Abstract
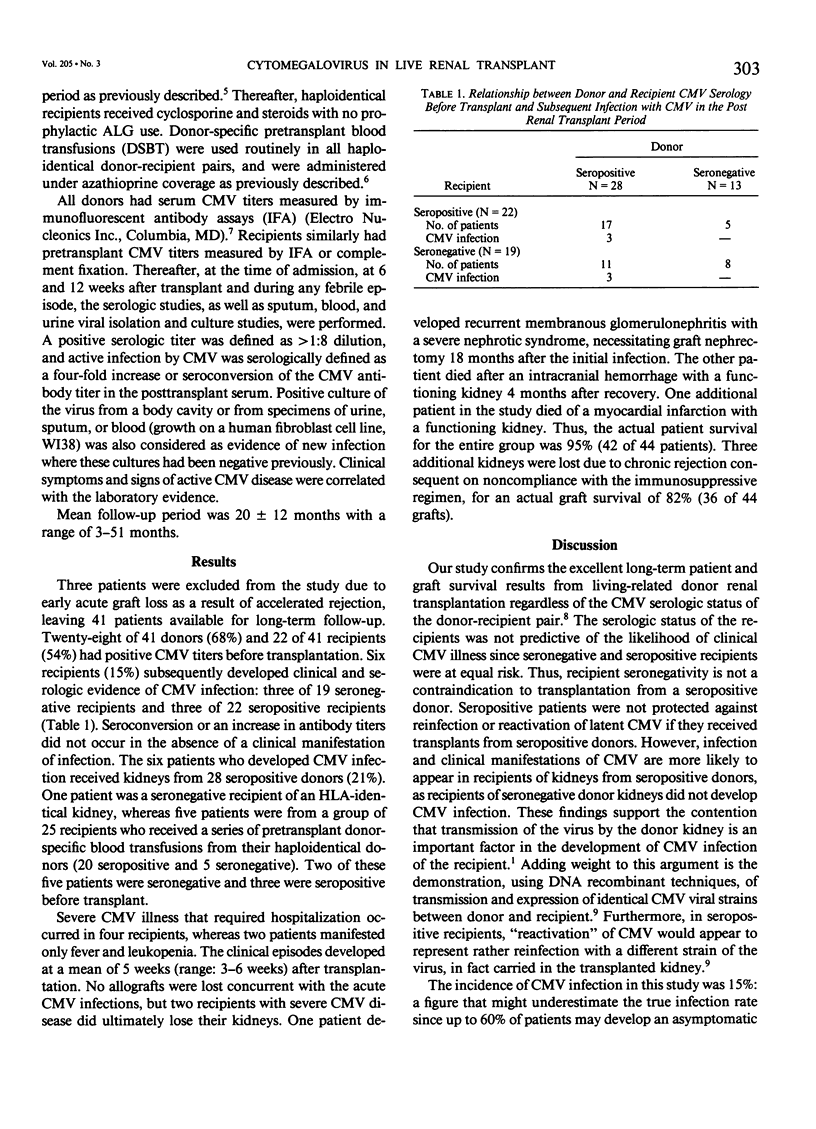
Forty-four living-related donor kidney (LRD) recipients (19 HLA-identical and 25 haploidentical) were followed prospectively to determine the posttransplant incidence and sequelae of cytomegalovirus (CMV) infection as they relate to the CMV status of recipients and donors. CMV titers were measured in all patients before transplantation by an immunofluorescent assay (IFA). Recipients similarly had CMV titers measured at selected intervals after transplant and during febrile episodes. Appropriate viral cultures were simultaneously performed. Laboratory evidence of infection was correlated with symptoms and signs of active CMV disease. Mean follow-up period was 20 +/- 12 months with a range of 3-51 months. Three patients were excluded due to early acute rejection resulting in graft loss. Twenty-eight of 41 donors (68%) and 22 of 41 recipients (54%) had positive CMV titers before transplantation. Six of 41 recipients (15%) subsequently developed clinical and laboratory evidence of CMV infection: three of 19 seronegative recipients and three of 22 seropositive recipients. All six patients received kidneys from seropositive donors. Four patients had severe CMV disease (2 seronegative, 2 seropositive), whereas two patients had leukopenia and fever only. Two patients with severe CMV infections subsequently lost their grafts due to unrelated causes. Overall, actual patient and graft survival of the entire group is 95% and 82%, respectively. In conclusion, individuals who receive LRD kidneys from seronegative individuals are unlikely to develop CMV infection, and transplantation of seropositive LRD kidneys may be associated with transmission of CMV in susceptible recipients regardless of their serologic status. With appropriate management of CMV illness in the posttransplant period, LRD kidney donation is safe and efficacious and should not be discouraged on the basis of pretransplant CMV serology in any donor-recipient pairing.
Full text
PDF
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Armstrong J. A., Tarr G. C., Youngblood L. A., Dowling J. N., Saslow A. R., Lucas J. P., Ho M. Cytomegalovirus infection in children undergoing open-heart surgery. Yale J Biol Med. 1976 Mar;49(1):83–91. [PMC free article] [PubMed] [Google Scholar]
- Bia M. J., Andiman W., Gaudio K., Kliger A., Siegel N., Smith D., Flye W. Effect of treatment with cyclosporine versus azathioprine on incidence and severity of cytomegalovirus infection posttransplantation. Transplantation. 1985 Dec;40(6):610–614. doi: 10.1097/00007890-198512000-00007. [DOI] [PubMed] [Google Scholar]
- Chou S. W. Acquisition of donor strains of cytomegalovirus by renal-transplant recipients. N Engl J Med. 1986 May 29;314(22):1418–1423. doi: 10.1056/NEJM198605293142205. [DOI] [PubMed] [Google Scholar]
- Glenn J. Cytomegalovirus infections following renal transplantation. Rev Infect Dis. 1981 Nov-Dec;3(6):1151–1178. doi: 10.1093/clinids/3.6.1151. [DOI] [PubMed] [Google Scholar]
- Morris P. J., French M. E., Dunnill M. S., Hunnisett A. G., Ting A., Thompson J. F., Wood R. F. A controlled trial of cyclosporine in renal transplantation with conversion to azathioprine and prednisolone after three months. Transplantation. 1983 Sep;36(3):273–277. doi: 10.1097/00007890-198309000-00009. [DOI] [PubMed] [Google Scholar]
- Najarian J. S., Fryd D. S., Strand M., Canafax D. M., Ascher N. L., Payne W. D., Simmons R. L., Sutherland D. E. A single institution, randomized, prospective trial of cyclosporin versus azathioprine-antilymphocyte globulin for immunosuppression in renal allograft recipients. Ann Surg. 1985 Feb;201(2):142–157. doi: 10.1097/00000658-198502000-00003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nicholson K. G. Antiviral therapy. Varicella-zoster virus infections, herpes labialis and mucocutaneous herpes, and cytomegalovirus infections. Lancet. 1984 Sep 22;2(8404):677–682. doi: 10.1016/s0140-6736(84)91233-9. [DOI] [PubMed] [Google Scholar]
- Peterson P. K., Balfour H. H., Jr, Marker S. C., Fryd D. S., Howard R. J., Simmons R. L. Cytomegalovirus disease in renal allograft recipients: a prospective study of the clinical features, risk factors and impact on renal transplantation. Medicine (Baltimore) 1980 Jul;59(4):283–300. [PubMed] [Google Scholar]
- Pollak R., Hau T., Mozes M. F. The spectrum of peritonitis in renal transplant recipients. Am Surg. 1985 Nov;51(11):617–620. [PubMed] [Google Scholar]
- Rubin R. H., Tolkoff-Rubin N. E., Oliver D., Rota T. R., Hamilton J., Betts R. F., Pass R. F., Hillis W., Szmuness W., Farrell M. L. Multicenter seroepidemiologic study of the impact of cytomegalovirus infection on renal transplantation. Transplantation. 1985 Sep;40(3):243–249. doi: 10.1097/00007890-198509000-00004. [DOI] [PubMed] [Google Scholar]
- Simmons R. L., Lopez C., Balfour H., Jr, Kalis J., Rattazzi L. C., Najarian J. S. Cytomegalovirus: Clinical virological correlations in renal transplant recipients. Ann Surg. 1974 Oct;180(4):623–634. doi: 10.1097/00000658-197410000-00028. [DOI] [PMC free article] [PubMed] [Google Scholar]


