Abstract
OBJECTIVE
To determine whether patient preferences for the use of coronary revascularization procedures differ between white and black Americans.
DESIGN
Cross-sectional survey.
SETTING
Tertiary care Department of Veterans Affairs hospital.
PATIENTS
Outpatients with and without known coronary artery disease were interviewed while awaiting appointments (n = 272). Inpatients awaiting catheterization were approached the day before the scheduled procedure (n = 80). Overall, 118 blacks and 234 whites were included in the study.
MEASUREMENTS AND MAIN RESULTS
Patient responses to questions regarding (1) willingness to undergo angioplasty or coronary artery bypass surgery if recommended by their physician and (2) whether they would elect bypass surgery if they were in either of two hypothetical scenarios, one in which bypass surgery would improve symptoms but not survival and one in which it would improve both symptoms and survival. Blacks were less likely to say they would undergo revascularization procedures than whites. However, questions dealing with familiarity with the procedure were much stronger predictors of a positive attitude toward procedure use. Patients who were not working or over 65 years of age were also less interested in procedure use. In multivariable analysis race was not a significant predictor of attitudes toward revascularization except for angioplasty recommended by their physician.
CONCLUSIONS
Racial differences in revascularization rates may be due in part to differences in patient preferences. However, preferences were more closely related to questions assessing various aspects of familiarity with the procedure. Patients of all races may benefit from improved communication regarding proposed revascularization. Further research should address this issue in patients contemplating actual revascularization.
Keywords: race, coronary artery bypass graft surgery, doctor-patient relationship, percutaneous transluminal coronary angioplasty, survey
Coronary artery disease (CAD) is the leading cause of death among blacks in this country.1,2 The risk of death from CAD in blacks is similar to that in whites for all ages combined and exceeds that of whites between the ages of 25 and 64.2,3 Further, a recent widening of the difference in life expectancy between whites and blacks has been tied to an increasing difference in rates of death due to heart disease between races.4 Despite this, numerous studies have shown that blacks are considerably less likely than whites to undergo invasive cardiovascular procedures, especially revascularization.5–8 Whites are up to 50% more likely to undergo percutaneous transluminal coronary angioplasty (PTCA),5 and three times as likely to undergo coronary artery bypass grafting (CABG).8 These results are consistent in studies using administrative and clinical data,9 in studies with prospective and retrospective data collection and in studies of specialized populations such as that served by the Department of Veterans Affairs (VA) medical system. The differences are large, reproducible, and of unexplained origin.
As many revascularization procedures are elective, it is possible that a systematic racial difference in patient preferences for procedure use contributes to this difference. Data on the likelihood that a patient will accept a recommendation to undergo a revascularization procedure are scarce. In the Coronary Artery Surgery Study (CASS), physicians recommended CABG to 46.5% of blacks and 59.4% of whites. However, only 80.5% of blacks for whom CABG was recommended actually had the procedure as compared with 90.4% of whites. Moreover, of the 4,652 whites for whom medical management was recommended, 11.6% later underwent CABG, compared with only 1% of the 100 blacks.10 Analysis of data from the weekly joint cardiology–cardiothoracic surgery conference of one VA referral center for CABG found that black patients were twice as likely as white patients to refuse a procedure when recommended (23% vs 10%) (S. Sedlis, personal communication).
Although limited, these data suggest that the racial differences in revascularization rates may, at least in part, reflect a tendency for blacks to decline these procedures or for whites to pursue them. The studies to date,10 however, have compared patients who may have had dissimilar clinical situations when they accepted or declined procedures (also S. Sedlis, unpublished results). We sought to compare the attitudes toward revascularization procedures among blacks and whites when presented with identical hypothetical clinical situations.
METHODS
Survey
A survey was developed that assessed attitudes toward procedure use as well as variables we believed would predict those attitudes. The survey, written in lay terms, was refined by pilot testing, first among black and white VA employees and then among black and white volunteer patients. Patients participating in pilot testing were not included in the final analysis. The survey included questions regarding participant age, race, education level, employment status, living arrangements, and health status, all of which may influence health behaviors. In addition, on the basis of the Health Belief Model for patient behavior and personal clinical experience,11 we believed that patient familiarity with revascularization procedures should influence attitudes toward revascularization. Therefore, familiarity was measured by asking participants to report how many family members or friends had undergone CABG, their own estimate of operative mortality of CABG, and their self-reported familiarity with CABG, phrased two ways (Are you familiar with bypass surgery? and Do you have a good idea what happens to a person who has bypass surgery?) Similar questions were asked about PTCA, except that an estimate of the risk of having complications requiring CABG was substituted for the estimate of operative mortality.
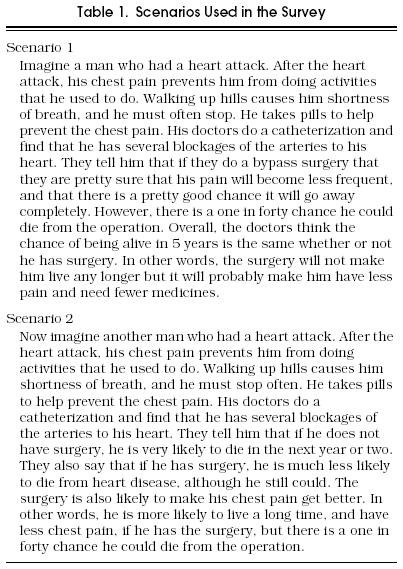
We believed that patients’ decisions to undergo a cardiovascular procedure would involve both the patients’ tendency to follow their doctors’ recommendations and their attitudes toward the procedure. Therefore, attitudes toward procedure use were assessed using two approaches. First, a question concerning CABG was asked as follows, “If your doctor recommended that you have bypass surgery to improve the blood flow to your heart, would you do so?” This was followed by a similar question about PTCA. Second, two scenarios were presented in which a man had suffered a myocardial infarction and was left with class II-III angina. In one, CABG was said to be likely to improve symptoms but not survival. In the second, CABG was said to be likely to improve both symptoms and survival. Both scenarios included an estimated operative mortality of 2.5%. The participant was then asked to comment regarding whether he would want bypass surgery if he were that person. The full scenarios, which were read aloud verbatim by a research assistant (RA), are shown in Table 1.
Table 1.
Scenarios Used in the Survey
Patients
The study population included three categories of male patients treated at the Pittsburgh VA Medical Center, a large, university-affiliated, acute care VA hospital: (1) ambulatory patients without a diagnosis of CAD (n = 216); (2) ambulatory patients who had previously undergone either PTCA or CABG (n = 77); and (3) hospitalized patients who were awaiting a scheduled cardiac catheterization (CATH) for known or suspected CAD (n = 80). Ambulatory patients were approached while they awaited appointments in the internal medicine clinic. Inpatients awaiting CATH were identified from the CATH schedule and approached in their rooms. All other inpatients awaiting CATH were asked to participate if they were not in an intensive care setting and not undergoing clinical care when approached by the RA. Trained RAs reviewed charts to identify eligible male veterans. Surveys were performed by three RAs, one black and two white. The RAs attempted to enroll all eligible blacks and as many whites as could be accommodated. Participants provided oral informed consent after being asked to participate in a survey to learn why some patients are more or less likely to agree to revascularization. As requested by the Pittsburgh VAMC’s Subcommittee on Human Studies, which approved the study, patients did not provide their names or other unique identifiers when completing the survey.
Analysis
Simple descriptive statistics were used to describe the study population. The four dependent variables (willingness to undergo PTCA if recommended, willingness to undergo CABG if recommended, and two scenarios) were categorized into yes responses and no/not sure responses. Similar results were obtained when the not sure responses were excluded. Age was examined as a continuous and categorical variable in exploratory analyses, but was dichotomized at age 65 for the final analysis.
Because the responses to the questions measuring familiarity were highly correlated with one another, factor analysis was used to determine whether a summary variable would capture the meaning in these. However, no clear summary factor was found, so each question was treated as a separate measure. Similarly, although the measures of attitude toward revascularization were correlated, we elected to report separate analyses using each of these measures as the dependent variable.
Characteristics of the black and white populations were compared using χ2 tests and Student’s t tests, as appropriate. Then χ2 tests were used to examine the association of each independent variable within the measures of attitude toward revascularization. Variables that approached (p ≤ .1) significance in univariate analyses were entered into a logistic regression, using stepwise forward selection. This analysis was repeated with race forced into the model. It was also repeated with race, inpatient/outpatient status, and previous revascularization forced into the model. We also performed univariate and multivariable analyses of each of the independent and dependent variables stratified by category (inpatient, outpatient with CAD, and outpatient without CAD). We found that these analyses yielded no evidence of heterogeneity across categories, so only the analyses of all three categories combined are presented.
Because of concern that the race of the person administering the survey might affect patient responses, we compared attitudes toward revascularization among participants who were interviewed by black and white RAs, using χ2 testing.
Survey data were entered into a computerized database, then verified after they had been converted into an SAS file. All statistical analyses were carried out using SAS statistical software in a Windows 3.11 environment (PC SAS for Windows 3.11, version 6.08).12
RESULTS
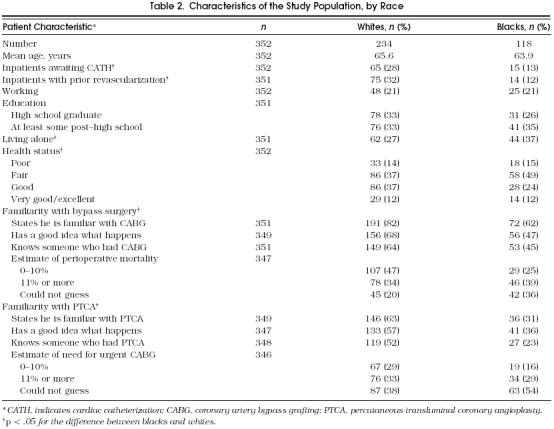
Overall, 373 patients were interviewed. Patients who could not be classified as either white or black were excluded, as were those whose interview was discontinued before at least one of the outcome variables had been answered, usually to avoid interfering with clinical care (n = 21). The characteristics of the remaining 352 patients are presented in Table 2. Blacks and whites were similar in age, working status, and education, but black patients reported worse health status, were more likely to live alone, and were less familiar with each of the revascularization procedures. Black patients were also less likely to have had a previous revascularization or to be awaiting CATH.
Table 2.
Characteristics of the Study Population, by Race
Overall, 65.7% of participants said they would choose CABG given the scenario in which it would improve symptoms but not survival, compared with 84.4% who would choose it if CABG improved both symptoms and survival. When asked whether they would undergo a PTCA if their doctor recommended it, 64.2% said yes. The comparable number for doctor-recommended CABG was 72.1%.
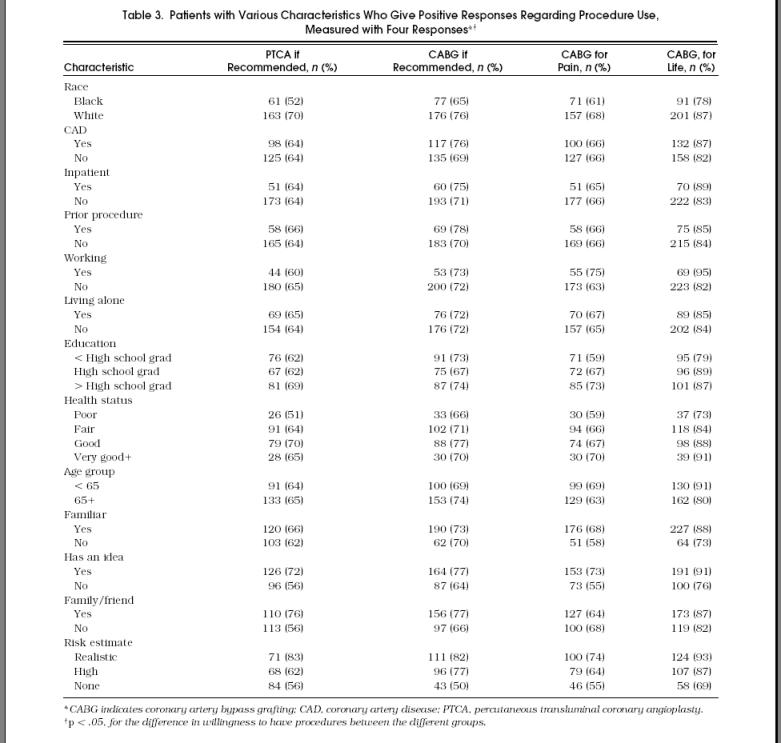
In univariate comparisons (Table 3), whites were generally more inclined to undergo procedures than blacks for each of the outcome variables. Each of the measures of increased patient familiarity with revascularization (self-report as “familiar” with the procedure, having a “good idea” what happens when one undergoes it, having a family member or friend who had a procedure, or having a realistic estimate of risk) was correlated with a more positive attitude toward revascularization, frequently to a significant degree (Table 3). However, none of age, education, employment, living situation, health status, history of previous revascularization, or being in the hospital awaiting CATH predicted responses favoring revascularization.
Table 3.
Patients with Various Characteristics Who Give Positive Responses Regarding Procedure Use, Measured with Four Responses
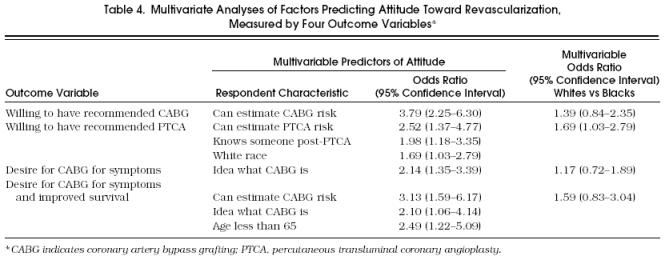
In the multivariate analysis (Table 4), measures of familiarity with the procedure were the most important predictors of attitude toward revascularization. For each of the dependent variables the pattern of predictors was slightly different, but one of the questions we had devised to measure familiarity was always the more powerful predictor. Race did enter the model predicting willingness to undergo PTCA if the patient’s doctor so advised. When race was forced into the other models, it did not approach statistical significance, although in each case the responses of black participants tended to be less favorable toward procedure use. In addition, veterans less than 65 years of age were more likely to choose CABG given the scenario in which it improved both survival and symptoms, even after controlling for familiarity with the procedure. When these analyses were repeated with inpatient status and history of previous procedure use forced into the model, the results were unchanged.
Table 4.
Multivariate Analyses of Factors Predicting Attitude Toward Revascularization, Measured by Four Outcome Variables*
In univariate analysis, race of the interviewer also appeared to have some influence on black participants’ preferences for opting for revascularization procedures. For each dependent variable, black patients were more likely to state they would opt for a procedure when surveyed by a black RA rather than a white RA. These differences ranged from 20% for having a PTCA if the doctor recommended one to 12% for having a CABG when presented a scenario in which it would improve survival as well as symptoms. These differences approached, but did not achieve, statistical significance. White participants had similar responses whether they were interviewed by a white or a black RA (data not shown).
DISCUSSION
In this survey of more than 350 black and white patients, we found that whites were more likely to say they would undergo revascularization if recommended by their physician, and to say they would elect CABG if they were in a situation in which it would be likely to improve symptoms and long-term survival. This finding is consistent with previous work that has found that among patients offered CABG, blacks are less likely to actually undergo the procedure.10 Unlike these previous findings, which may have reflected differences in clinical characteristics among blacks and whites offered CABG, our study design controls for different clinical scenarios by providing all patients with identical situations. In addition, we were able to show that much of the black-white difference in patient preferences seemed to be explained by questions that addressed familiarity with the procedures in different ways. When these questions are included in multivariate models, race is a significant predictor of only one of four measures of attitudes. Finally, although these findings are based on small numbers of patients, it is also interesting that these differences were smaller when the interviewer was also black.
We have been unable to identify analogous studies of patient preferences for procedure use in the literature. However, several studies have found that blacks are more likely to delay seeking care for chest pain than whites, although at least one suggested this may reflect primarily socioeconomic differences.13–15 Several authors have suggested that this may be because black patients are less familiar with signs and symptoms of coronary heart disease.16,17 Lack of knowledge concerning heart disease symptoms might lead to different responses to symptoms of chest pain, but it is not clear how this would result in different attitudes toward revascularization among black patients.16,18 Another possibility is that blacks are more averse to using the medical system in general, perhaps reflecting previous negative experiences with it.19,20 Our survey did not address this possibility.
Other factors that may be important for understanding racial differences in the decision to accept or elect revascularization procedures are identified in the Health Belief Model.11 This model suggests that decision making is affected by a number of factors including beliefs about individual vulnerability to disease and the seriousness of disease and confidence in treatment efficacy, balanced against perceived barriers to care.21 Our finding that familiarity with the procedure was associated with procedure use would seem consistent with this model.
We should note that the grouping of our questions measuring familiarity is based on our theoretical perception that these questions would all measure the same construct in different ways. Our inability to group these with factor analysis, despite their having significant collinearity, suggests that more than one construct is being measured by these questions. More detailed studies using larger numbers of patients and different formulations of these questions may clarify the constructs that are truly important to the decision making process.
The consistent trend for black patients to be more likely to say they would choose revascularization when surveyed by a black RA as opposed to a white RA is also consistent with earlier reports. Brooks reported that 24% of black patients are dissatisfied with clinic visits, and attributed this to communication barriers, use of medical jargon, lack of warmth and friendliness by physicians, and perhaps a distrust of whites.22 As blacks make up 12% of the U.S. population but comprise only 3% of physicians,23 and even fewer subspecialists, most black patients facing an invasive cardiac procedure will be counseled by a physician who is not black. Thus, it is plausible that racial incongruity between patient and physician may contribute to the lower revascularization rates among blacks. One should consider that this analysis was not a part of our original study design. It also should be noted that the RAs, who did not have medical training, simply posed the two questions and read the scenarios verbatim, as they appear in Table 1, a much different situation than that of a physician counseling a patient. Nonetheless, our results raise the possibility that increasing the number of minority physicians in the workforce, particularly in subspecialty positions, may decrease differences in procedure use between blacks and whites.
There are several limitations to this study. Most importantly, answers were purely hypothetical. Actual decision making, for example in the setting of an acute ischemic event, might be considerably different as this situation would presumably lead to marked changes in one’s perceived susceptibility to disease, as well as its seriousness. However, it is interesting that the 10% higher proportion of whites who said they would agree to CABG if their doctor recommended it is similar to the difference in acceptance rates of CABG among patients in the CASS registry.10
Second, although we asked participants to answer questions about a hypothetical situation, they may have considered their own condition in deciding whether or not to elect CABG in the scenarios presented. It is possible that the racial differences in responses that we found reflected differences in the participants’ clinical situation, rather than differences in attitudes.
Third, because all participants were patients at the Pittsburgh VAMC, they may not be representative of blacks and whites across the country. For example, patients who use the VA medical system are more likely to be male, poor, and have a lower level of education than other Americans.24 A population that included women, had higher incomes, or was more highly educated might have given different responses. On the other hand, by studying men who use the VA, we minimize the potential confounding of race by differences in income and education. Moreover, it is unlikely that the physicians caring for black and white participants in this study had made systematically different attempts at patient education, as the same internal medicine and cardiology faculty supervise or provide directly the primary and cardiac care for these patients.
In addition, the fact that we used a convenience sample, rather than a truly random sample, may have yielded an unrepresentative population. Patients who were available for an interview may be more or less willing to undergo procedures than the population in general. However, it is our impression that the vast majority of patients in this VA clinic arrive significantly in advance of their scheduled appointment, in time to be a candidate for the present study. Fewer than 5% of patients who were approached did not agree to be interviewed.
Finally, our study did not address whether increasing patient familiarity with the procedures would have led to changes in attitudes. Indeed, because it relied on self-report, we cannot be sure whether we measured familiarity with a procedure or simply the desire to appear knowledgeable. Similarly, our study could not determine whether the lack of familiarity with procedures was secondary to other attitudes such as fear or distrust of invasive procedures or the medical system in general, which might have prevented gaining familiarity with CABG or PTCA.
We believe these results provide direction for researchers and clinicians concerned about patterns of use of revascularization procedures. First, the present results should be replicated in patients who are actually facing a decision regarding whether or not to proceed to a revascularization procedure, as well as in a more scientifically selected sample of the general population. This is particularly important for patients for whom revascularization would be medically necessary—that is, when revascularization is clearly beneficial and better than any other alternative.
Second, clinicians should be careful to ensure that lower levels of familiarity with CABG and PTCA at baseline do not lead to uninformed decision making, regardless of patient race. Unfortunately, physicians may spend more time explaining risks and benefits of procedures to patients who are well educated, and paradoxically give less information to those patients who are least familiar with proposed treatments.22 Thus, clinicians should be careful to assess baseline levels of familiarity with procedures when discussing recommendations with patients. If unfamiliar with the procedure, patients could be exposed to tailored educational programs before being asked to make a decision. This might be especially important if the patients have not been exposed to such decision making, for example among friends and relatives, in the past.
Acknowledgments
Barbara Hanusa, PhD, helped us with the analysis of the data and performed the factor analyses.
References
- 1.Oberman A, Cutter G. Issues in the natural history and treatment of coronary heart disease in black populations: surgical treatment. Am Heart J. 1984;108:688–94. doi: 10.1016/0002-8703(84)90656-2. [DOI] [PubMed] [Google Scholar]
- 2.Gillum RF. Coronary heart disease in black populations, 1: mortality and morbidity. Am Heart J. 1982;104:839–51. doi: 10.1016/0002-8703(82)90021-7. [DOI] [PubMed] [Google Scholar]
- 3.Watkins LO. Epidemiology of coronary heart disease in black populations: methodological proposals. Am Heart J. 1984;108:635–40. doi: 10.1016/0002-8703(84)90648-3. [DOI] [PubMed] [Google Scholar]
- 4.Kochanek KD, Maurer JD, Rosenberg HM. Why did black life expectancy decline from 1984 through 1989 in the United States? Am J Public Health. 1994;84:938–44. doi: 10.2105/ajph.84.6.938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Whittle J, Conigliaro J, Good CB, Lofgren RP. Racial differences in the use of invasive cardiovascular procedures in the Department of Veterans Affairs medical system. N Engl J Med. 1993;329:621–7. doi: 10.1056/NEJM199308263290907. [DOI] [PubMed] [Google Scholar]
- 6.Wenneker MB, Epstein AM. Racial inequalities in the use of procedures for patients with ischemic heart disease in Massachusetts. JAMA. 1989;261:253–7. [PubMed] [Google Scholar]
- 7.Hannan EL, Kilburn H, Jr, O’Donnell JF, Lukacik G, Shields EP. Interracial access to selected cardiac procedures for patients hospitalized with coronary artery disease in New York State. Med Care. 1991;29:430–41. doi: 10.1097/00005650-199105000-00004. [DOI] [PubMed] [Google Scholar]
- 8.Goldberg KC, Hartz AJ, Jacobsen SJ, Krakauer H, Rimm AA. Racial and community factors influencing coronary artery bypass graft surgery rates for all 1986 Medicare patients. JAMA. 1992;267:1473–7. [PubMed] [Google Scholar]
- 9.Johnson PA, Lee TH, Cook EF, Rouan GW, Goldman L. Effect of race on the presentation and management of patients with acute chest pain. Ann Intern Med. 1993;118:593–601. doi: 10.7326/0003-4819-118-8-199304150-00004. [DOI] [PubMed] [Google Scholar]
- 10.Maynard C, Fisher LD, Passamani ER, Pullum T. Blacks in the Coronary Artery Surgery Study (CASS): race and clinical decision making. Am J Public Health. 1986;76:1446–8. doi: 10.2105/ajph.76.12.1446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Rosenstock IM. Historical origins of the Health Belief Model. Health Educ Monogr. 1974;2:328–35. [Google Scholar]
- 12. SAS Institute Inc. SAS Language and Procedures: Usage, Version 6. Cary, NC: SAS Institute Inc., 1989.
- 13.Cooper RS, Simmons B, Castaner A, Prasad R, Franklin C, Ferlinz J. Survival rates and prehospital delay during myocardial infarction among black persons. Am J Cardiol. 1986;57:208–11. doi: 10.1016/0002-9149(86)90892-1. [DOI] [PubMed] [Google Scholar]
- 14.Ell K, Haywood LJ, Sobel E, deGuzman M, Blumfield D, Ning J-P. Acute chest pain in African Americans: factors in the delay in seeking emergency care. Am J Public Health. 1994;84:965–70. doi: 10.2105/ajph.84.6.965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Strogatz DS. Use of medical care for chest pain: differences between blacks and whites. Am J Public Health. 1990;80:290–4. doi: 10.2105/ajph.80.3.290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Raczynski JM, Taylor H, Cutter G, Hardin M, Rappaport N, Oberman A. Diagnoses, symptoms, and attribution of symptoms among black and white inpatients admitted for coronary heart disease. Am J Public Health. 1994;84:951–6. doi: 10.2105/ajph.84.6.951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Folsom AR, Sprafka JM, Luepker RV, Jacobs DR. Beliefs among black and white adults about causes and prevention of cardiovascular disease: the Minnesota Heart Survey. Am J Prev Med. 1988;4:121–7. [PubMed] [Google Scholar]
- 18.Davis IJ, Brown CP, Allen F, Davis T, Waldron D. African-American myths and health care: the sociocultural theory. J Natl Med Assoc. 1995;87:791–4. [PMC free article] [PubMed] [Google Scholar]
- 19.Blendon RJ, Aiken LH, Freeman HE, Corey CR. Access to medical care for black and white Americans: a matter of continuing concern. JAMA. 1989;261:278–81. [PubMed] [Google Scholar]
- 20.Bailiey EJ. Sociocultural factors and health care–seeking behavior among black Americans. J Natl Med Assoc. 1987;79:389–92. [PMC free article] [PubMed] [Google Scholar]
- 21.Horner RD, Oddone EZ, Matchar DB. Theories explaining racial differences in the utilization of diagnostic and therapeutic procedures for cerebrovascular disease. Milbank Q. 1995;73:443–62. [PubMed] [Google Scholar]
- 22.Brooks TR. Pitfalls in communication with Hispanic and African-American patients: do translators help or harm? J Natl Med Assoc. 1992;84:941–7. [PMC free article] [PubMed] [Google Scholar]
- 23.King G, Bendel R. A statistical model estimating the number of African-American physicians in the United States. J Natl Med Assoc. 1994;86:264–72. [PMC free article] [PubMed] [Google Scholar]
- 24.Assistant Secretory for Finance and Planning, Office of Planning and Management Analysis. Washington, DC: Department of Veterans Affairs; 1990. Department of Veterans Affairs. Survey of Medical System Users. [Google Scholar]


