Abstract
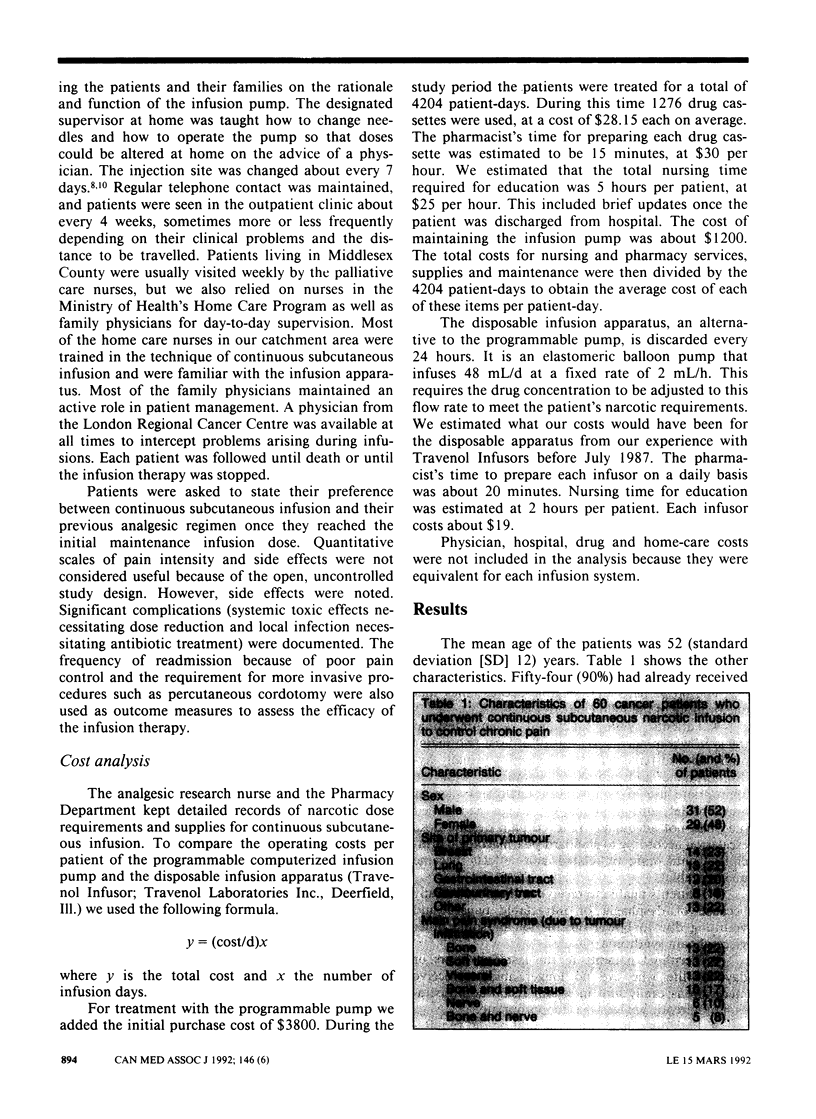
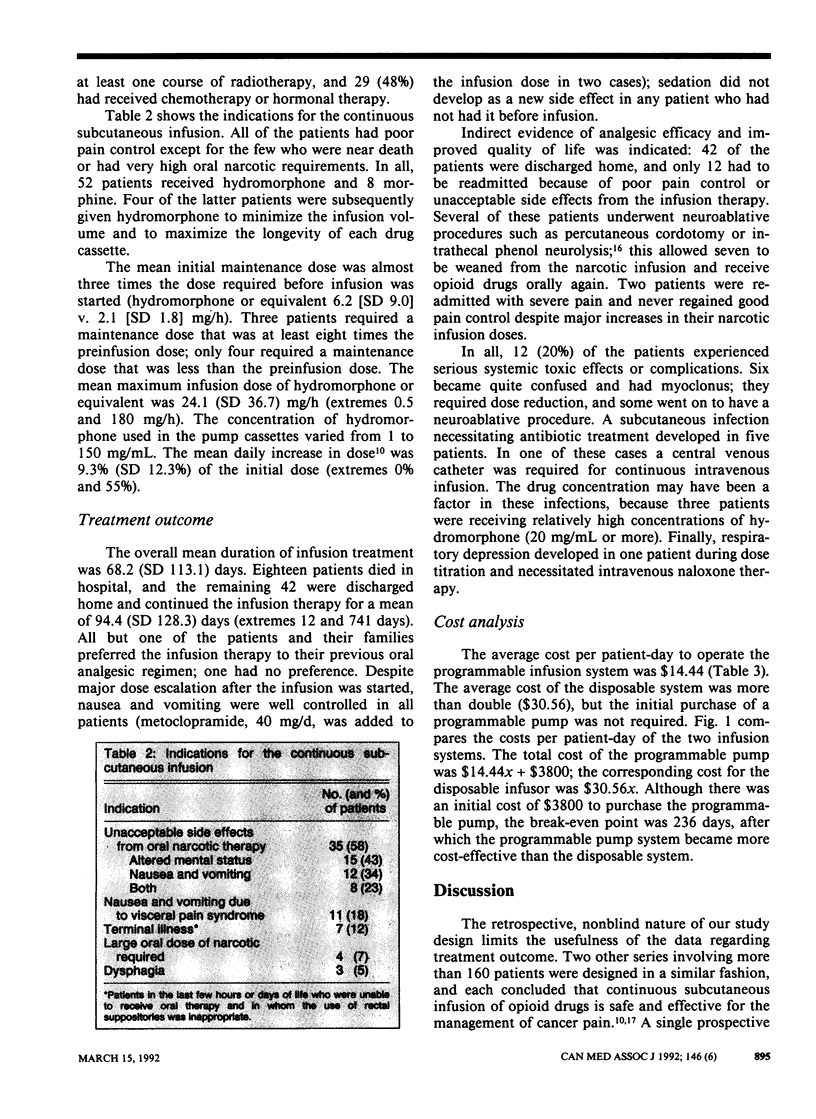
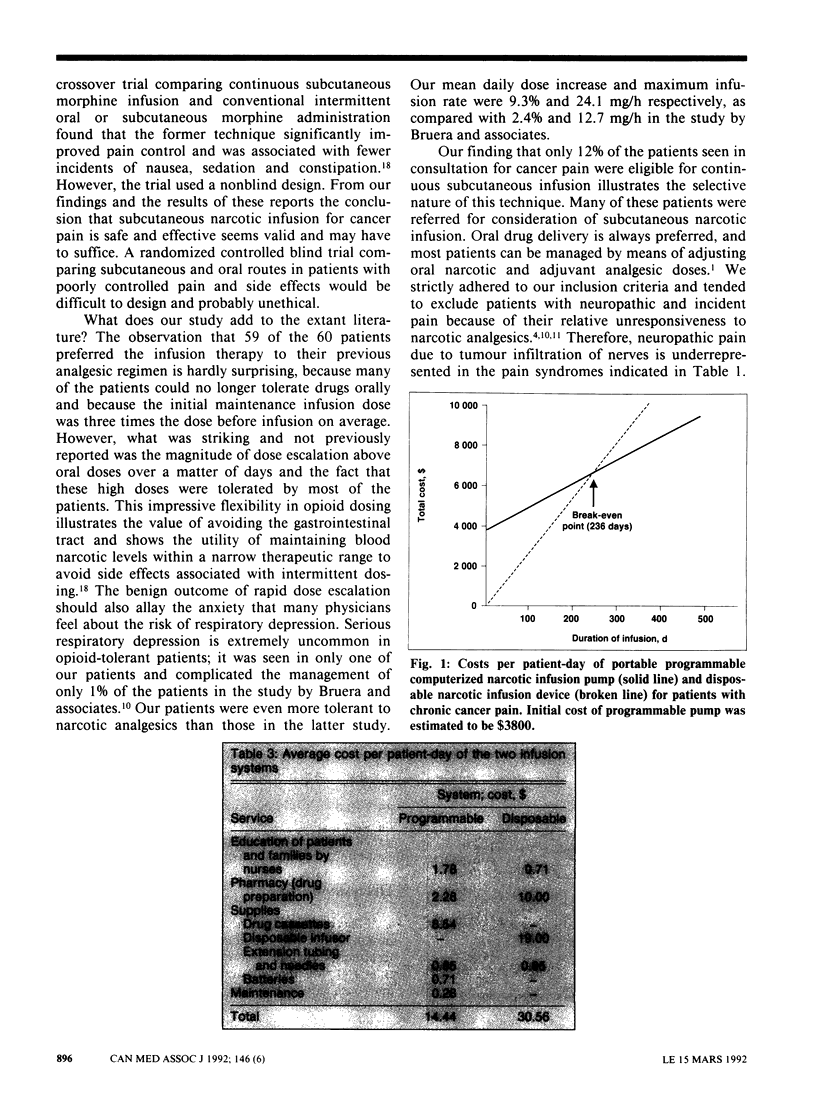
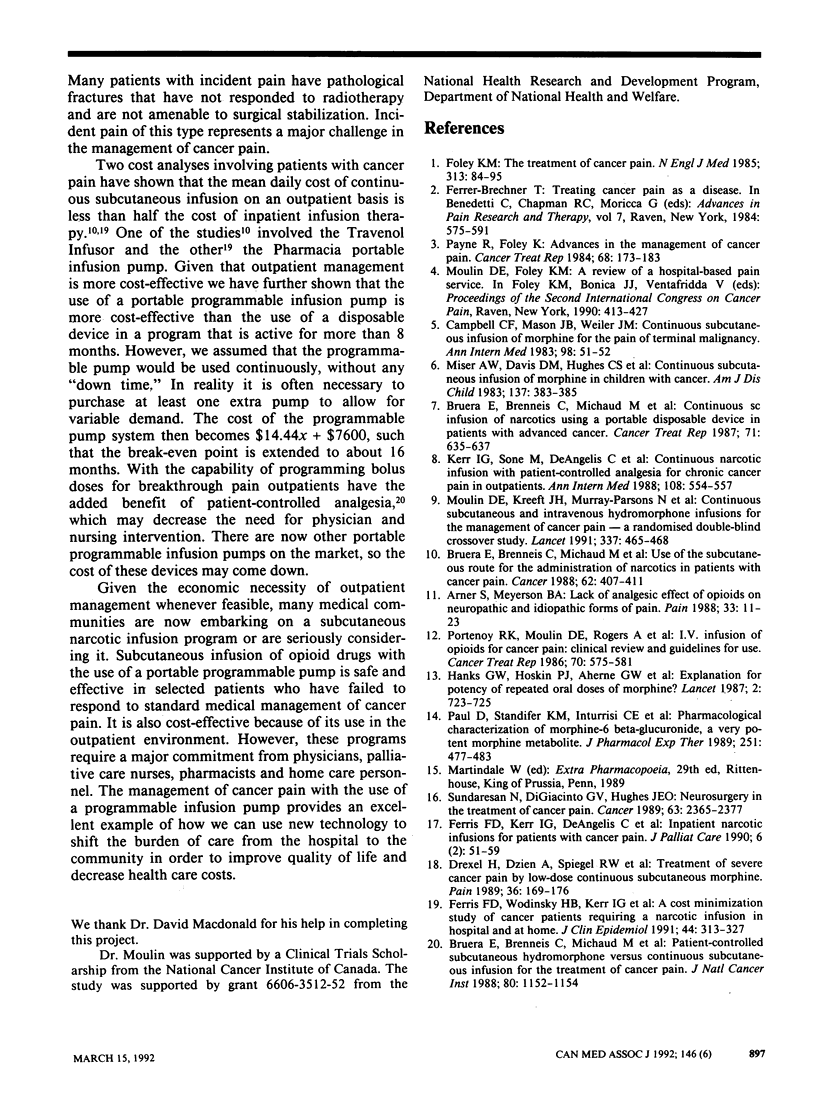
OBJECTIVE: To provide guidelines for the institution and maintenance of a continuous subcutaneous narcotic infusion program for cancer patients with chronic pain through an analysis of the narcotic requirements and treatment outcomes of patients who underwent such therapy and a comparison of the costs of two commonly used infusion systems. DESIGN: Retrospective study. SETTING: Tertiary care facilities and patients' homes. PATIENTS: Of 481 patients seen in consultation for cancer pain between July 1987 and April 1990, 60 (12%) met the eligibility criteria (i.e., standard medical management had failed, and they had adequate supervision at home). INTERVENTION: Continuous subcutaneous infusion with hydromorphone hydrochloride or morphine started on an inpatient basis and continued at home whenever possible. OUTCOME MEASURES: Patient selectivity, narcotic dosing requirements, discharge rate, patient preference for analgesic regimen, side effects, complications and cost-effectiveness. RESULTS: The mean initial maintenance infusion dose after dose titration was almost three times higher than the dose required before infusion (hydromorphone or equivalent 6.2 v. 2.1 mg/h). Eighteen patients died, and the remaining 42 were discharged home for a mean of 94.4 (standard deviation 128.3) days (extremes 12 and 741 days). The mean maximum infusion rate was 24.1 mg/h (extremes 0.5 and 180 mg/h). All but one of the patients preferred the infusion system to their previous oral analgesic regimen. Despite major dose escalations nausea and vomiting were well controlled in all cases. Twelve patients (20%) experienced serious systemic toxic effects or complications; six became encephalopathic, which necessitated dose reduction, five had a subcutaneous infection necessitating antibiotic treatment, and one had respiratory depression. The programmable computerized infusion pump was found to be more cost-effective than the disposable infusion device after a break-even point of 8 months. CONCLUSIONS: Continuous subcutaneous infusion of opioid drugs with the use of a portable programmable pump is safe and effective in selected patients who have failed to respond to standard medical treatment of their cancer pain. Dose titration may require rapid dose escalation, but this is usually well tolerated. For most communities embarking on such a program a programmable infusion system will be more cost-effective than a disposable system.
Full text
PDF
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Arnér S., Meyerson B. A. Lack of analgesic effect of opioids on neuropathic and idiopathic forms of pain. Pain. 1988 Apr;33(1):11–23. doi: 10.1016/0304-3959(88)90198-4. [DOI] [PubMed] [Google Scholar]
- Bruera E., Brenneis C., Michaud M., Bacovsky R., Chadwick S., Emeno A., MacDonald N. Use of the subcutaneous route for the administration of narcotics in patients with cancer pain. Cancer. 1988 Jul 15;62(2):407–411. doi: 10.1002/1097-0142(19880715)62:2<407::aid-cncr2820620227>3.0.co;2-t. [DOI] [PubMed] [Google Scholar]
- Bruera E., Brenneis C., Michaud M., Chadwick S., MacDonald R. N. Continuous sc infusion of narcotics using a portable disposable device in patients with advanced cancer. Cancer Treat Rep. 1987 Jun;71(6):635–637. [PubMed] [Google Scholar]
- Bruera E., Brenneis C., Michaud M., MacMillan K., Hanson J., MacDonald R. N. Patient-controlled subcutaneous hydromorphone versus continuous subcutaneous infusion for the treatment of cancer pain. J Natl Cancer Inst. 1988 Sep 21;80(14):1152–1154. doi: 10.1093/jnci/80.14.1152. [DOI] [PubMed] [Google Scholar]
- Campbell C. F., Mason J. B., Weiler J. M. Continuous subcutaneous infusion of morphine for the pain of terminal malignancy. Ann Intern Med. 1983 Jan;98(1):51–52. doi: 10.7326/0003-4819-98-1-51. [DOI] [PubMed] [Google Scholar]
- Drexel H., Dzien A., Spiegel R. W., Lang A. H., Breier C., Abbrederis K., Patsch J. R., Braunsteiner H. Treatment of severe cancer pain by low-dose continuous subcutaneous morphine. Pain. 1989 Feb;36(2):169–176. doi: 10.1016/0304-3959(89)90020-1. [DOI] [PubMed] [Google Scholar]
- Ferris F. D., Kerr I. G., De Angelis C., Sone M., Hume S. Inpatient narcotic infusions for patients with cancer pain. J Palliat Care. 1990 Summer;6(2):51–59. [PubMed] [Google Scholar]
- Ferris F. D., Wodinsky H. B., Kerr I. G., Sone M., Hume S., Coons C. A cost-minimization study of cancer patients requiring a narcotic infusion in hospital and at home. J Clin Epidemiol. 1991;44(3):313–327. doi: 10.1016/0895-4356(91)90043-9. [DOI] [PubMed] [Google Scholar]
- Foley K. M. The treatment of cancer pain. N Engl J Med. 1985 Jul 11;313(2):84–95. doi: 10.1056/NEJM198507113130205. [DOI] [PubMed] [Google Scholar]
- Kerr I. G., Sone M., Deangelis C., Iscoe N., MacKenzie R., Schueller T. Continuous narcotic infusion with patient-controlled analgesia for chronic cancer pain in outpatients. Ann Intern Med. 1988 Apr;108(4):554–557. doi: 10.7326/0003-4819-108-4-554. [DOI] [PubMed] [Google Scholar]
- Miser A. W., Davis D. M., Hughes C. S., Mulne A. F., Miser J. S. Continuous subcutaneous infusion of morphine in children with cancer. Am J Dis Child. 1983 Apr;137(4):383–385. doi: 10.1001/archpedi.1983.02140300061017. [DOI] [PubMed] [Google Scholar]
- Moulin D. E., Kreeft J. H., Murray-Parsons N., Bouquillon A. I. Comparison of continuous subcutaneous and intravenous hydromorphone infusions for management of cancer pain. Lancet. 1991 Feb 23;337(8739):465–468. doi: 10.1016/0140-6736(91)93401-t. [DOI] [PubMed] [Google Scholar]
- Paul D., Standifer K. M., Inturrisi C. E., Pasternak G. W. Pharmacological characterization of morphine-6 beta-glucuronide, a very potent morphine metabolite. J Pharmacol Exp Ther. 1989 Nov;251(2):477–483. [PubMed] [Google Scholar]
- Payne R., Foley K. M. Advances in the management of cancer pain. Cancer Treat Rep. 1984 Jan;68(1):173–183. [PubMed] [Google Scholar]
- Portenoy R. K., Moulin D. E., Rogers A., Inturrisi C. E., Foley K. M. I.v. infusion of opioids for cancer pain: clinical review and guidelines for use. Cancer Treat Rep. 1986 May;70(5):575–581. [PubMed] [Google Scholar]
- Sundaresan N., DiGiacinto G. V., Hughes J. E. Neurosurgery in the treatment of cancer pain. Cancer. 1989 Jun 1;63(11 Suppl):2365–2377. doi: 10.1002/1097-0142(19890601)63:11<2365::aid-cncr2820631149>3.0.co;2-t. [DOI] [PubMed] [Google Scholar]


