Abstract
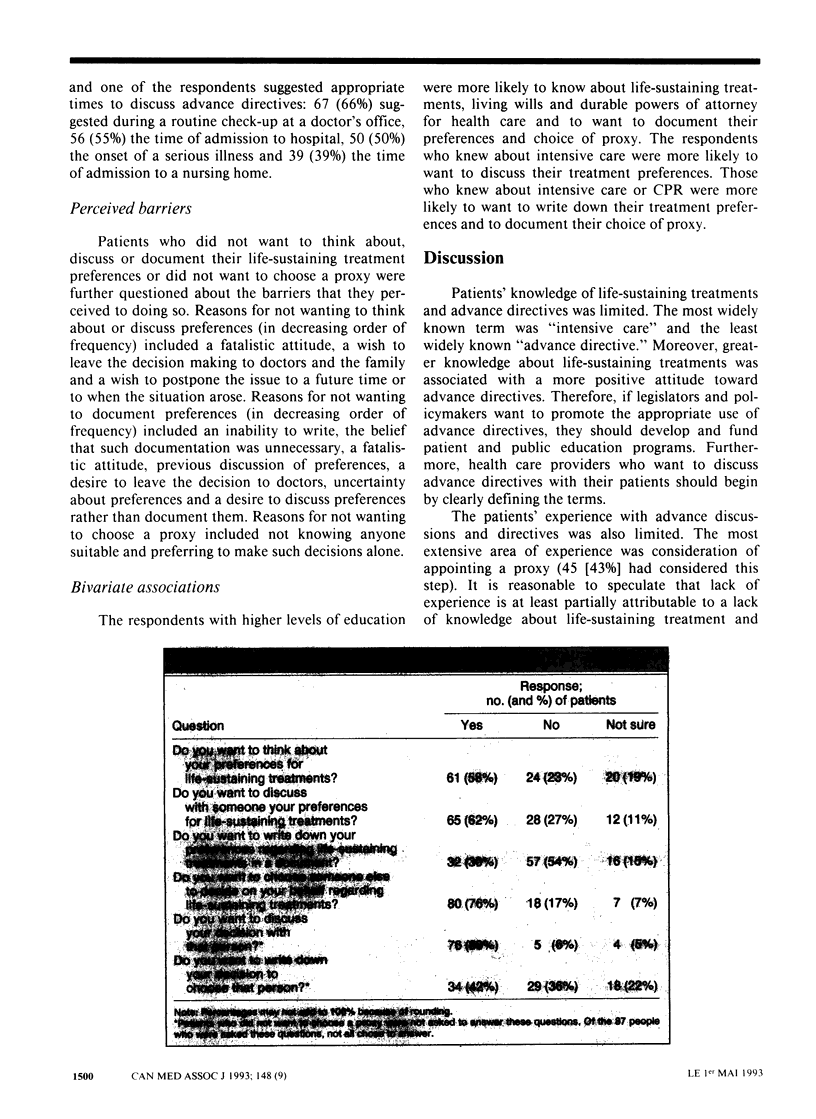
OBJECTIVE: To examine the knowledge of, previous experience with, attitudes toward and perceived barriers to completing advance directives among outpatients at two general medicine clinics. DESIGN: Cross-sectional questionnaire administered in face-to-face structured interviews. SETTING: General internal-medicine outpatient clinics at a university teaching hospital. PATIENTS: One hundred and five adult outpatients who could communicate in spoken English and who consented to be interviewed. RESULTS: Of 167 patients approached, 58 were excluded because they could not communicate in spoken English, and 4 refused to participate. Of the remaining 105 patients, 17 (16%) knew about living wills, 12 (11%) about durable powers of attorney for health care and 4 (4%) about advance directives. Twenty-three (22%) had thought about their preferences for life-sustaining treatment, 20 (19%) had discussed them, none had written them down, and 45 (43%) had thought about choosing a proxy. Sixty-one (58%) wanted to think about their preferences for treatment, 65 (62%) wanted to discuss them, 32 (30%) wanted to write them down, and 80 (76%) wanted to choose a proxy. The perceived barriers to completing an advance directive were inability to write, the belief that an advance directive was unnecessary, a fatalistic attitude, previous discussion of preferences, a desire to leave the decision to doctors, uncertainty about preferences, a desire to discuss preferences rather than document them, a desire to wait until the situation arose, a desire to write down preferences in the future and a desire to avoid thinking about preferences or advance directives. Respondents with more knowledge of life-sustaining treatments were more likely to want to complete an advance directive. CONCLUSIONS: Outpatients have positive attitudes toward advance directives, but their knowledge and experience are limited. These data underscore the need for patient education and for policies to eliminate the barriers to completing advance directives that patients face.
Full text
PDF
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Emanuel L. L., Barry M. J., Stoeckle J. D., Ettelson L. M., Emanuel E. J. Advance directives for medical care--a case for greater use. N Engl J Med. 1991 Mar 28;324(13):889–895. doi: 10.1056/NEJM199103283241305. [DOI] [PubMed] [Google Scholar]
- Ende J., Kazis L., Ash A., Moskowitz M. A. Measuring patients' desire for autonomy: decision making and information-seeking preferences among medical patients. J Gen Intern Med. 1989 Jan-Feb;4(1):23–30. doi: 10.1007/BF02596485. [DOI] [PubMed] [Google Scholar]
- Frankl D., Oye R. K., Bellamy P. E. Attitudes of hospitalized patients toward life support: a survey of 200 medical inpatients. Am J Med. 1989 Jun;86(6 Pt 1):645–648. [PubMed] [Google Scholar]
- Gamble E. R., McDonald P. J., Lichstein P. R. Knowledge, attitudes, and behavior of elderly persons regarding living wills. Arch Intern Med. 1991 Feb;151(2):277–280. [PubMed] [Google Scholar]
- Lo B., McLeod G. A., Saika G. Patient attitudes to discussing life-sustaining treatment. Arch Intern Med. 1986 Aug;146(8):1613–1615. [PubMed] [Google Scholar]
- Molloy David W., Guyatt Gordon, Alemayehu Efrem, McIlroy William E. Treatment preferences, attitudes toward advance directives and concerns about health care. Humane Med. 1991 Oct;7(4):285–290. [PubMed] [Google Scholar]
- Rye P. D., Wallston K. A., Wallston B. S., Smith R. A. The desire to control terminal health care and attitudes toward living wills. Am J Prev Med. 1985 May-Jun;1(3):56–60. [PubMed] [Google Scholar]
- Shmerling R. H., Bedell S. E., Lilienfeld A., Delbanco T. L. Discussing cardiopulmonary resuscitation: a study of elderly outpatients. J Gen Intern Med. 1988 Jul-Aug;3(4):317–321. doi: 10.1007/BF02595786. [DOI] [PubMed] [Google Scholar]
- Steinbrook R., Lo B., Moulton J., Saika G., Hollander H., Volberding P. A. Preferences of homosexual men with AIDS for life-sustaining treatment. N Engl J Med. 1986 Feb 13;314(7):457–460. doi: 10.1056/NEJM198602133140730. [DOI] [PubMed] [Google Scholar]
- Stolman C. J., Gregory J. J., Dunn D., Levine J. L. Evaluation of patient, physician, nurse, and family attitudes toward do not resuscitate orders. Arch Intern Med. 1990 Mar;150(3):653–658. [PubMed] [Google Scholar]
- Teno J., Fleishman J., Brock D. W., Mor V. The use of formal prior directives among patients with HIV-related diseases. J Gen Intern Med. 1990 Nov-Dec;5(6):490–494. doi: 10.1007/BF02600877. [DOI] [PubMed] [Google Scholar]
- Wagner A. Cardiopulmonary resuscitation in the aged. A prospective survey. N Engl J Med. 1984 Apr 26;310(17):1129–1130. doi: 10.1056/NEJM198404263101732. [DOI] [PubMed] [Google Scholar]


