Abstract
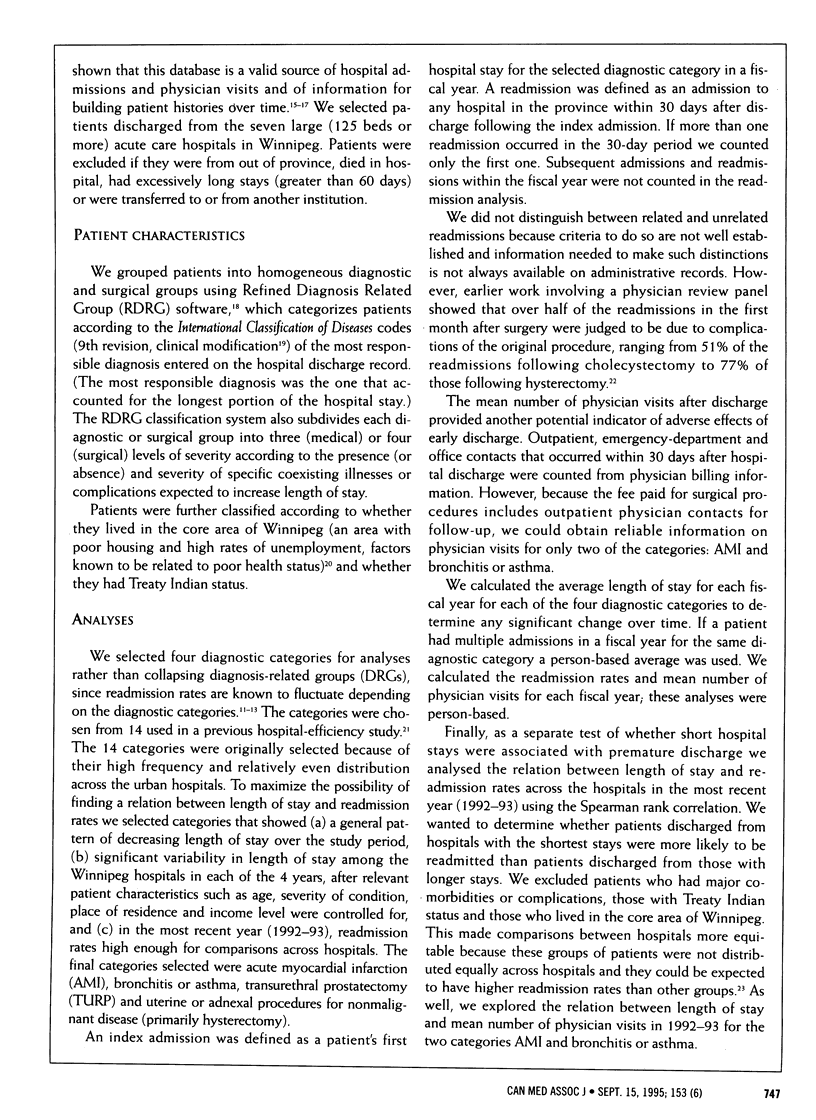
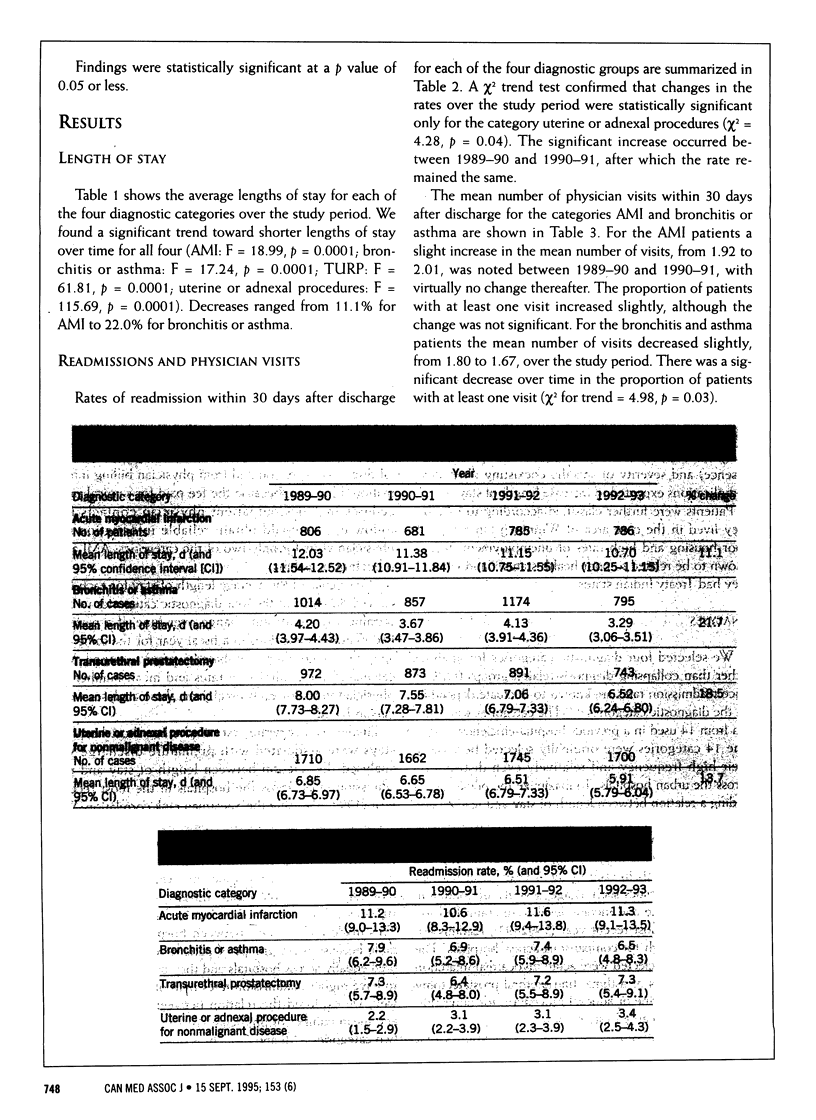
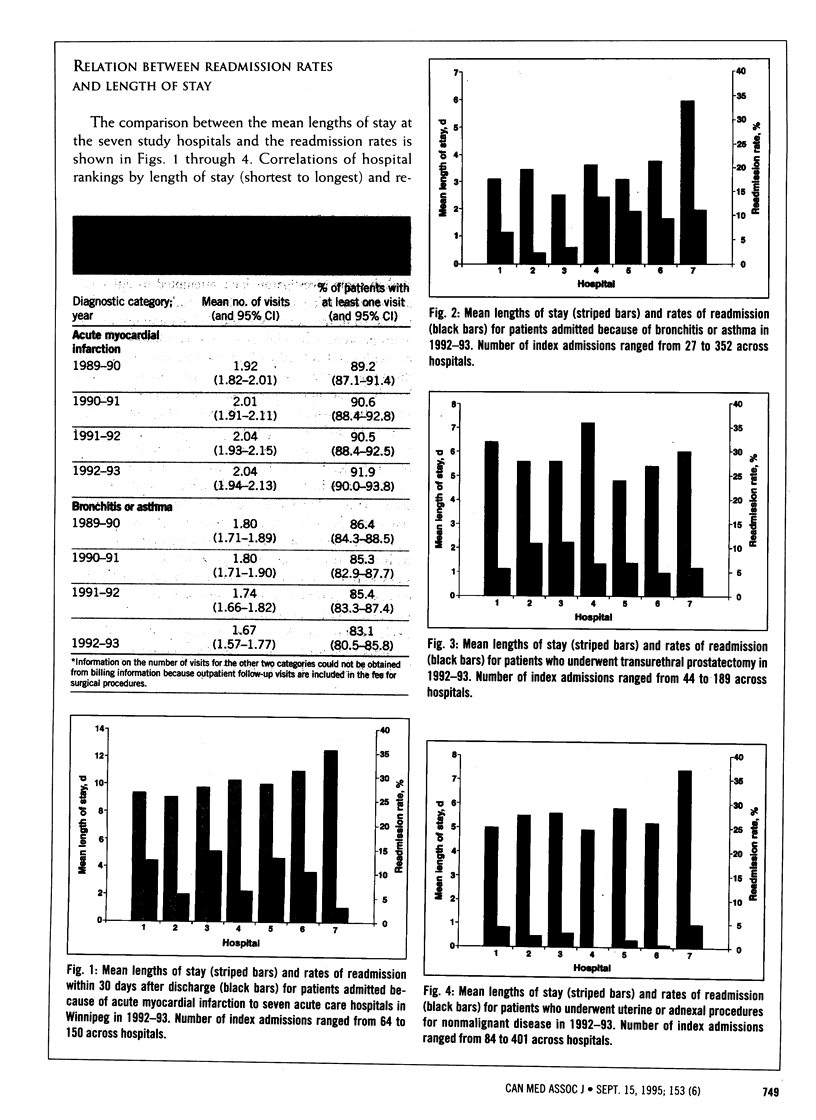
OBJECTIVE: To determine whether decreasing lengths of stay over time for selected diagnostic categories were associated with increased hospital readmission rates and mean number of physician visits after discharge. DESIGN: Retrospective descriptive study. SETTING: The seven large (125 beds or more) acute care hospitals in Winnipeg. PATIENTS: Manitoba residents admitted to any one of the seven hospitals because acute myocardial infarction (AMI), bronchitis or asthma, transurethral prostatectomy (TURP) and uterine or adnexal procedures for nonmalignant disease during the fiscal years 1989-90 to 1992-93. Patients from out of province, those who died in hospital, those with excessively long stays (more than 60 days) and those who were transferred to or from another institution were excluded. OUTCOME MEASURES: Length of hospital stay, and rate of readmission within 30 days after discharge for all four categories and mean number of physician visits within 30 days after discharge for two categories (AMI and bronchitis or asthma. RESULTS: The length of stay decreased significantly over the 4 years for all of the four categories, the smallest change being observed for patients with AMI (11.1%) and the largest for those with bronchitis or asthma (22.0%). The readmission rates for AMI, bronchitis or asthma, and TURP showed no consistent change over the 4 years. The readmission rate for uterine or adnexal procedures increased significantly between the first and second year (chi 2 = 4.28, p = 0.04) but then remained constant over the next 3 years. The mean number of physician visits increased slightly for AMI in the first year (1.92 to 2.01) and then remained virtually the same. It decreased slightly for bronchitis or asthma over the 4 years. There was no significant correlation between length of stay and readmission rates for individual hospitals in 1992-93 in any of the four categories. Also, no correlation was observed between length of stay and mean number of physician visits for individual hospitals in 1992-93 in the categories AMI and bronchitis or asthma. CONCLUSIONS: Improving hospital efficiency by shortening length of stay does not appear to result in increased rates of readmission or numbers of physician visits within 30 days after discharge from hospital. Research is needed to identify optimal lengths of stay and expected readmission rates.
Full text
PDF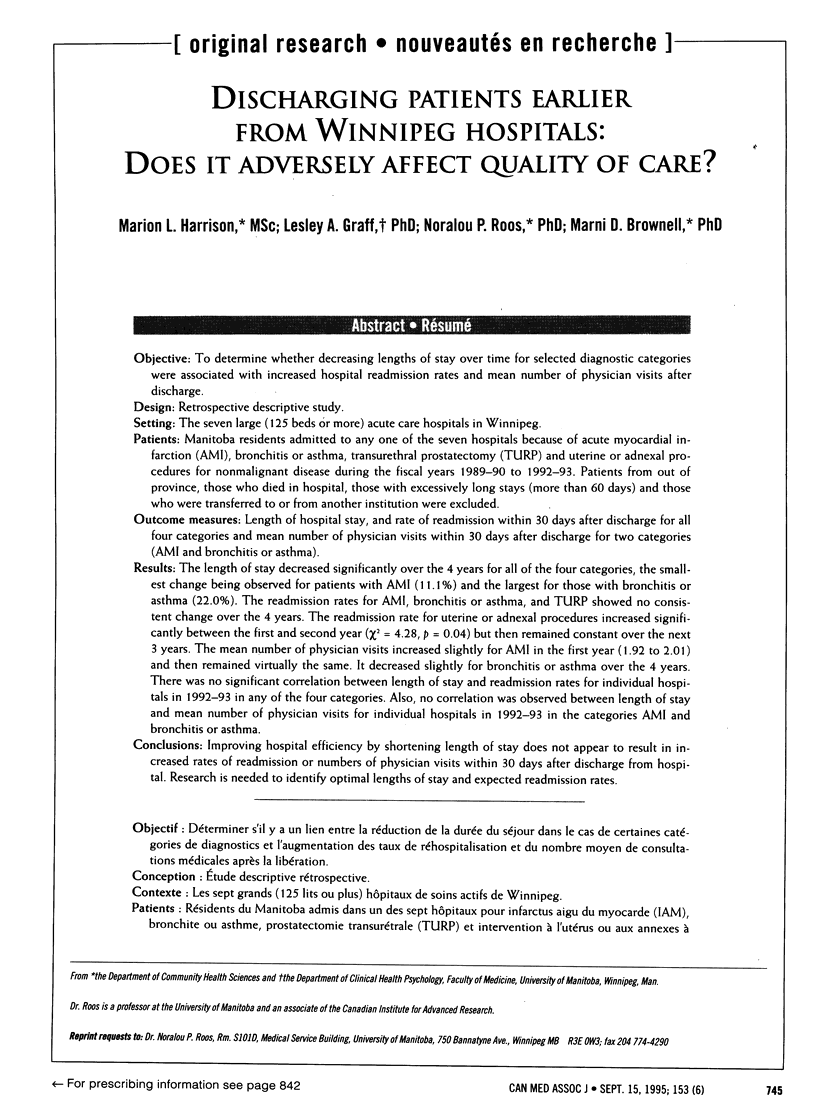

Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Brook R. H., Lohr K. N. Monitoring quality of care in the Medicare program. Two proposed systems. JAMA. 1987 Dec 4;258(21):3138–3141. [PubMed] [Google Scholar]
- Brownell M. D., Roos N. P. Variation in length of stay as a measure of efficiency in Manitoba hospitals. CMAJ. 1995 Mar 1;152(5):675–682. [PMC free article] [PubMed] [Google Scholar]
- Cleary P. D., Greenfield S., Mulley A. G., Pauker S. G., Schroeder S. A., Wexler L., McNeil B. J. Variations in length of stay and outcomes for six medical and surgical conditions in Massachusetts and California. JAMA. 1991 Jul 3;266(1):73–79. [PubMed] [Google Scholar]
- DesHarnais S. I., McMahon L. F., Jr, Wroblewski R. T., Hogan A. J. Measuring hospital performance. The development and validation of risk-adjusted indexes of mortality, readmissions, and complications. Med Care. 1990 Dec;28(12):1127–1141. [PubMed] [Google Scholar]
- DesHarnais S., Hogan A. J., McMahon L. F., Jr, Fleming S. Changes in rates of unscheduled hospital readmissions and changes in efficiency following the introduction of the Medicare prospective payment system. An analysis using risk-adjusted data. Eval Health Prof. 1991 Jun;14(2):228–252. doi: 10.1177/016327879101400206. [DOI] [PubMed] [Google Scholar]
- Epstein A. M., Bogen J., Dreyer P., Thorpe K. E. Trends in length of stay and rates of readmission in Massachusetts: implications for monitoring quality of care. Inquiry. 1991 Spring;28(1):19–28. [PubMed] [Google Scholar]
- Gooding J., Jette A. M. Hospital readmissions among the elderly. J Am Geriatr Soc. 1985 Sep;33(9):595–601. doi: 10.1111/j.1532-5415.1985.tb06315.x. [DOI] [PubMed] [Google Scholar]
- Holloway J. J., Medendorp S. V., Bromberg J. Risk factors for early readmission among veterans. Health Serv Res. 1990 Apr;25(1 Pt 2):213–237. [PMC free article] [PubMed] [Google Scholar]
- Kosecoff J., Kahn K. L., Rogers W. H., Reinisch E. J., Sherwood M. J., Rubenstein L. V., Draper D., Roth C. P., Chew C., Brook R. H. Prospective payment system and impairment at discharge. The 'quicker-and-sicker' story revisited. JAMA. 1990 Oct 17;264(15):1980–1983. [PubMed] [Google Scholar]
- Manheim L. M., Feinglass J., Shortell S. M., Hughes E. F. Regional variation in Medicare hospital mortality. Inquiry. 1992 Spring;29(1):55–66. [PubMed] [Google Scholar]
- Manton K. G., Woodbury M. A., Vertrees J. C., Stallard E. Use of Medicare services before and after introduction of the prospective payment system. Health Serv Res. 1993 Aug;28(3):269–292. [PMC free article] [PubMed] [Google Scholar]
- Riley G., Lubitz J. Outcomes of surgery in the Medicare aged population: rehospitalization after surgery. Health Care Financ Rev. 1986 Fall;8(1):23–34. [PMC free article] [PubMed] [Google Scholar]
- Roos L. L., Jr, Cageorge S. M., Austen E., Lohr K. N. Using computers to identify complications after surgery. Am J Public Health. 1985 Nov;75(11):1288–1295. doi: 10.2105/ajph.75.11.1288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roos L. L., Jr, Roos N. P., Cageorge S. M., Nicol J. P. How good are the data? Reliability of one health care data bank. Med Care. 1982 Mar;20(3):266–276. doi: 10.1097/00005650-198203000-00003. [DOI] [PubMed] [Google Scholar]
- Roos L. L., Mustard C. A., Nicol J. P., McLerran D. F., Malenka D. J., Young T. K., Cohen M. M. Registries and administrative data: organization and accuracy. Med Care. 1993 Mar;31(3):201–212. doi: 10.1097/00005650-199303000-00002. [DOI] [PubMed] [Google Scholar]
- Roos L. L., Sharp S. M., Wajda A. Assessing data quality: a computerized approach. Soc Sci Med. 1989;28(2):175–182. doi: 10.1016/0277-9536(89)90145-7. [DOI] [PubMed] [Google Scholar]
- Thomas J. W., Holloway J. J. Investigating early readmission as an indicator for quality of care studies. Med Care. 1991 Apr;29(4):377–394. doi: 10.1097/00005650-199104000-00006. [DOI] [PubMed] [Google Scholar]
- Weissman J. S., Stern R. S., Epstein A. M. The impact of patient socioeconomic status and other social factors on readmission: a prospective study in four Massachusetts hospitals. Inquiry. 1994 Summer;31(2):163–172. [PubMed] [Google Scholar]


