Abstract
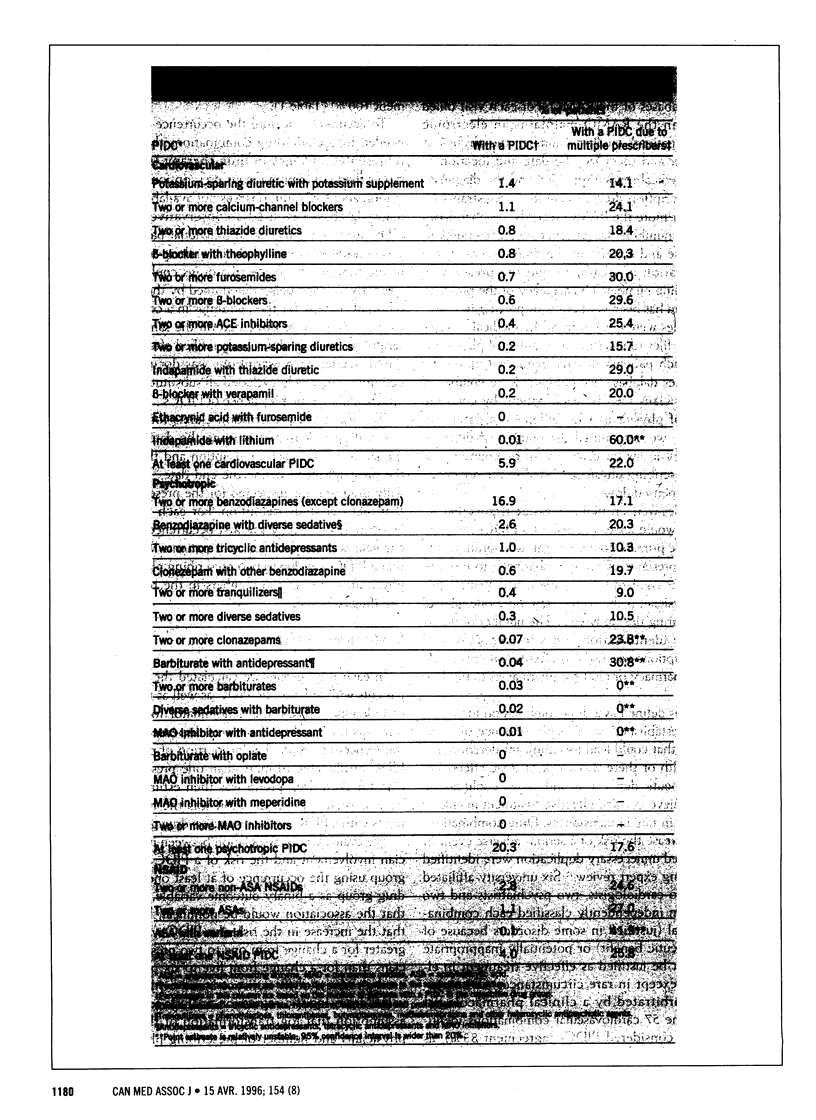
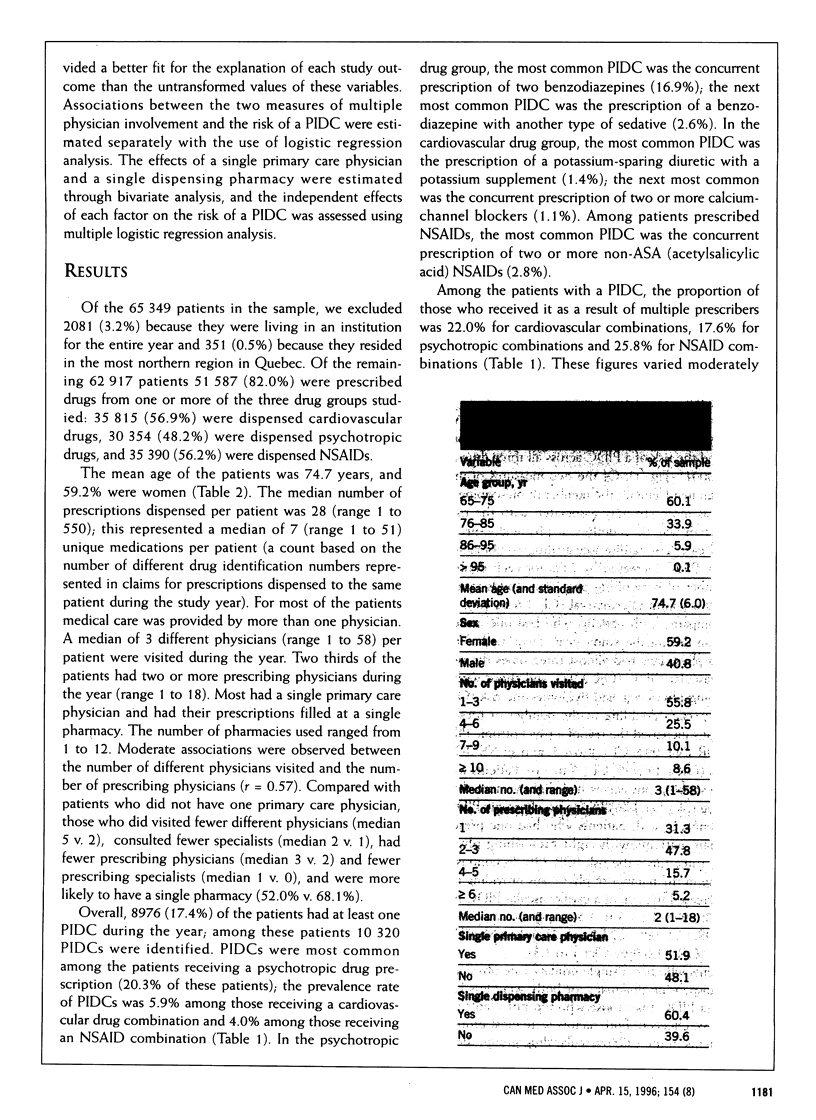
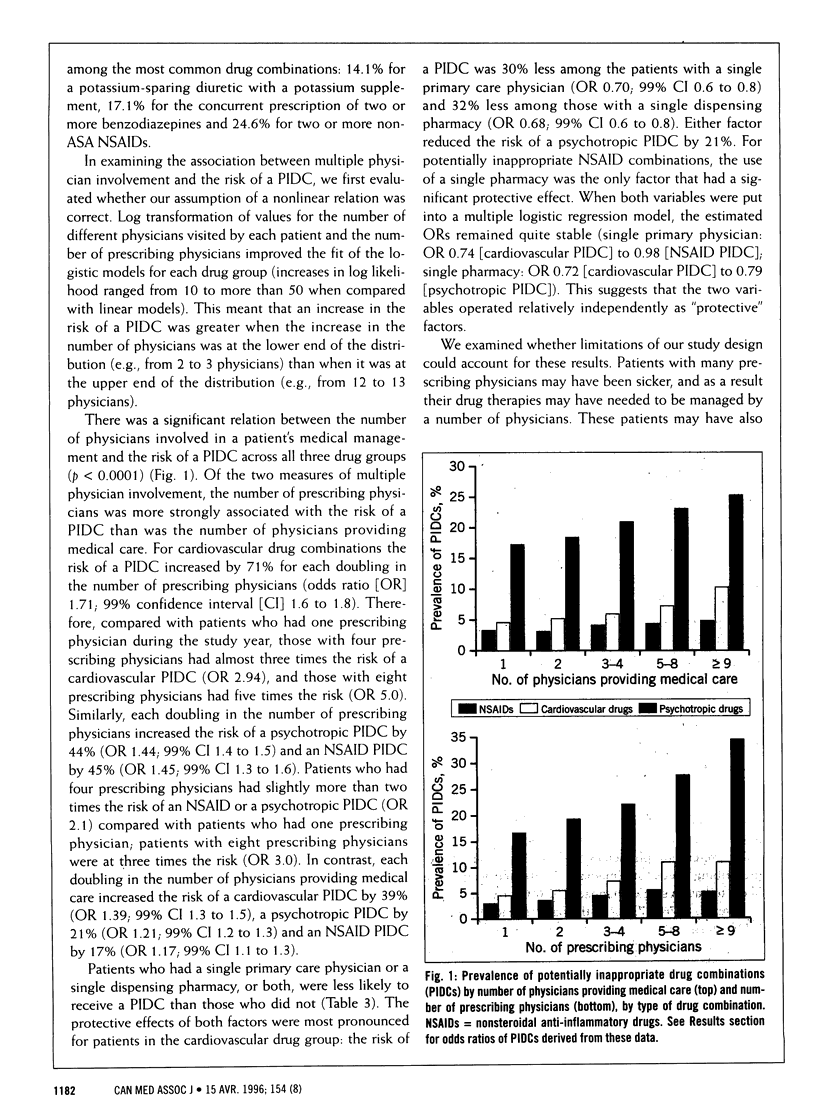
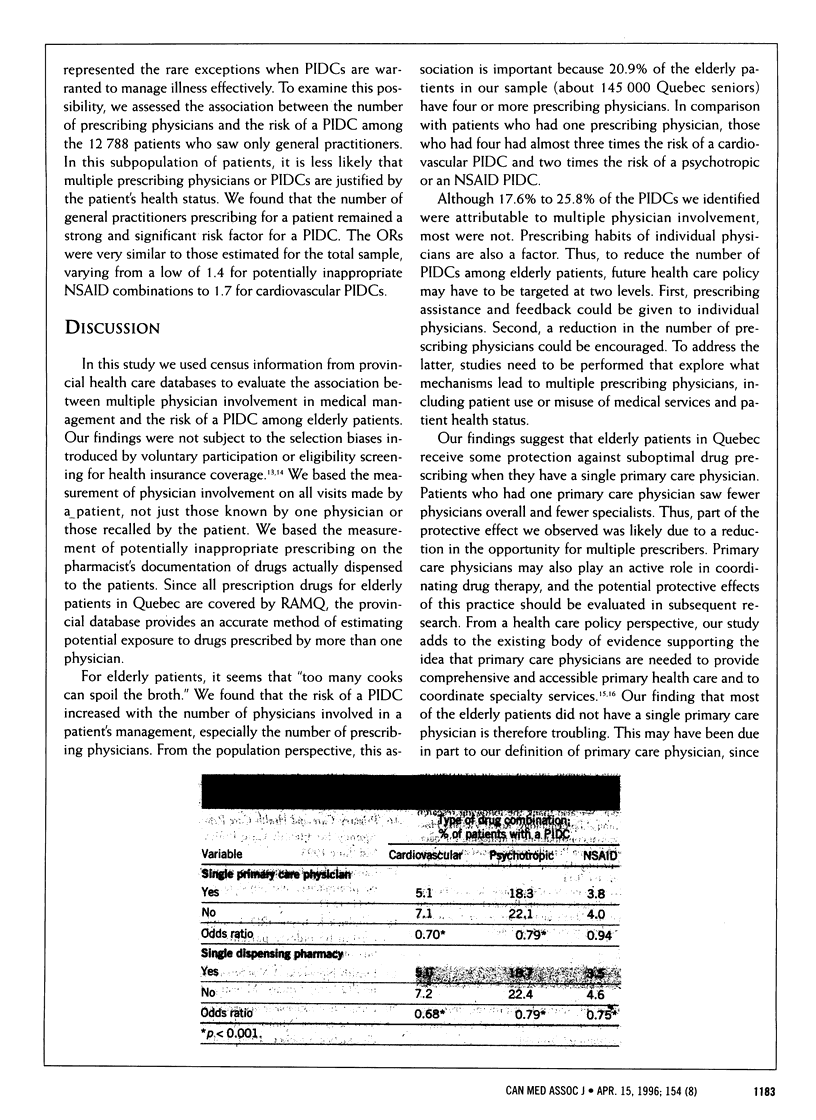
OBJECTIVES: To determine (a) whether the risk of a potentially inappropriate drug combination (PIDC) increases with the number of physicians involved in the medical management of an elderly patient and (b) whether the risk of a PIDC is reduced if a patient has a single primary care physician or a single dispensing pharmacy, or both. DESIGN: Cross-sectional retrospective provincial database study. PARTICIPANTS: A regionally stratified random sample of 51,587 elderly medicare registrants in Quebec who (a) visited at least one physician in 1990, (b) were not living in a health care institution for the entire year and (c) had been dispensed at least one prescription for a cardiovascular drug, a psychotropic drug or a nonsteroidal anti-inflammatory drug (NSAID). OUTCOME MEASURES: Information on all physician visits and drugs dispensed during 1990. Physician claims were used to identify the number of physicians involved in a patient's management and whether the patient had one primary care physician. Prescription claims were used to identify the number of PIDCs, prescribing physicians and dispensing pharmacies. RESULTS: The prevalence of PIDCs ranged from 4.0% (among those in the NSAID group) to 20.3% (among those in the psychotropic drug group). Of the PIDCs identified, 17.6% to 25.8% resulted from contemporaneous prescribing by different physicians. The number of prescribing physicians was the most important risk factor for a PIDC in all drug groups (odds ratio [OR] 1.44 to 1.71). The presence of a single primary care physician lowered the risk for cardiovascular and psychotropic PIDCs (OR 0.70 and 0.79 respectively) but not for NSAID PIDCs (OR 0.94). The use of a single dispensing pharmacy lowered the risk of a PIDC in all drug groups (OR 0.68 to 0.79). CONCLUSION: The greater the number of physicians prescribing medications for an elderly patient, the greater is the risk that the patient will receive a PIDC. A single primary care physician and a single dispensing pharmacy may be "protective" factors in preventing PIDCs.
Full text
PDF



Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Beers M. H., Ouslander J. G. Risk factors in geriatric drug prescribing. A practical guide to avoiding problems. Drugs. 1989 Jan;37(1):105–112. doi: 10.2165/00003495-198937010-00008. [DOI] [PubMed] [Google Scholar]
- Col N., Fanale J. E., Kronholm P. The role of medication noncompliance and adverse drug reactions in hospitalizations of the elderly. Arch Intern Med. 1990 Apr;150(4):841–845. [PubMed] [Google Scholar]
- Colt H. G., Shapiro A. P. Drug-induced illness as a cause for admission to a community hospital. J Am Geriatr Soc. 1989 Apr;37(4):323–326. doi: 10.1111/j.1532-5415.1989.tb05498.x. [DOI] [PubMed] [Google Scholar]
- Grymonpre R. E., Mitenko P. A., Sitar D. S., Aoki F. Y., Montgomery P. R. Drug-associated hospital admissions in older medical patients. J Am Geriatr Soc. 1988 Dec;36(12):1092–1098. doi: 10.1111/j.1532-5415.1988.tb04395.x. [DOI] [PubMed] [Google Scholar]
- Gurwich E. L. Comparison of medication histories acquired by pharmacists and physicians. Am J Hosp Pharm. 1983 Sep;40(9):1541–1542. [PubMed] [Google Scholar]
- Ives T. J., Bentz E. J., Gwyther R. E. Drug-related admissions to a family medicine inpatient service. Arch Intern Med. 1987 Jun;147(6):1117–1120. [PubMed] [Google Scholar]
- Kendrick R., Bayne J. R. Compliance with prescribed medication by elderly patients. Can Med Assoc J. 1982 Nov 15;127(10):961–962. [PMC free article] [PubMed] [Google Scholar]
- Larson E. B., Kukull W. A., Buchner D., Reifler B. V. Adverse drug reactions associated with global cognitive impairment in elderly persons. Ann Intern Med. 1987 Aug;107(2):169–173. doi: 10.7326/0003-4819-107-2-169. [DOI] [PubMed] [Google Scholar]
- Ray W. A., Griffin M. R., Schaffner W., Baugh D. K., Melton L. J., 3rd Psychotropic drug use and the risk of hip fracture. N Engl J Med. 1987 Feb 12;316(7):363–369. doi: 10.1056/NEJM198702123160702. [DOI] [PubMed] [Google Scholar]
- Siddharthan K. HMO enrollment by Medicare beneficiaries in heterogeneous communities. Med Care. 1990 Oct;28(10):918–927. doi: 10.1097/00005650-199010000-00006. [DOI] [PubMed] [Google Scholar]
- Soumerai S. B., McLaughlin T. J., Avorn J. Improving drug prescribing in primary care: a critical analysis of the experimental literature. Milbank Q. 1989;67(2):268–317. [PubMed] [Google Scholar]
- Tamblyn R., Lavoie G., Petrella L., Monette J. The use of prescription claims databases in pharmacoepidemiological research: the accuracy and comprehensiveness of the prescription claims database in Québec. J Clin Epidemiol. 1995 Aug;48(8):999–1009. doi: 10.1016/0895-4356(94)00234-h. [DOI] [PubMed] [Google Scholar]
- Tinetti M. E., Speechley M., Ginter S. F. Risk factors for falls among elderly persons living in the community. N Engl J Med. 1988 Dec 29;319(26):1701–1707. doi: 10.1056/NEJM198812293192604. [DOI] [PubMed] [Google Scholar]


