Abstract
OBJECTIVE
To investigate family physicians’ views on factors that make health care decisions difficult for patients, interventions family physicians use to support patients making decisions, and interventions proposed by the Ottawa Decision Support Framework (ODSF).
DESIGN
Thirteen group discussions.
SETTING
Five family practice units.
PARTICIPANTS
One hundred twenty family physicians.
INTERVENTIONS
The multifaceted implementation intervention consisted of feedback from participants, a reminder at point of care, and an interactive workshop. During the workshop, family physicians were asked about their views on 2 videos both showing the concluding phase of a simulated clinical encounter with a woman facing a decision about hormone therapy. One video showed usual care; the other showed use of the ODSF process and related tools. Content was analyzed using observations by non-participants, field notes, material collected from participants during workshops, evaluation forms completed at the end of workshops, and comments written on exit questionnaires from the implementation trial.
MAIN OUTCOME MEASURES
Family physicians’ views on the types of difficult decisions their patients face, the factors that make decisions difficult for patients, the interventions family physicians use to support patients’ decisions, and the interventions proposed by the ODSF.
RESULTS
The 2 most frequently cited factors making decisions difficult for patients were experiencing uncertainty and fears about adverse outcomes. Before being introduced to the ODSF, participants had used mostly information-related strategies to provide decision support. After learning about the ODSF, participants overwhelmingly identified assessing patients’ values as a priority. At the end of the workshop, the 5 changes in practice participants most frequently intended to make were, in order of importance, to assess patients’ values, to ask about patients’ preferred role in decision making, to screen for decisional conflict, to assess support or undue pressure on patients, and to increase patients’ involvement in decision making.
CONCLUSION
The ODSF process and related tools have the potential to broaden family physicians’ views on supporting patients facing difficult decisions.
Abstract
OBJECTIF
Déterminer l’opinion des médecins de famille sur les facteurs qui font que les patients ont de la difficulté à prendre des décisions en matière de soins, établir les moyens utilisés par les médecins pour les assister dans ces décisions et discuter des interventions proposées par le guide Ottawa Decision Support Framework (ODSF).
TYPE D’ÉTUDE
Treize groupes de discussion.
CONTEXTE
Cinq établissements de médecine familiale.
PARTICIPANTS
Cent vingt médecins de famille.
INTERVENTIONS
Les éléments de cet essai de mise en place aux aspects multiples comprenaient les réactions des participants, un rappel en situation clinique réelle et un atelier interactif. Durant l’atelier, on demandait aux médecins de famille de commenter 2 vidéos montrant la conclusion d’une consultation fictive dans laquelle une patiente doit prendre une décision concernant l’hormonothérapie. Une des vidéos montrait la façon habituelle tandis que l’autre utilisait l’ODSF et les outils associés. Pour l’analyse du contenu, on a utilisé les observations de non-participants, les notes prises sur le vif, les documents fournis par les participants durant les ateliers et les commentaires retrouvés dans les questionnaires distribués à la fin de l’intervention.
PRINCIPAUX PARAMÈTRES ÉTUDIÉS
L’opinion des médecins concernant les types de décisions difficiles auxquels sont confrontés les patients, les facteurs qui rendent ces décisions difficiles pour les patients, les moyens utilisés par les médecins de famille pour aider les patients dans ces décisions et les interventions proposées par l’ODSF.
RÉSULTATS
L’incertitude et la crainte d’effets indésirables étaient les deux facteurs les plus fréquemment cités pour expliquer la difficulté à prendre des décisions. Avant de connaître l’ODSF, les participants avaient surtout utilisé des stratégies axées sur l’information pour guider la décision des patients. Après avoir pris connaissance de l’ODSF, ils ont en très grande majorité reconnu qu’il était primordial d’évaluer les valeurs du patient. À la fin de l’atelier, les cinq changements que les participants se proposaient le plus souvent d’adopter dans leur pratique étaient, par ordre d’importance : établir les valeurs du patient, s’informer du rôle qu’il préfère jouer dans la prise de décision, rechercher tout conflit décisionnel, évaluer le support et les pressions indues de l’entourage, et augmenter la participation du patient à la décision.
CONCLUSION
L’utilisation de l’ODSF et des outils associés est susceptible de donner aux médecins de famille une vue élargie de l’aide qu’ils peuvent apporter au patient confronté à une décision difficile.
EDITOR’S KEY POINTS.
Empirical data indicate that physicians are uncomfortable with actively engaging patients in decision making and that they have not yet adopted shared decision making.
The Ottawa Decision Support Framework was developed to guide interventions aimed at preparing patients and health care providers for shared decision making.
This study investigated family physicians’ views on the types of difficult decisions their patients face, the factors that make decisions difficult for patients, the interventions family physicians use to support patients’ decisions, and the interventions proposed by the Ottawa framework.
The 5 changes physicians most frequently intended to make in practice were to assess patients’ values, to ask for patients’ preferred role in decision making, to screen for and identify decisional conflict, to assess support or undue pressure from others, and to increase patients’ involvement in decision making.
POINTS DE REPÈRE DU RÉDACTEUR.
D’après certaines données empiriques, les médecins seraient mal à l’aise lorsqu’ils doivent encourager les patients à prendre des décisions et ils n’auraient pas encore adopté un mode de décision partagé.
Le document Ottawa Decision Support Framework (ODSF) a été conçu pour servir de guide aux interventions destinées à préparer les patients et les professionnels de la santé à collaborer ensemble à la prise de décision.
Cette étude voulait savoir ce que les médecins de famille pensent des types de décisions qui confrontent leurs patients, des interventions utilisées par les médecins pour les aider dans ces décisions et des interventions proposées par le guide ODSF.
Parmi les changements que les médecins avaient l’intention d’adopter dans leur pratique, les plus fréquemment cités étaient les 5 suivants: établir les valeurs du patient, lui faire préciser le rôle qu’il souhaite jouer dans la prise de décision, dépister et identifier les conflits décisionnels, évaluer le support et les pressions indues de l’entourage, et accroître la participation du patient à la prise de décision.
Recent years have seen the emergence of shared decision making, a process whereby decisions are shared by patients and doctors, informed by the best evidence available, and weighted in light of patients’ individual characteristics and values.1 In accordance with a patient-centred approach,2,3 shared decision making aims to enable patients “to take an active role in deciding about and planning their health care.”4,5 A systematic review of shared decision-making programs indicates that, compared with usual care or simple information leaflets, these programs performed better in terms of disseminating more information, encouraging patients to have more realistic expectations, lowering decisional conflict, increasing the proportion of people active in decision making, reducing the proportion of people remaining undecided, and fostering greater agreement between values and choice of therapy.6
The National Population Health Survey carried out in 1996-1997 revealed that 81% of Canadians visited a primary care physician at least once that year.7 In population studies dealing with the question of health decision making, Canadians indicated their desire to participate actively in the decision-making process.8 They indicated also that counseling by a physician continues to be the way they prefer to receive information before they make health decisions.9 When faced with health-related decisions, Canadians expect their physicians to have the necessary skills to ensure adequate decision support or, at least, that their physicians can direct them to trustworthy resources. Empirical data indicate, however, that physicians are uncomfortable with actively engaging patients in decision making10-13 and that they have not yet adopted the concept of shared decision making.9,11-15
It is in this context that new conceptual frameworks for shared decision making have emerged.1,16 The Ottawa Decision Support Framework (ODSF) was devised to guide development of interventions aimed at preparing patients and providers for shared decision making.16,17 The ODSF helps patients and providers make their way through a structured process of shared decision making. One of the ODSF’s important contributions is to identify decisional conflict as one of the key elements in decision making. Decisional conflict can be expressed as a state of uncertainty about which course of action to take when the choice among competing actions involves risk, loss, regret, or a challenge to personal life values.18 Identification of decisional conflict is one of the key skills taught to health care providers learning about shared decision making.1,19 Conflict can be assessed using the Decisional Conflict Scale (DCS).20
This paper reports on data collected during a large trial of implementing the ODSF in primary care. We investigated family physicians’ views on the types of difficult decisions their patients face, the factors that make decisions difficult for patients, the interventions physicians use to support patients making difficult decisions, and the interventions proposed by the ODSF.
METHODS
Study design and participants
A large before-after implementation trial of the ODSF included a qualitative assessment of family physicians’ views on the ODSF (this study), a theory-based evaluation of a multifaceted intervention to implement the ODSF and the DCS in clinical practice, and an assessment of the effect of implementing the ODSF on the agreement between physicians and their patients on the DCS. This implementation trial was conducted in 5 of 8 family practice units affiliated with one department of family medicine. Clinical teachers and residents in family medicine were the target participants. The inclusion criterion was to be involved in outpatient clinical activities at the family practice unit during the time the study was conducted. Informed consent was obtained from all clinical teachers and residents.
Data collection
During the implementation trial, the multifaceted implementation strategy comprised individual feedback, a reminder at point-of-care, and an interactive workshop. The interactive workshop offered sufficient time for a demonstration of the ODSF and a structured group discussion. The workshop was also used to collect data on participants’ views on the ODSF. The principal investigator facilitated the workshop with a cotrainer from the clinical site. After a brief introduction, participants in the workshop were asked to write down 2 difficult decisions their patients face. To elicit participants’ views on supporting patients facing difficult decisions, 2 videos showed the concluding phase of a simulated clinical encounter between a family physician and a middle-aged woman facing a decision about hormone therapy. The first video presented usual care. Participants were invited to identify factors that made the decision difficult for the woman, interventions the physician used to provide decision support, and other interventions they would have used to provide decision support.
Workshop participants were then introduced to the ODSF process and tools. After this short didactic presentation, a second video showed the same simulated encounter with the physician using the ODSF process and tools to support the woman’s decision making. Participants then discussed new interventions the physician had used to provide decision support and other interventions they would suggest.
A trained anthropologist acted as a non-participating observer at the workshops. She wrote a report after each workshop. This report included verbatim comments by participants, her perception of participants’ understanding of and interest in the material presented, and general comments on group dynamics. Within a few days of the workshop, each report was reviewed by the principal investigator, who also took field notes at the end of each workshop. After each workshop, participants completed evaluation forms on which they identified 2 changes they intended to make in practice.
Analysis and coding
The principal investigator and a research assistant analyzed the content of all reports and notes.21-23 For each workshop, both assessors independently read the written material and identified the unit of text relevant to each of the topics under study. Each unit of text was then coded according to the relevant and previously established code lists. The 2 assessors discussed any units of text that could not be coded under the established lists and created new codes if necessary, thus refining and expanding the preliminary code lists. The 2 assessors resolved any disagreements through discussion.
Codes were then aggregated into themes, and themes were aggregated into main categories. Data matrices were used to identify the point of information redundancy24; they also helped to identify variations across workshops and across family practice units.25 Categories and underlying themes were ordered according to the number of workshops in which they were identified. For each theme, specific quotations from data sources were kept for the final report to ensure that interpretations were trustworthy.24 Cotrainers and the non-participating observer were sent an interim report of the results and invited to provide feedback (member checking).24 The study was approved by the University of Ottawa’s Research Ethics Committee and the research ethics committees of the 5 institutions where the trial was conducted.
FINDINGS
Participants
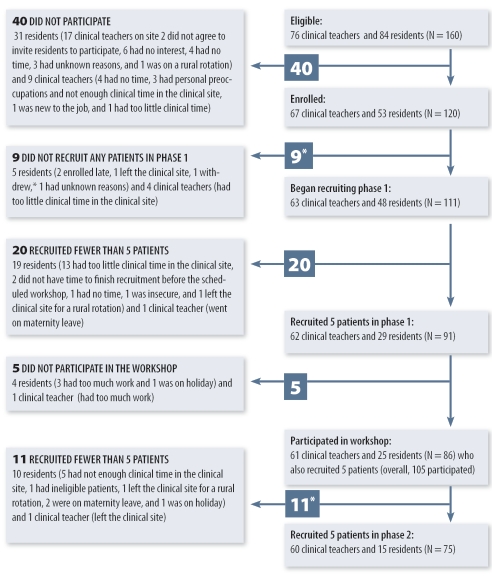
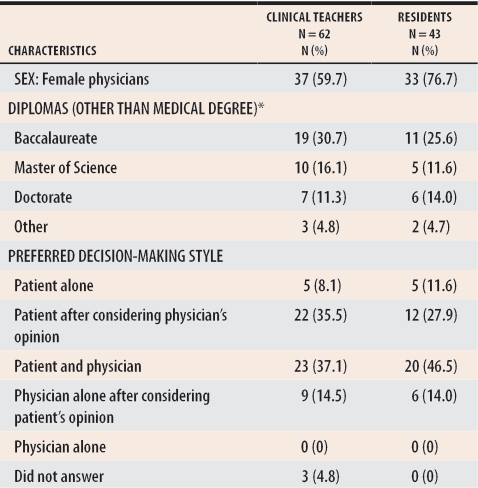
Between November 20, 2003, and March 10, 2004, 67 clinical teachers and 53 residents in family medicine enrolled in the overall implementation trial (response rate was 75%). In the only site that serves as a “Groupe de Médecine Familiale,” 1 nurse and 1 nutritionist also enrolled, so 122 providers were included in the overall trial. Figure 1 presents the flow of participants for the sample frame. Table 1 lists characteristics of the 105 physicians and residents who were enrolled in the overall trial and who participated in 1 of the workshops. Forty did not participate (9 clinical teachers and 31 residents).
Figure 1.
Flow of participants for the sample frame of family physicians
*One participant who did not recruit patients in phase 1 participated in the workshop and recruited 1 patient in phase 2.
Table 1. Characteristics of the 105 physicians who attended the workshops and were enrolled in the main implementation trial.
Physicians and residents were a mean of 41.7 (±7.3) and 28.1 (±4.9) years old, spent a mean of 43.1 (±8.7) and 44.3 (±15.4) hours in professional activities,* and saw a mean of 42.6 (±21.9) and 27.5 (±20.3) patients each week in consultation, respectively.
*Categories are not mutually exclusive.
At one site, because of organizational constraints, clinical teachers did not give permission to contact their residents (n = 17). Compared with the 120 physicians and residents participating in the study, the 23 who did not participate were more likely to be male (P = .02) but were of similar status (ie, first-year resident, second-year resident, or clinical teacher) (P = .06). When compared with the clinical teachers who participated (n = 67), the 9 who did not participate were more likely to have been in practice for 30 years or more rather than less than 30 years (P = .02). We collected 115 individual evaluation forms because all providers from each family practice unit were invited to the workshop even if they were not enrolled in the overall trial. Of the 121 exit questionnaires collected at the end of the implementation trial, 41 contained participants’ written comments.
Difficult decisions and views on supporting patients
No new information was provided after the eighth workshop. Cancer therapy was the only difficult decision that was mentioned in all 13 workshops; antidepressant drug therapy was mentioned in 12. Level of care, lifestyle issues, screening tests, and hormone therapy were the next most frequently mentioned difficult decisions. There was consensus among participants that the first video reflected usual care accurately. In more than half the workshops, and in order of importance, the most frequently cited categories and related themes under “factors that made the decision difficult for the patient” were experiencing uncertainty; fear of adverse outcomes; symptoms; support or undue pressure (perceptions of others and lack of advice from the physician); and balancing conflicting information, understanding information, lacking information on alternatives and on hormone therapy, receiving too much information, and judging the source of information to be unreliable.
In 4 workshops, some participants thought the patient had no difficulty making her decision about hormone therapy. In 3 workshops, some participants thought that when a patient says she is unsure, it is a polite way of saying no to the option being offered by the physician.
When asked about strategies used by the physician in the first video to provide support (usual care), the most frequently cited strategy was discussion of information. Related themes are listed in Table 2. No new data emerged after the eighth workshop. When asked about other strategies that could have been used to provide decision support, participants in more than half the workshops identified, in order of importance, exploration of fears, discussion of information and roles in decision making, and exploration of support or undue pressure. One item, “ask questions in another way,” was added in the 11th workshop.
Table 2.
Actions taken by physicians to provide decision support to simulated patients in the first and second videos
*Translated from French.
Views on the ODSF process and tools
After being introduced to the ODSF, participants watched the second video in which the physician used the ODSF process and tools. When asked about the new strategies used by the physician to provide decision support (Table 2), participants in 12 out of 13 workshops identified discussion of values. In more than half the workshops, participants also identified discussion of role, support or undue pressure, and decision-making status. No new strategies were identified after the 10th workshop. After seeing the second video, the most frequently identified other strategy participants mentioned was discussion of alternatives to hormone therapy. No other strategies were suggested after the 12th workshop.
Intended changes in practice
On the evaluation forms completed at the end of each workshop, the 5 most frequent changes in practice participants intended to make were to assess patients’ values, to ask for patients’ preferred role in decision making, to screen for and identify decisional conflict, to assess support or undue pressure from others, and to improve patients’ involvement in decision making.
DISCUSSION
Results of this study contribute to knowledge in the area of translating shared decision making into primary care practice for several reasons. First, participants provided a comprehensive list of difficult decisions they perceived their patients faced. These results are consistent with those of a large population-based survey of Canadians regarding their needs in health-related decision making.9 This is interesting because it suggests that family physicians who participated in this study agreed with the health decision-making needs expressed by a sample of Canadians who were not health professionals. Therefore, this list could inform developers of decision aids about key areas to explore to improve their clinical relevance for primary care.
Second, these results provide insight into how three quarters of the clinical teachers and residents in one department of family medicine in Canada view a decision support intervention aimed at facilitating patients’ involvement in decision making, that is, shared decision making. In both videos used in this study, the simulated patient provided numerous cues to help participants identify decisional conflict.20 In the first video depicting usual care, at the end of the clinical encounter, the woman said she was still unsure (hallmark of decisional conflict). Nevertheless, in 4 separate workshops, some participants thought she had no difficulty. In 3 workshops, hesitation was interpreted as a polite way for the patient to say no to hormone therapy. This suggests some physicians still need to learn how to identify decisional conflict, a key skill in informed and shared decision making.1
Third, following the first video, when asked about the factors that made the decision difficult for the simulated patient, participants in fewer than one third of the workshops mentioned the possible need to balance or clarify values. After the first video, when asked about the strategies the physician had used to provide decision support, participants identified mostly information-related strategies. This is interesting, given the fact that there was general consensus that the first video showed usual care. This is congruent with results of previous studies that showed that physicians tend not to ask patients about their values.12,26 This suggests that family physicians need tools to help them attend to patients’ values, a key component of informed and shared decision making.1
Fourth, following the first video, the other strategy participants most frequently said they would have used to provide decision support was exploration of fears or worries. This is congruent with the content of the OPTION scale that assesses physicians’ behaviour in involving patients in decision making.15 The OPTION scale was developed by a group of general practitioners in Wales, UK, and, therefore, is not based on the ODSF. This agreement between the ODSF and the OPTION scale suggests that exploration of fears or worries is a key component of what family physicians perceive shared decision making to be. These findings also suggest that family physicians still view their role as one of providing reassurance and one cherished by patients27 and physicians.28 Yet, it is still unclear how providing reassurance to patients is compatible with promoting their involvement in decision making.
Last, following the second video in which the physician used the ODSF structured process and related tools, participants clearly identified some key components. Most frequently they mentioned discussion of the patient’s values, followed by discussion of role, support or undue pressure, and decision-making status. This list of strategies is quite similar to the list of changes that participants intended to make in their practices and could be a predictor of change in physicians’ practice behaviour.29 This suggests that the ODSF could help health care providers pay more attention to patients’ values.30
Limitations
In spite of its interesting findings, this study has limitations. First, we used qualitative methods to explore family physicians’ views on supporting patients facing difficult health care decisions and on use of the ODSF. Qualitative approaches cannot provide background for inferential interpretations of data.
The principal investigator’s previous personal and professional experiences might have influenced interpretation of results.31 To reduce this influence, data were collected by a trained anthropologist who acted as a non-participating observer. Triangulation of data was employed (verbatim reports and participants’ written comments), and data were analyzed for content with the help of 1 independent research assistant who had not participated in the trial before this stage. Member checking of the interim report was carried out, and representative excerpts from the data sources were provided.
Second, this study was conducted in academic clinical settings where the patient-centred method is valued and taught. Therefore, we cannot assume that these results are transferable to other types of clinical settings.
Third, we adapted our group discussion to fit a 1.5-hour interactive workshop. It is possible that participants did not have enough time to discuss the topic and that important comments were not collected. We did our best in light of the fact that “few resources are available for clinical effectiveness activities and there is a need for maximizing benefits from any one of those.”32 Data matrices showed that, for most questions, we were able to reach saturation within the number of workshops that were conducted.
Finally, 43 of the 53 residents who enrolled in the overall trial participated in the workshop. Only 15 of these, however, were able to complete the entire implementation trial. More needs to be done to ensure participation of residents in implementation trials. Perhaps it will be necessary to ensure that they can recruit patients at other clinical sites.
Conclusion
Despite its limitations, the contribution of this study is both methodologic and substantive. The method developed to identify physicians’ views on decision support and on use of the ODSF could be of interest to health services researchers. The interactive workshop served as a component of a multifaceted implementation strategy. It also served as a strategy for comprehensive data collection from a large group of health professionals in a relatively short period. Given the importance of family physicians’ exploring patients’ fears or worries, future research should assess how providing reassurance to patients relates to promoting patients’ involvement in decision making. This new knowledge will facilitate implementation of shared decision-making processes in the context of family medicine in Canada, a topic that has been woefully under-studied.
Acknowledgments
We are indebted to the 122 primary care providers who enrolled in the implementation trial. We thank Mr Anthony Chadwick for reviewing our manuscript. Dr Légaré was supported by a scholarship from the Canadian Institutes of Health Research (CIHR) Institute of Health Services and Policy and Research and is currently supported by a clinical scientist award from the Fonds de la Recherche en Santé du Québec. This research was supported by the Canada Research Chair in Health Related Decision Support, ICEBERG, Chaire Andrée et Lucie Chagnon pour une approche intégrée en santé, and Centre de recherche du CHUQ hôpital St-François d’Assise.
Biography
Drs Légaré, Saucier, and Cauchon are family physicians with the Department of Family Medicine at Laval University in Quebec city, Que. Dr Légaré holds a New Clinical Scientist award from Fonds de la recherche en santé du Québec. Dr O’Connor is a Tier 1 Canada Research Chair in Health Related Decision Support. Dr Graham holds a New Scientist award from the Canadian Institutes of Health Research. Dr Côté is Acting Director of the Centre de développement pédagogique des sciences de la santé in the Faculty of Medicine at Laval University. Ms Paré is a social worker with the Centre Local de Santé Communautaire Haute-Ville.
Footnotes
Competing interests: None declared
References
- 1.Towle A, Godolphin W. Framework for teaching and learning informed shared decision making. BMJ. 1999;319(7212):766–771. doi: 10.1136/bmj.319.7212.766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Stewart M, Brown JB, Weston WW, McWhinney IR, McWilliam CL, Freeman TR. Patient-centered medicine: transforming the clinical method. London, Engl: Sage Publications; 1995. [Google Scholar]
- 3.Weston WW. Informed and shared decision-making: the crux of patient-centred care. CMAJ. 2001;165:438–440. [PMC free article] [PubMed] [Google Scholar]
- 4.Wetzels R, Wensing M, Grol R. Involving older patients in general/family practice. Concept, tools and implementation. Copenhagen, Denmark: European Association for Quality in General Practice/Family Medicine; 2004. [Google Scholar]
- 5.Howie J, Heaney D, Maxwell M. Quality, core values and the general practice consultation: issues of definition, measurement and delivery. Fam Pract. 2004;21(4):458–468. doi: 10.1093/fampra/cmh419. [DOI] [PubMed] [Google Scholar]
- 6.O’Connor AM, Stacey D, Entwistle V, Llewellyn-Thomas H, Rovner D, Holmes-Rovner M, et al. Decision aids for people facing health treatment or screening decisions (Cochrane review). Update software ed. In: The Cochrane Library. Oxford, Engl: Cochrane Library; 2004. [Google Scholar]
- 7.Federal, Provincial and Territorial Advisory Committee on Population Health. Statistical report on the health of Canadians. Ottawa, Ont: Statistics Canada, Health Canada; 1999. [Google Scholar]
- 8.Martin S. “Shared responsibility” becoming the new medical buzz phrase. CMAJ. 2002;167:295. [PMC free article] [PubMed] [Google Scholar]
- 9.O’Connor AM, Drake E, Wells G, Tugwell P, Laupacis A, Elmslie T. A survey of the decision-making needs of Canadians faced with complex health decisions. Health Expect. pp. 1–13. [DOI] [PMC free article] [PubMed]
- 10.Elwyn G, Edwards A, Gwyn R, Grol R. Towards a feasible model for shared decision making: focus group study with general practice registrars. BMJ. 1999;319(7212):753–756. doi: 10.1136/bmj.319.7212.753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Godolphin W, Towle A, McKendry R. Challenges in family practice related to informed and shared decision-making: a survey of preceptors of medical students. CMAJ. 2001;165:434–435. [PMC free article] [PubMed] [Google Scholar]
- 12.Makoul G, Arntson P, Schofield T. Health promotion in primary care: physician-patient communication and decision making about prescription medications. Soc Sci Med. pp. 1241–1254. [DOI] [PubMed]
- 13.Guimond P, Bunn H, O’Connor AM, Jacobsen MJ, Tait VK, Drake ER, et al. Validation of a tool to assess health practitioners’ decision support and communication skills. Patient Educ Couns. pp. 235–245. [DOI] [PubMed]
- 14.McKinstry B. Do patients wish to be involved in decision making in the consultation? A cross sectional survey with video vignettes. BMJ. 2000;321(7265):867–871. doi: 10.1136/bmj.321.7265.867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Elwyn G, Edwards A, Wensing M, Hood K, Atwell C, Grol R. Shared decision making: developing the OPTION scale for measuring patient involvement. Qual Saf Health Care. pp. 93–99. [DOI] [PMC free article] [PubMed]
- 16.O’Connor AM, Tugwell P, Wells GA, Elmslie T, Jolly E, Hollingworth G, et al. A decision aid for women considering hormone therapy after menopause: decision support framework and evaluation. Patient Educ Couns. pp. 267–279. [DOI] [PubMed]
- 17.O’Connor AM, Drake ER, Fiset V, Graham ID, Laupacis A, Tugwell P. The Ottawa patient decision aids. Eff Clin Pract. pp. 163–170. [PubMed]
- 18.Carpenito-Moyet LJ. Decisional conflict. In: Nursing diagnosis: application to clinical practice. Philadelphia, Pa: Lippincott Williams and Wilkins; 2000. pp. 312–321. [Google Scholar]
- 19.Towle A, Godolphin W. Education and training of health care professionals. In: Edwards A, Elwyn G, editors. Evidence-based patient choice: inevitable or impossible? Oxford, Engl: Oxford University Press; 2001. pp. 245–270. [Google Scholar]
- 20.O’Connor AM. Validation of a decisional conflict scale. Med Decis Making. pp. 25–30. [DOI] [PubMed]
- 21.Pope C, Mays N. Reaching the parts other methods cannot reach: an introduction to qualitative methods in health and health services research. BMJ. 1995;311(6996):42–45. doi: 10.1136/bmj.311.6996.42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Mays N, Pope C. Rigour and qualitative research. BMJ. 1995;311(6997):109–112. doi: 10.1136/bmj.311.6997.109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Mays N, Pope C. Qualitative research: observational methods in health care settings. BMJ. 1995;311(6998):182–184. doi: 10.1136/bmj.311.6998.182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Cresswell JW. Qualitative inquiry and research design. Choosing among five traditions. Thousand Oaks, Calif: Sage Publications; 1998. [Google Scholar]
- 25.Miles MB, Huberman AM. An expanded sourcebook. Qualitative data analysis. 2nd ed. Thousand Oaks, Calif: Sage Publications; 1994. [Google Scholar]
- 26.Massé R, Légaré F, Côté L, Dodin S. The limitations of a negotiation model for perimenopausal women. Sociol Health Illness. 2001;23(1):44–64. [Google Scholar]
- 27.Edwards A, Elwyn G, Smith C, Williams S, Thornton H. Consumers’ views of quality in the consultation and their relevance to ‘shared decision-making’ approaches. Health Expect. pp. 151–161. [DOI] [PMC free article] [PubMed]
- 28.West AF, West RR. Clinical decision-making: coping with uncertainty. Postgrad Med J. pp. 319–321. [DOI] [PMC free article] [PubMed]
- 29.Wakefield J, Herbert CP, Maclure M, Dormuth C, Wright JM, Legare J, et al. Commitment to change statements can predict actual change in practice. J Contin Educ Health Prof. pp. 81–93. [DOI] [PubMed]
- 30.Llewellyn-Thomas H, Sutherland HJ, Tibshirani R, Ciampi A, Till JE, Boyd NF. The measurement of patients’ values in medicine. In: Elstein JA, Da AS, editors. Professional judgment. Cambridge, Engl: Cambridge University Press; 1988. pp. 395–408. [Google Scholar]
- 31.Malterud K. Qualitative research: standards, challenges, and guidelines. Lancet. 2001;358(9280):483–488. doi: 10.1016/S0140-6736(01)05627-6. [DOI] [PubMed] [Google Scholar]
- 32.Grimshaw JM, Thomas RE, MacLennan G, Fraser C, Ramsay CR, Vale L, et al. Effectiveness and efficiency of guideline dissemination and implementation strategies. Health Technol Assess. iii-iv,1-72. [DOI] [PubMed]