Abstract
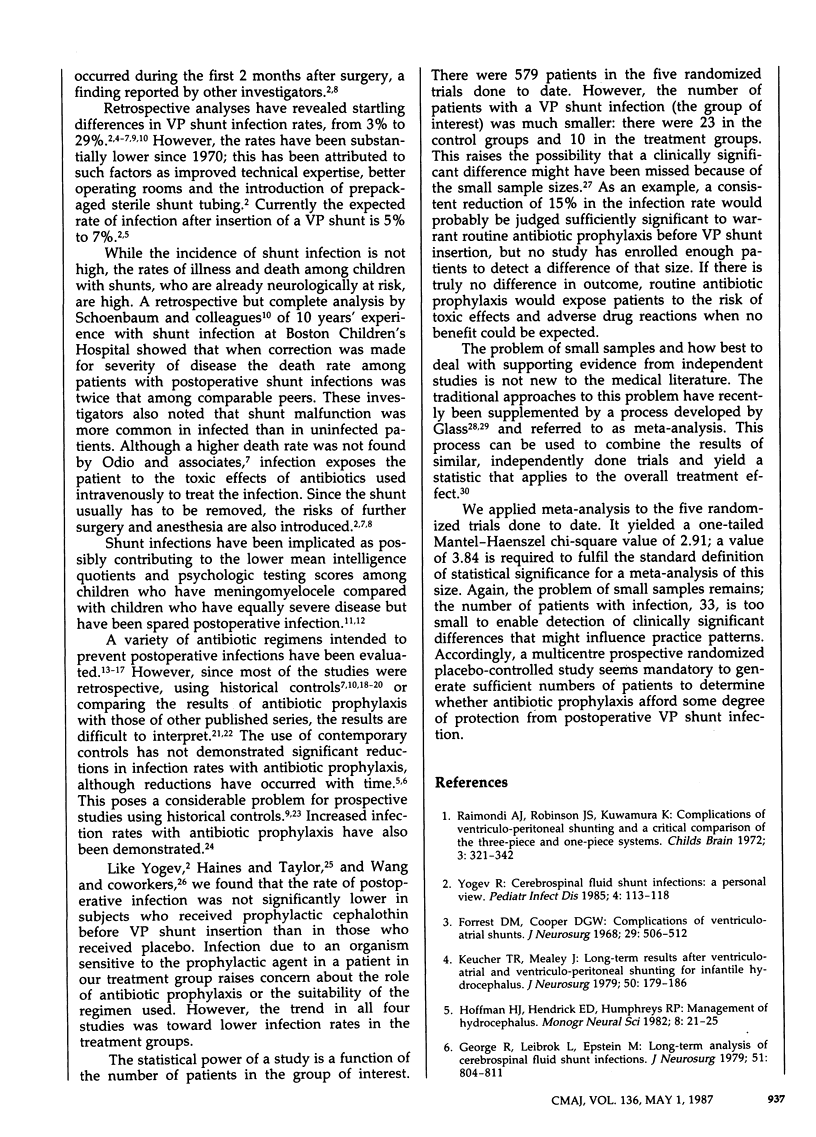
Postoperative infection is an important complication after insertion of a ventriculoperitoneal (VP) shunt in children with hydrocephalus. A randomized double-blind placebo-controlled study was performed to determine the efficacy of cephalothin in preventing postoperative shunt infection. Sixty-three children who presented for elective VP shunt insertion between January 1982 and December 1985 and who did not have a history of shunt infections were randomly assigned to receive four doses of prophylactic cephalothin, 25 mg/kg (32 patients), or of a multivitamin placebo (31 patients). Postoperative infection developed in 6% of the treatment group, compared with 10% of the placebo group, a difference that was not statistically significant, although a clinical significance may have been masked by the small sample size. A large multicentre trial is needed to determine the efficacy of antibiotic prophylaxis in reducing the incidence of postoperative VP shunt infections.
Full text
PDF
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Ajir F., Levin A. B., Duff T. A. Effect of prophylactic methicillin on cerebrospinal fluid shunt infections in children. Neurosurgery. 1981 Jul;9(1):6–8. doi: 10.1227/00006123-198107000-00002. [DOI] [PubMed] [Google Scholar]
- Bayston R. Antibiotic prophylaxis in shunt surgery. Dev Med Child Neurol Suppl. 1975;(35):99–103. doi: 10.1111/j.1469-8749.1975.tb03587.x. [DOI] [PubMed] [Google Scholar]
- Einarson T. R., McGhan W. F., Bootman J. L., Sabers D. L. Meta-analysis: quantitative integration of independent research results. Am J Hosp Pharm. 1985 Sep;42(9):1957–1964. [PubMed] [Google Scholar]
- George R., Leibrock L., Epstein M. Long-term analysis of cerebrospinal fluid shunt infections. A 25-year experience. J Neurosurg. 1979 Dec;51(6):804–811. doi: 10.3171/jns.1979.51.6.0804. [DOI] [PubMed] [Google Scholar]
- Guglielmo B. J., Hohn D. C., Koo P. J., Hunt T. K., Sweet R. L., Conte J. E., Jr Antibiotic prophylaxis in surgical procedures. A critical analysis of the literature. Arch Surg. 1983 Aug;118(8):943–955. doi: 10.1001/archsurg.1983.01390080045013. [DOI] [PubMed] [Google Scholar]
- Haines S. J., Taylor F. Prophylactic methicillin for shunt operations: effects on incidence of shunt malfunction and infection. Childs Brain. 1982;9(1):10–22. doi: 10.1159/000120031. [DOI] [PubMed] [Google Scholar]
- Ignelzi R. J., Kirsch W. M. Follow-up analysis of ventriculoperitoneal and ventriculoatrial shunts for hydrocephalus. J Neurosurg. 1975 Jun;42(6):679–682. doi: 10.3171/jns.1975.42.6.0679. [DOI] [PubMed] [Google Scholar]
- Keucher T. R., Mealey J., Jr Long-term results after ventriculoatrial and ventriculoperitoneal shunting for infantile hydrocephalus. J Neurosurg. 1979 Feb;50(2):179–186. doi: 10.3171/jns.1979.50.2.0179. [DOI] [PubMed] [Google Scholar]
- Lewis R. T. Antibiotic prophylaxis in surgery. Can J Surg. 1981 Nov;24(6):561–566. [PubMed] [Google Scholar]
- Malis L. I. Prevention of neurosurgical infection by intraoperative antibiotics. Neurosurgery. 1979 Sep;5(3):339–343. [PubMed] [Google Scholar]
- Mashford M. L., Robertson M. B., Stewart J. M. Use of prophylactic antibiotics in surgery. Med J Aust. 1980 May 31;1(11):532–534. doi: 10.5694/j.1326-5377.1980.tb135098.x. [DOI] [PubMed] [Google Scholar]
- McCullough D. C., Kane J. G., Presper J. H., Wells M. Antibiotic prophylaxis in ventricular shunt surgery. I. Reduction of operative infection rates with methicillin. Childs Brain. 1980;7(4):182–189. [PubMed] [Google Scholar]
- Nelson J. D. Cerebrospinal fluid shunt infections. Pediatr Infect Dis. 1984 May-Jun;3(3 Suppl):S30–S32. doi: 10.1097/00006454-198405001-00011. [DOI] [PubMed] [Google Scholar]
- Odio C., McCracken G. H., Jr, Nelson J. D. CSF shunt infections in pediatrics. A seven-year experience. Am J Dis Child. 1984 Dec;138(12):1103–1108. doi: 10.1001/archpedi.1984.02140500009004. [DOI] [PubMed] [Google Scholar]
- Raimondi A. J., Robinson J. S., Kuwawura K. Complications of ventriculo-peritoneal shunting and a critical comparison of the three-piece and one-piece systems. Childs Brain. 1977;3(6):321–342. doi: 10.1159/000119684. [DOI] [PubMed] [Google Scholar]
- Salmon J. H. Adult hydrocephalus. Evaluation of shunt therapy in 80 patients. J Neurosurg. 1972 Oct;37(4):423–428. doi: 10.3171/jns.1972.37.4.0423. [DOI] [PubMed] [Google Scholar]
- Savitz M. H., Katz S. S. Rationale for prophylactic antibiotics and neurosurgery. Neurosurgery. 1981 Aug;9(2):142–144. doi: 10.1227/00006123-198108000-00005. [DOI] [PubMed] [Google Scholar]
- Schoenbaum S. C., Gardner P., Shillito J. Infections of cerebrospinal fluid shunts: epidemiology, clinical manifestations, and therapy. J Infect Dis. 1975 May;131(5):543–552. doi: 10.1093/infdis/131.5.543. [DOI] [PubMed] [Google Scholar]
- Venes J. L. Control of shunt infection. Report of 150 consecutive cases. J Neurosurg. 1976 Sep;45(3):311–314. doi: 10.3171/jns.1976.45.3.0311. [DOI] [PubMed] [Google Scholar]
- Wang E. E., Prober C. G., Hendrick B. E., Hoffman H. J., Humphreys R. P. Prophylactic sulfamethoxazole and trimethoprim in ventriculoperitoneal shunt surgery. A double-blind, randomized, placebo-controlled trial. JAMA. 1984 Mar 2;251(9):1174–1177. [PubMed] [Google Scholar]
- Yogev R. Cerebrospinal fluid shunt infections: a personal view. Pediatr Infect Dis. 1985 Mar-Apr;4(2):113–118. doi: 10.1097/00006454-198503000-00001. [DOI] [PubMed] [Google Scholar]
- Yu H. C., Patterson R. H., Jr Prophylactic antimicrobial agents after ventriculoatriostomy for hydrocephalus. J Pediatr Surg. 1973 Dec;8(6):881–885. doi: 10.1016/0022-3468(73)90004-3. [DOI] [PubMed] [Google Scholar]


