to the pain intensity immediately before treatment. The mean VAS 2 minutes after the treatment was similar (China 4.1, Italy 4.8). In both countries, the highest pain reduction occurred 30 minutes after the treatment, and the test for trend of repeated measures shows a highly significant (P < .001) decrease in mean VAS scores from one measure to the next.
Figure 1.
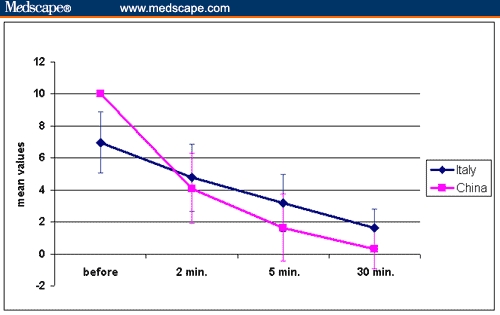
Visual analog pain scale values of the first treatment, in Chinese and Italian subjects (n = 40).
In China, analysis of VAS values at 2, 5, and 30 minutes showed a mean decrease of 2 points at each measure. Seventeen Chinese women (85%) had no pain (VAS = 0) 30 minutes after the treatment. In Italy, the mean VAS reduction from each measure to the next one was 1.8 points. Four Italian women (20%) had no pain (VAS = 0) 30 minutes after the treatment.
Other Measures of Short-term Effects
The treatment's effect on daily activities, hours spent in bed due to pain, consumption of analgesic tablets or herbs, intensity and duration of pain (measured by the Cox scores) are summarized in (Table 3). Differences in the Chi-square test before and after treatment were significant (P < .001). Within each population, all pre/post differences were significant ("consumption of herbs" among Chinese women: P = .001; all other variables P < .001) except for "consumption of herbs" among Italian women.
Table 3.
Short-term Post-treatment (First Treatment) Results on Menstrual Distress Measures
| Subjects | Time | Daily Activities | Hours in Bed | Cox Score 1 (Duration of Pain) |
Cox Score 2 (Intensity of Pain) |
Analgesic tablets | Consumption of herbs | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n | (%) | n | (%) | n | (%) | Mean ± SD |
Mean ± SD |
Mean ± SD |
Mean ± SD |
n | (%) | ||
| Normal | Limited | Suspended | |||||||||||
|
All (n = 40) |
Before | 0 | (0.0) | 11 | (27.5) | 29 | (72.5) | 10.4 ± 8.2 |
23.7 ± 6.4 |
19.8 ± 7.3 |
3.8 ±2.8 |
15 | (37.5) |
| After | 34 | (85.0) | 6 | (15.0) | 0 | (0.0) | 0 | 5.1 ± 7.1 |
4.2 ± 6.0 |
0.3 ±1.0 |
2 | (5.0) | |
|
Chinese (n = 20) |
Before | 0 | (0.0) | 6 | (30.0) | 14 | (70.0) | 11.9 ± 8.9 |
23.7 ± 5.0 |
19.0 ± 5.7 |
2.4 ±2.2 |
9 | (45.0) |
| After | 19 | (95.0) | 1 | (5.0) | 0 | (0.0) | 0 | 2.3 ± 3.4 |
2.4 ± 3.5 |
0 | 0 | (0.0) | |
|
Italian (n = 20) |
Before | 0 | (0.0) | 5 | (25.0) | 15 | (75.0) | 9.0 ± 7.5 |
23.8 ± 7.6 |
20.6 ± 8.8 |
5.3 ±2.6 |
6 | (30.0) |
| After | 15 | (75.0) | 5 | (25.0) | 0 | (0.0) | 0 | 8.0 ± 8.7 |
6.0 ± 7.4 |
0.6 ±1.3 |
2 | (10.0) | |
Follow-up Cycles: Women Treated Once
Data from 23 subjects (12 Chinese and 11 Italian) who were treated once and completed the 3 cycles of follow-up are summarized in (Table 4), which compares each measure before the treatment and at the end of the third cycle follow-up. Significant to highly significant differences (P = .017 to P < .001) were found in "daily activities" (both groups), "hours in bed" (Chinese subjects), "Cox 1 and 2 scores" (both groups), and "analgesic tablets" (Italian subjects). Nonsignificant differences were found in "hours in bed" (Italian subjects, P = .08), "tablets taken" (Chinese subjects, P = .14), and "consumption of herbs" (all subjects P = .2, Chinese subjects P = .08, Italian subjects P = 1).
Table 4.
Results at the End of 3 Months of Follow-up (Subjects Treated Once)
| Subjects | Time | Daily Activities | Hours in Bed | Cox Score 1 (Duration of Pain) |
Cox Score 2 (Intensity of Pain) |
Analgesic tablets | Consumption of herbs | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n | (%) | n | (%) | n | (%) | Mean ± SD | Mean ± SD | Mean ± SD | Mean ± SD | n | (%) | ||
| Normal | Limited | Suspended | |||||||||||
|
All (n = 23) |
Before | 0 | (0.0) | 6 | (26.1) | 17 | (73.9) | 11.6 ± 10.3 | 24.3 ± 6.9 | 19.5 ± 7.9 | 4.3 ± 3.0 | 9 | (39.1) |
| End follow up | 5 | (21.7) | 13 | (56.5) | 5 | (21.7) | 4.4 ± 3.7 | 13.0 ± 7.7 | 10.5 ± 5.7 | 1.8 ± 2.1 | 5 | (21.7) | |
|
Chinese (n = 12) |
Before | 0 | (0.0) | 2 | (16.7) | 10 | (83.3) | 13.3 ± 11.1 | 23.2 ± 4.3 | 17.7 ± 4.3 | 2.8 ± 2.6 | 6 | (50.0) |
| After | 0 | (0.0) | 11 | (91.7) | 1 | (8.3) | 4.7 ± 3.3 | 11.8 ± 6.4 | 10.3 ± 4.9 | 1.4 ± 1.9 | 2 | (16.7) | |
|
Italian (n = 11) |
Before | 0 | (0.0) | 4 | (36.4) | 7 | (63.6) | 9.9 ± 9.7 | 25.6 ± 9.1 | 21.5 ± 10.4 | 5.9 ± 2.5 | 3 | (27.3) |
| After | 5 | (45.4) | 2 | (18.2) | 4 | (36.4) | 4.2 ± 4.2 | 14.4 ± 9.0 | 10.7 ± 6.8 | 2.2 ± 2.3 | 3 | (27.3) | |
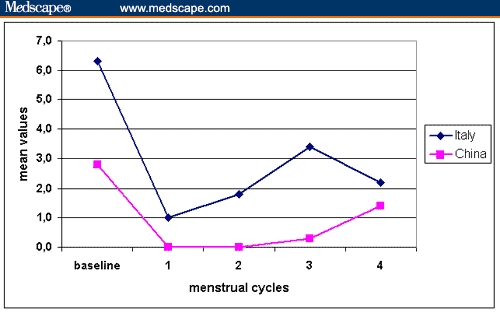
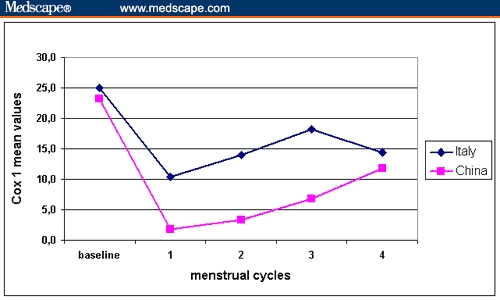
Test results for the trends of repeated measures are reported in Figures 2 through 5; they show a highly significant positive trend over the entire follow-up period for all variables. The levels of daily activities (normal, limited or suspended), the numbers of hours in bed and tablets taken, and the Cox scores 1 (duration) and 2 (intensity) decrease sharply immediately after the treatment, then go up progressively, but at the end of the follow-up remain significantly different from the baseline.
Figure 2.
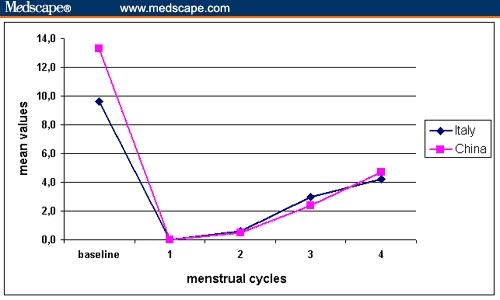
Number of hours spent in bed among subjects treated once (n = 23).
Figure 5.
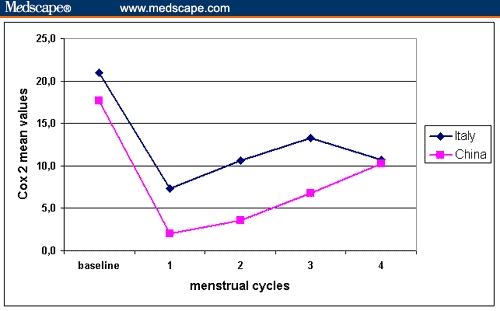
Pain intensity (Cox score 2) in subjects treated once.
Interpolation curves were estimated on the observed Cox 1 score (duration) and Cox 2 score (intensity) of menstrual pain by extrapolating the estimated scores. Figures 6 and 7 show that the Cox scores would regress to baseline at the seventh cycle post-treatment (R2 for Cox 1= 0.93 and R2 for Cox 2 = 0.92). Figures 2 through 7 account for all measures of women treated once (n = 24).
Figure 6.
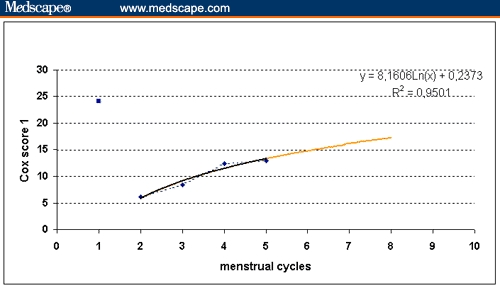
Regression to the baseline of Cox score 1 (pain duration) in subjects treated once.
Figure 7.
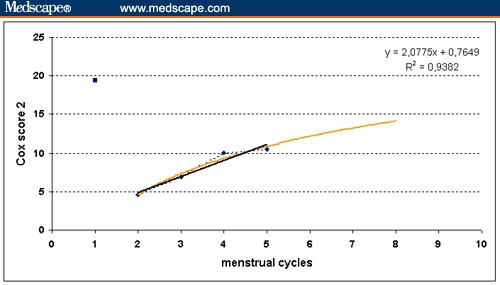
Regression to the baseline of Cox score 2 (pain intensity) in subjects treated once.
Follow-up Cycles: Women Treated Twice
Sixteen subjects (8 Chinese and 8 Italian) requested a second vitamin K acupuncture point injection treatment during the 3-month follow-up. Two survival curves were built on the event "2nd treatment" with respect to "cycle n." The log-rank test comparing the 2 survival curves for the Chinese and the Italian subjects showed no difference between the 2 groups in the probability of the event during the follow-up (P = .7). The second treatment was requested at different cycles by Chinese and Italian women (Table 1). We compared all measures in the 2 subgroups of the women treated once (n = 23) and the women treated twice (n = 16). Testing for trends of repeated measures did not show significant differences between the 2 groups with respect to hours spent in bed, the number of tablets or herbs taken, the restriction of daily activities, or the duration and intensity of menstrual pain.
Side Effects
Data on the side effects of 44 treatments were collected. The only registered discomfort was limited local pain at the site of injection, which disappeared within 1 or several hours.
The difference between the 2 populations regarding perceived pain in the lower leg after injection is significant (P = .001) (Table 5). Fourteen Italian women reported light pain vs 1 Chinese woman; 1 Italian and 1 Chinese woman reported mild pain. Only 1 participant reported severe local pain (an Italian subject). Eighteen Chinese women and 8 Italians reported no injection-site discomfort.
Table 5.
Side Effects (Local Leg Pain) of Vitamin K Acupuncture Point Injection
| None | Light | Mild | Severe | |
|---|---|---|---|---|
| n (%) | n (%) | n (%) | n (%) | |
| China (n = 20) | 18 (90) | 1 (5) | 1 (5) | 0 (0) |
| Italy (n = 24) | 8 (33) | 14 (58) | 1 (4) | 1 (4) |
Discussion
Relief of menstrual pain in patients with primary dysmenorrhea was observed both in Chinese and Italian women after vitamin K injection at the San Yin Jiao/Spleen 6 acupuncture point. A distinctive decrease from the baseline VAS when compared with the 30 minutes post-treatment measure was observed in both groups. No severe side effects or adverse events were reported. Self-reports of daily life restriction, number of analgesic tablets consumed, hours in bed due to menstrual pain, and the Cox scores for pain duration and intensity decreased significantly. Acupuncture point injection is easy to administer, and if these preliminary results are confirmed by a larger, controlled study, could provide a treatment option for severe menstrual pain in any emergency unit.
Both the Chinese and Italian data show continuing positive effects after 4-cycle follow-up in several subjects of the subgroup who were treated only once. For example, 18 of 23 subjects had less impairment of their normal daily activities. We did not record the reason women asked for a second treatment, and it is not clear how many women requested a second treatment because of relapse or because they wanted to prevent painful recurrences. This fact limits our understanding of the long-term effects of the treatment in subjects treated twice. On the other hand, as the comparison between subjects who received 1 treatment and those who received 2 treatments shows no significant difference on all outcomes, we think that it is probably not useful to repeat treatments unless there is a clear indication of relapse.
In the subgroup of women treated once, interpolation curves show that the duration and the intensity of menstrual pain (Cox scores) would regress to baseline levels at the seventh post-treatment cycle. This confirms clinical observations by authors of this paper and suggests that women with severe primary dysmenorrhea who do not wish to take OCs or NSAIDs might manage severe dysmenorrhea with 2 vitamin K acupuncture point injections per year.
Dysmenorrhea is caused by uterine ischemia, due to the contraction of the myometrium, and is associated with excessive secretion of prostaglandins.[17-19] Acupuncture at the San Yin Jiao/Spleen 6 point may affect the pelvic nerve plexus formed by T5-L1 sympathetic nerve fibers and mediate contractions of uterine myometrium.[10] Vitamin K may also relax the contractions of uterine myometrium caused by PGF2alpha.[10] Acupuncture blocks transmission of pain impulses.[20] The rapid pain relief observed after vitamin K acupuncture point injection could be the result of a synergy of multiple mechanisms. Many subjects in both China and Italy showed continuing pain relief, at least until the fourth consecutive menstrual cycle. As we know, NSAIDs and OCs do not have prophylactic multicycle treatment effects. The mechanism of continued pain relief after vitamin K acupuncture point injection is unknown; however, a study of hemorrhaghic disease found that intramuscular injection of vitamin K may have an effect for up to 2 months.[21]
Interesting differences at baseline and in the effect of treatment were observed for women in 2 cultural contexts. The consumption of NSAID analgesic tablets in China was far lower than that in Italy at baseline, during treatment, and at the end of the follow-up period (all differences ranged from significant to highly significant, except the last, P = .2). Chinese women preferred herbal preparations or decoctions and nondrug therapies to NSAID tablets.
Treatment effects on acute pain were rapid and clinically significant for women in both countries. Chinese women, however, reported more pain relief than Italian women. Different drugs were used in each country: vitamin K3 (menadione sodium bisulfite) was administered in China, whereas vitamin K4 (menadiol sodium diphosphate) was administered in Italy, because water-soluble vitamin K3 was not available in Italy. As the chemical structure of vitamin K4 is a little different from that of vitamin K3, our results raise the question of whether there is a possible difference in the effects of vitamin K3 and vitamin K4 on menstrual pain.
Range of effectiveness could also be influenced by degree of belief in the therapy and by variation in pain thresholds or cultural acceptance of pain-reporting in different cultures. The level of discomfort reported due to local pain at the injection site was significantly different in the 2 groups; this also could be due to culturally mediated differences in pain perception or reporting.
The different timing of the second treatment (Table 1)
In China, vitamin K3 acupuncture point injection was performed by an acupuncturist with more than 20 years' clinical experience in TCM. Treatment in Italy was administered by 2 gynecologists, one of whom had clinical training and experience with acupuncture and another who had had a 1-week training in acupuncture point injection technique with San Yin Jiao/Spleen 6. Skill in point location and syringe manipulation in order to get the "de Qi" (typical acupuncture sensation, thought to be important for the treatment outcome) may have influenced clinical outcomes.
Finally, the belief (unproven but common, especially in China) of a synergistic effect between acupuncture and herbs could have influenced both preference and outcomes of the rescue treatment.
In our opinion, however, beyond any speculation about the reasons for effect differences attributable to cultural factors between the 2 populations, the most important finding of the study is that the investigated treatment showed promising results in both populations.
Conclusion
Vitamin K acupuncture point injection seems to be an effective and safe treatment for primary dysmenorrhea. It may be especially useful for women who suffer adverse effects when taking OCs or NSAIDs or who prefer not to take medications. Moreover, the treatment was acceptable to the Italian women in this sample, 40% of whom requested a second treatment. This therapy may therefore be transferable from its original cultural context in China to the West. The short- and long-term efficacy and safety, comparison with placebo, and possible mechanisms of vitamin K acupuncture point injection warrant further investigation in clinical and basic science studies. Qualitative studies on the experience of painful menstruation, along with clinical experiments, should be employed to explore the effects of treatment in different populations and cultural contexts.
Figure 3.
NSAID tablets in subjects treated once (n = 23).
Figure 4.
Pain duration (Cox score 1) in subjects treated once.
Footnotes
Corresponding Author: Francesco Cardini, MD, Via Risorgimento 15, 37126 Verona, Italy. Tel +39 045 914266. Fax +39 045 8389990. Email: cardinif@internetstudio3.it
Contributor Information
Anna Laura Regalia, Obstetrics & Gynecology Department, Hospital S. Gerardo (Monza), Milano Bicocca University, Milan, Italy.
Christine Wade, The Richard and Hinda Rosenthal Center for Complementary and Alternative Medicine, Department of Rehabilitation Medicine, College of Physicians & Surgeons, Columbia University, New York, NY.
References
- 1.Zondervan KT, Yudkin PL, Vessey MP, et al. The prevalence of pelvic pain in the United Kingdom: a systematic review. Br J Obstet Gynaecol. 1998;105:93-99. [DOI] [PubMed] [Google Scholar]
- 2.Wilson M, Farquhar C. Dysmenorrhoea. In: Clinical Evidence, Issue 4. London, UK: BMJ Publishing Group; 2000. [Google Scholar]
- 3.Zhang QB, Sun XC, Tang DL, et al. Research and analysis of the menstrual physiological constants in China. Chin J Obstet Gynecol. 1980;15:219-223. [Google Scholar]
- 4.Andersch B, Milsom I. An epidemiologic study of young women with dysmenorrhea. Am J Obstet Gynecol. 1982;144:655-660. [DOI] [PubMed] [Google Scholar]
- 5.Zhang WY, Li Wanpo A. Efficacy of minor analgesics in primary dysmenorrhea: a systematic review. Br J Obstet Gynaecol. 1998;105:780-789. [DOI] [PubMed] [Google Scholar]
- 6.Robinson JC, Plichta S, Weisman CS, et al. Dysmenorrhea and use of oral contraceptives in adolescent women attending a family planning clinic. Am J Obstet Gynecol. 1992;166:578-583. [DOI] [PubMed] [Google Scholar]
- 7.Milsom I, Sundell G, Andersch B. The influence of different combined oral contraceptives on the prevalence and severity of dysmenorrhea. Contraception. 1990;42:497-506. [DOI] [PubMed] [Google Scholar]
- 8.Habek D, Habek JC, Bobic-Vukovic M, Vujic B. Efficacy of acupuncture for the treatment of primary dysmenorrhea. Gynakol Geburtshilfliche Rundsch. 2003;43:250-253. [DOI] [PubMed] [Google Scholar]
- 9.Helms JM. Acupuncture for the management of primary dysmenorrhea. Obstet Gynecol 1987;69:51-56. [PubMed] [Google Scholar]
- 10.Yu J, Chao JA. Clinical and experimental study of dysfunctional dysmenorrhea treated by vitamin K. New Drugs and Clinical Remedies. 1985;5:14-16. [Google Scholar]
- 11.Zhao WJ, Weng JE, Yu J. Clinical study of vitamin K3 acupuncture point injection in treating pelvic pain. Chinese Acupuncture & Moxibustion. 2000;20:393-394. [Google Scholar]
- 12.Luo L, Chen WJ. Development of acu-injection treatment. Journal of Clinical Acupuncture and Moxibustion. 2001;17:53-56. [Google Scholar]
- 13.Yu J. Practice and study of acupuncture in obstetrics and gynecology. In: Pan WK, ed. The Scientific and Technical Progresses of the Traditional Chinese Medicine and Pharmacology at Home and Abroad. Shanghai: Shanghai Scientific and Technical Publishing House; 1992: 142-149. [Google Scholar]
- 14.Steinberger A. The treatment of dysmenorrhea by acupuncture. Am J Chin Med. 1981;9:57-60. [DOI] [PubMed] [Google Scholar]
- 15.Li L. Literature research on point injection with Chinese Angelica liquor. J Tradit Chin Med. 1998;18:308-312. [PubMed] [Google Scholar]
- 16.Cox DJ, Meyer RG. Behavioral treatment parameters with primary dysmenorrhea. J Behav Med. 1978;3:297-310. [DOI] [PubMed] [Google Scholar]
- 17.Lundstrom V. Uterine activity during the normal cycle and dysmenorrhea. In: Dawood MY, ed. Dysmenorrhea. Baltimore, Md: Williams & Wilkins; 1981: 53-74 [Google Scholar]
- 18.Akerlund M, Bengtsson LP, Carter AM. A technique for monitoring endometrial or decidual blood flow with an intra-uterine thermister probe. Acta Obstet Gynecol Scand. 1975;54:469-477. [DOI] [PubMed] [Google Scholar]
- 19.Pickles VR, Hall WJ, Best FA, et al. Prostaglandins in endometrium and menstrual fluid from normal and dysmenorrhoeic subjects. J Obstet Gynaecol Br Commonw. 1965;72:185-192. [DOI] [PubMed] [Google Scholar]
- 20.Melzack R, Stillwell DM, Fox EJ. Trigger points and acupuncture points for pain: correlations and implications. Pain. 1977;3:3-23. [DOI] [PubMed] [Google Scholar]
- 21.Loughnan PM, McDougall PN. Does intramuscular vitamin K1 act as an unintended depot preparation? J.Padiatr Child Health. 1996;32:251-254 [DOI] [PubMed] [Google Scholar]


