Cataract surgery is the commonest single surgical procedure carried out in the developed world. In the developing world, cataract remains the commonest cause of blindness. In 1990 an estimated 37 million people were blind worldwide—40% of them because of cataract.1 Every year, an extra 1-2 million people go blind. Every five seconds one person in our world goes blind, and a child goes blind every minute. In 75% of these cases the blindness is treatable or preventable. However, 90% of blind people live in the poorest sections of the developing world, and without proper interventions the number of blind people will increase to 75 million by 2020.
Various aspects of the surgery for age related cataract have changed substantially in the past five years, and the quality of outcome, plus the improved safety of the modern procedure,2 has in part driven the increase in numbers of procedures performed.
What causes cataract
Most cataracts arise because of ageing of the crystalline lens. As new lens fibres continue to be laid down in the crystalline lens, and existing ones are not replaced, the lens is unusual in being one of the few structures of the body that continues to grow during life. The transparency of the lens is maintained by many interdependent factors that are responsible for its optical homogeneity, including its microscopic structure and chemical constituents. With ageing, there is a gradual accumulation of yellow-brown pigment within the lens, which reduces light transmission. There are also structural changes to the lens fibres, which result in disruption of the regular architecture and arrangement of the fibres that are necessary to maintain optical clarity.
Extrinsic factors associated with cataract formation vary with socioeconomic and geographical differences (box 1). In the developing world a multitude of factors—such as malnutrition, acute dehydrating diseases at young age, and exposure to excessive ultraviolet rays—seem to be important. In many developing countries cataracts are common in young adults, frequently associated with atopic disorders and their treatment as well as with diabetes. Other causes of cataract include trauma in a variety of forms—direct penetration, contusion, radiation, electrical, or metabolic—and congenital disorders. This review deals with age related cataract only.
Summary points
Cataract is not always due to ageing
Cataract symptoms vary depending on type of cataract and the patient's lifestyle and visual requirements
Cataract surgery in the developed world is undertaken when the benefit from removal of symptoms outweighs the small risks attached to modern surgery
After surgery, 85-90% of patients should obtain vision sufficient to meet the requirements for driving in most countries
New implant technology promises to improve the image quality and conquer the problems of presbyopia (the need for spectacles to read)
Posterior capsule opacification 2-5 years after surgery is still a problem in many cases
Data sources and selection criteria
There is not a strong evidence base for a significant part of cataract surgery intervention. However, we took into account the Cochrane review of surgical intervention for age related cataract and the Clinical Evidence chapter on cataract when we wrote this review. Other sources of expert opinion have been the Royal College of Ophthalmologists and the American Academy of Ophthalmology, both of which publish guidelines on management of cataract.
One of the authors is a former president of the United Kingdom and Ireland Society of Cataract and Refractive Surgeons and attends the annual meeting of that organisation as well as those of the European and American societies. He is therefore well placed to be aware of current clinical practice.
Symptoms of cataracts
Optometrists or primary care physicians often note lens opacities in patients, which technically would mean that the patients have cataracts. In practice, however, we usually restrict the term cataract to the situation when opacities are causing symptoms or substantially degrading the visual image.
Box 1: Main extrinsic factors associated with cataract formation3-5
Developed world
Smoking
Diabetes
Use of systemic corticosteroids
Additional important factors in the developing world
Diet (malnutrition)
Acute dehydrating diseases
Cumulative exposure to sunlight (ultraviolet B)
Cataracts are often described in terms of the part of the lens that is principally affected. There are many subdivisions in a full classification, and these can be helpful in ascribing different levels of symptoms to different subtypes of cataract. For generalists, however, the simple trio of nuclear, cortical, and subcapsular cataract is sufficient (see box 2).
Decisions for surgery
Developed world
There is no hard and fast rule about when to operate for cataract (fig 1). Essentially, surgery is considered when the likely improvement in vision compared with current problems make it worth taking the risk of serious, sight threatening complications (although these are now uncommon with modern surgical practice). In the past, a combination of relatively crude surgical techniques and poor visual rehabilitation afterwards (no lens implants) meant that cataracts were left until they were very advanced (“ripe”) before surgery was undertaken. However, as techniques have become more sophisticated (and safer) and the visual results have improved,6-8 surgery is undertaken at a much earlier stage. Indeed, the risks of serious complications may now be greater if the cataract has been left to an advanced stage.9
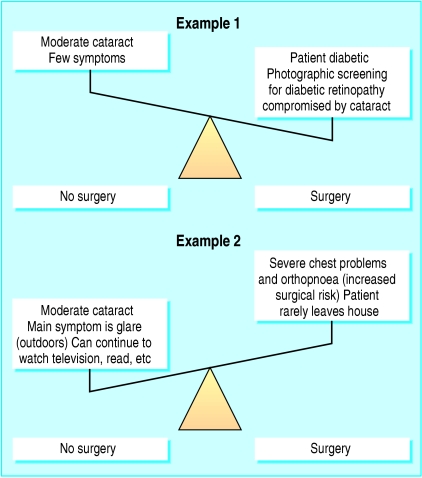
Fig 1.
Examples of two different risk-benefit considerations in patients with moderate cataract
Box 2: Main effects of different types of cataract
Nuclear cataract
Gradually reduced contrast
Reduced colour intensity
Reading often surprisingly good for level of Snellen acuity
Difficulty in seeing golf balls, car number plates, etc
Difficulty in recognising faces
Additional effects important in the developing world
Difficulty in working in fields at dusk
Cortical cataract
Light scatter from localised opacities and disruption of smooth light transmission
Problems with glare when driving
Difficulty reading
Sunlight uncomfortable in winter when sun low on horizon (northern and southern latitudes)
Additional effects important in the developing world
Difficulty in night driving
Compatible with daytime activities as the pigmented iris remains constricted
Subcapsular cataract
Visually disabling in good lighting—less trouble at low light levels when pupil is dilated
Difficulty in daytime driving
Difficulty in reading
Additional effects important in the developing world
Visually disabling as sunlight can be particularly bright
Developing world
In the developing world the problem of cataract blindness is much greater, as most people do not seek advice until the cataract is advanced or an eye has developed painful loss of vision caused by lens induced glaucoma. Some of the reasons for this are lack of awareness about cataract treatment, sex bias, low socioeconomic conditions, and lack of an old age maintenance plan by government. Many countries do not have enough clinicians to meet the demand,10,11 and most existing doctors prefer to settle in larger cities because more rural areas have inadequate infrastructure and education and civic amenities. This has resulted in a gross disparity in the distribution of eye care services.
Free diagnostic and treatment services organised by the National Plan for Control of Blindness (NPCB), District Blindness Control Society Programme, and non-governmental organisations in rural areas have helped to reduce the burden of blindness to a great extent, but the backlog for cataract surgery remains large. Also in these mass surgery programmes, the quality of the outcome is not always satisfactory. VISION 2020: The Right to Sight, a global initiative jointly launched by the World Health Organization and the International Agency for the Prevention of Blindness together with more than 20 international non-governmental organisations involved in eye care and preventing and managing blindness, aims to eliminate avoidable blindness by the year 2020 (www.v2020.org/main_page.asp). The World Health Assembly has adopted a resolution to provide more support for the Vision 2020 initiative.12
In the developing nations the lack of awareness in patients and their high threshold of tolerance has led to an inadequate emphasis on counselling before cataract surgery.
Cataract surgery
There are two generic terms for cataract extraction—intracapsular and extracapsular.
Intracapsular extraction involves removing the whole lens still within its intact capsule. This technique is no longer used in the developed world (except in rare specific circumstances) as the visual results are generally poorer and the operative and postoperative complications greater than with the alternative. It remains common in the developing world, however, because it requires less costly and sophisticated instruments, there is less dependency on back-up services and a reliable electricity supply, and it can be performed after a minimum of training.
Extracapsular extraction involves removing the lens from its capsule, which is retained within the eye and acts as a barrier between the anterior and posterior segments as well as forming the most usual site for replacement lens implantation. In manual extracapsular extraction the nucleus of the lens is removed en bloc, and therefore requires a relatively large incision.
Phacoemulsification
Phacoemulsification, part of most modern extracapsular extractions, uses sophisticated machinery to break the nucleus down into a mixture of emulsion and small pieces that can be aspirated through an irrigation-aspiration dual lumen system. This can be done through a small incision—around 3 mm commonly, but the latest developments allow removal through an incision of only 2 mm. There are two main advantages with the small incision. Firstly, there is less alteration to the shape of the cornea (which accounts for two thirds of the focusing in the eye), giving better unaided vision. Secondly, the surgery is performed within a closed environment with more control, and less fluctuation, of intraocular pressure, etc.
Clinical consensus is that phacoemulsification is less invasive, has fewer complications, and results in quicker and more stable visual rehabilitation than other techniques. As a result, there has been only one well controlled randomised trial comparing phacoemulsification and foldable intraocular lens implant with manual extracapsular extraction with a rigid implant.8 The outcome of this study agreed with the clinical consensus. However, this technique does require sophisticated equipment (with appropriate support), a good quality operating microscope, and a reliable power supply.
In phacoemulsification a small incision is made, usually at the edge of the cornea (fig 2). A viscoelastic substance is injected into the anterior chamber of the eye to maintain the space and protect the endothelium of the cornea during the rest of the procedure. A round continuous tear is made in the anterior capsule of the cataractous lens—about 5 or 6 mm in diameter. This allows access to the contents of the lens, which are removed by the phacoemulsification handpiece. Once the lens capsule is empty, further viscoelastic substance is injected into it to maintain the space while the foldable replacement lens implant is put into the capsule (fig 3). After removing the viscoelastic material, the surgeon carefully checks the incision to ensure that it is watertight. A suture is rarely needed. Injecting a bolus of cefuroxime into the anterior chamber at the end of the surgery significantly reduces the incidence of postoperative infected endophthalmitis.13
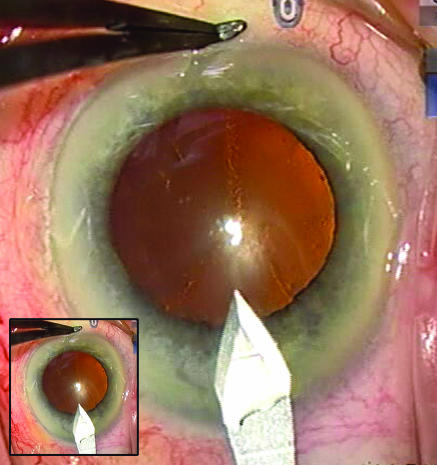
Fig 2.
Cornea with 2.2 mm incision made in it for cataract surgery. The whole procedure will be carried out through this incision. (Inset shows the actual size of the cornea)
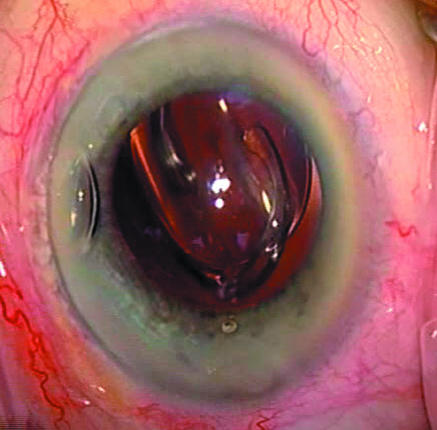
Fig 3.
Foldable intraocular lens starting to unfold in the empty lens capsule after insertion via a special cartridge
Small incision cataract surgery
In the developing world the lack of trained surgeons and appropriate infrastructure mean phacoemulsification is often not possible. Sutureless manual cataract surgery (known as small incision cataract surgery) is increasingly used as a substitute. In this technique a self sealing incision of about 6.0 mm is made outside the limbus. A tear is made in the anterior capsule, and the firmer portion of the cataract (nucleus) is expressed out of the eye through this incision. When done properly this technique can be performed rapidly, and suturing the incision is seldom needed, making it appropriate for high volume surgery.14,15 Although the results are not as predictable as with phacoemulsification, it gives an acceptable outcome and has proved to be economically viable in the developing world. Extracapsular cataract extraction with good micro-surgical technique is important in high volume centres as the technique is affordable,16 and in such centres this technique involves fewer postoperative complications.17,18
In developing countries most surgery involves a rigid intraocular lens rather than a foldable one because of the latter's substantially greater cost.
Tips for non-specialists
Patients with visual symptoms from cataract may still have good Snellen visual acuity
Optometrists may report cataract in patients who have no visual symptoms. If their vision is good they do not require referral for cataract assessment
Patients with nuclear sclerosis or nuclear cataract often have such gradual loss of vision that they may not complain of poor vision despite an acuity of 6/18 (20/60, 0.3) or worse. It is worth referring them
The presence of age related macular degeneration does not in itself rule out the possibility of cataract surgery
Let the surgeon know if your patient is using α1 adrenoceptor blocking drugs (especially tamsulosin for benign prostatic hyperplasia) because these can cause considerable problems for the surgeon during the operation
As a rule, no changes are required to anticoagulant and aspirin treatments before cataract surgery, but the anticoagulant control (international normalised ratio) should be within the therapeutic range to avoid excess risk of haemorrhage
General anaesthetic is rarely needed, although some patients will have intravenous sedation, particularly useful in cases of severe anxiety or head tremor
In the first two weeks after surgery any sudden reduction in vision or start of pain in the operated eye may herald infected endophthalmitis and requires immediate referral to an emergency eye service
A patient's story
George Coates (aged 72) had cataracts diagnosed after fairly rapid deterioration of his vision. This was a crushing blow to George, who needs to be able to drive in order to visit his disabled daughter and to help care for his young grandchildren.
George says: “I have never worn glasses in my life, and my sight had been very good until 2003, when my eyesight was deteriorating extremely rapidly until I was virtually blind in one eye. My wife and I look after our son's two children three full days a week, and I need my sight to be able to drive them around. My daughter suffered from spina bifida at birth, and both she and her husband are in wheelchairs, so I also need to be able to get to their house every day.”
George feels that the operation was quick and painless, although the prospect of the surgery had left him feeling daunted. He was surprised at how short a time he spent at the hospital on the day of surgery and how quickly his sight returned to a good level.
Outcomes
Outcomes from modern cataract surgery are much better than they were 20 years ago—because of fewer operative and postoperative complications and significant improvements in uncorrected visual acuity. Of all patients undergoing cataract surgery, 85-90% will have 6/12 (20/40 or 0.5) best corrected vision, and this figure rises to around 95% in patients who have no ocular comorbidity such as macular degeneration, diabetic retinopathy, or glaucoma.19 Because the surgery involves substitution of the patient's natural lens with an artificial implant, selecting the correct optical power of the replacement lens is crucial. Most patients wish to be left with good unaided distance vision, but some (usually those already short sighted) wish to be left with a degree of myopia so that their best unaided vision is at a closer distance (such as for reading).
In the developed world expectations about the quality of postoperative unaided vision are high. However, the refractive outcome is not always as predicted (so called refractive surprise), and patients who had not previously required glasses for distance vision but who require them after surgery can be extremely disappointed. Procedures to deal with this eventuality are available (such as exchanging the intraocular lens or adding another one and refractive laser surgery), and these may be appropriate depending on individual circumstances.
In the developing world, the impact of rapid visual rehabilitation compensates for the extra cost of the intraocular lens used in the procedure. Saving the economic costs of workforce loss from blindness, and the costs of the socioeconomic support required for blind people, significantly favours modern cataract surgery.
Complications
Although small incision extracapsular surgery is safer than earlier techniques, complications do still occur. During surgery, the posterior capsule can be ruptured, and this can lead to loss of part or all of the nucleus into the posterior segment. More commonly, however, it leads to prolapse of the vitreous body into the anterior segment. The prolapsed vitreous material must be carefully and meticulously removed from the area of incision and from the site of lens implantation. Rupture of the posterior capsule (with or without loss of vitreous humour) is reported to occur in 2-4% of operations. Capsule rupture is associated with an increased incidence of infected endophthalmitis, cystoid macular oedema, and retinal detachment.
Patients should be aware that some complications can lead to loss of functional vision in the operated eye. Many surgeons put the risk of this at around 0.1%, mainly as a result of three specific complications—infected endophthalmitis, choroidal or suprachoroidal haemorrhage, and retinal detachment. This is particularly important, of course, if the fellow eye does not have useful vision.
In developing countries, endophthalmitis remains a major concern. The periodic outburst of sporadic or cluster cases in mass cataract surgery “camps” remains a challenge for the organisations involved.
Unanswered research questions
Can the onset of cataract be delayed or prevented, particularly with regard to environmental factors and diet and ways of preventing some of the cytoskeleton and lens fibre degeneration seen in the ageing lens?
Preventing posterior capsule opacification: Can we and should we remove all the lens epithelial cells to prevent their proliferation? Can we modulate the behaviour of residual cells and prevent proliferation or fibrosis? Can we design a fully effective barrier to prevent proliferation or fibrosis encroaching on the area of the intraocular lens optic?
How can we prevent macular oedema after surgery?
What are the most desirable residual optical aberrations for maximal visual performance?
What type of intraocular lens design can best restore good vision over the full range of distances, as in the young adult eye?
Recent developments
Various improvements in surgical technique, each relatively minor, have cumulatively resulted in greatly increased efficiency. Phacoemulsification equipment has become more sophisticated, partly as a result of better understanding of how it works and partly from improved microelectronic control. As a result, the physical energy used to break the nucleus down is lower than it was 10 years ago, and surgeons are now able to use higher vacuums and aspiration rates when sucking out the pieces.
Better understanding of some of the factors leading to opacification of the posterior lens capsule that can occur in the years after cataract surgery has reduced its incidence—from a five year incidence of 40-50% expected 10 years ago to about 10% or possibly lower today (though accurate figures are hard to come by). Measures include meticulous removal of all strands of cortex from the equator of the capsule, incorporating a sharp edge to the optic of the intraocular lens implant, and possibly selection of appropriate lens material.
Useful links for patients
Royal College of Ophthalmologists. Understanding cataracts (www.rcophth.ac.uk/docs/publications/UnderstandingCataracts.pdf)
Best Treatments. Cataracts (www.besttreatments.co.uk/btuk/conditions/1000077670.jsp)
Royal National Institute for the Blind. Understanding cataracts (www.rnib.org.uk/xpedio/groups/public/documents/PublicWebsite/public_rnib003640.hcsp)
Eye Surgery Education Council. Cataracts (www.eyesurgeryeducation.com/Cataract_Treatment.html)
National Eye Institute. Cataract: what you should know (www.nei.nih.gov/health/cataract/cataract_facts.asp)
Intraocular lens design has seen two major innovations. Until recently, these lenses had spherical anterior and posterior surfaces. Light passing through more peripheral parts of such spherical lenses is bent more than light passing through more central parts, resulting in reduced image quality (“spherical aberration”). In disciplines such as microscopy, astronomy, and photography the use of aspheric lenses has been standard for decades. Some aspheric intraocular lenses are now available and neither add nor remove any spherical aberration in the eye. Other lenses are designed to nullify the degree of positive spherical aberration that exists in most corneas. Although this improves image contrast in low illumination, there is some evidence that the eye may function better with a small degree of spherical aberration. For example, depth of focus is improved by a degree of spherical aberration, and uncorrected reading vision is poorer in patients with intraocular lenses designed to leave the eye aberration-free.
The other important aspect of new lens design is attempting to provide a spectacle-free full range of vision—distance, intermediate, and near. Bifocal or multifocal intraocular lenses have been in use for 20 years, but the latest versions seem to offer spectacle independence to substantial numbers of patients with much reduced side effects compared with early designs.
Competing interests: The authors have no direct financial links, but they have received reimbursements for travel and accommodation expenses from companies manufacturing intraocular lenses and phacoemulsification machines (Alcon Laboratories, Fort Worth, TX, USA (DA and AV) and Bausch & Lomb, Rochester, NY, USA (DA)).
References
- 1.Thylefors B, Negrel AD, Pararajasegaram R, Dadzie KY. Global data on blindness. Bull World Health Organ 1995;73: 115-21. [PMC free article] [PubMed] [Google Scholar]
- 2.Allen D. Cataract. Clin Evid 2005;(14): 762-7. [PubMed]
- 3.Kelly SP, Thornton J, Edwards R, Sahu A, Harrison R. Smoking and cataract: review of causal association. J Cataract Refract Surg 2005;31: 2395-404. [DOI] [PubMed] [Google Scholar]
- 4.Taylor HR, West SK, Rosenthal FS, Munoz B, Newland HS, Abbey H, et al. Effect of ultraviolet radiation on cataract formation. N Engl J Med 1988;319: 1429-33. [DOI] [PubMed] [Google Scholar]
- 5.Zodpey SP, Ughade SN, Khanolkar VA, Shrikhande SN. Dehydrational crisis from severe diarrhoea and risk of age-related cataract. J Indian Med Assoc 1999;97: 13-5, 24. [PubMed] [Google Scholar]
- 6.Prajna NV, Chandrakanth KS, Kim R, Narendran V, Selvakumar S, Rohini G, et al. The Madurai intraocular lens study. II: clinical outcomes. Am J Ophthalmol 1998;125: 14-25. [DOI] [PubMed] [Google Scholar]
- 7.Snellingen T, Evans JR, Ravilla T, Foster A. Surgical interventions for age related cataract. Cochrane Database Syst Rev 2002;(2):CD001323. [DOI] [PubMed]
- 8.Minassian DC, Rosen P, Dart JK, Reidy A, Desai P, Sidhu M, et al. Extracapsular cataract extraction compared with small incision surgery by phacoemulsification: a randomized trial. Br J Ophthalmol 2001;85: 822-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Osborne SA, Adams WE, Bunce CV, Fraser SG. Validation of two scoring systems for the prediction of posterior capsule rupture during phacoemulsification surgery. Br J Ophthalmol 2006;90: 333-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Asbell PA, Dualan I, Mindel J, Brocks D, Ahmad M, Epstein S. Age-related cataract. Lancet 2005;365: 599-609. [DOI] [PubMed] [Google Scholar]
- 11.Vasavada AR, Raj SM. Cataract treatment where resources are scarce. Lancet 2005;365: 550-1. [DOI] [PubMed] [Google Scholar]
- 12.Foster A. Cataract and “Vision 2020-the right to sight” initiative. Br J Ophthalmol 2001;85: 635-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Barry P, Seal DV, Gettinby G, Lees F, Peterson M, Revie CW. ESCRS study of prophylaxis of postoperative endophthalmitis after cataract surgery: preliminary report of principal results from a European multicenter study. J Cataract Refract Surg 2006;32: 407-10. [DOI] [PubMed] [Google Scholar]
- 14.Ruit S, Paudyal G, Gurung R, Tabin G, Moran D, Brian G. An innovation in developing world cataract surgery: sutureless extracapsular cataract extraction with intraocular lens implantation. Clin Exp Ophthalmol 2000;28: 274-9. [DOI] [PubMed] [Google Scholar]
- 15.Balent LC, Narendrum K, Patel S, Kar S, Patterson DA. High volume sutureless intraocular lens surgery in a rural eye camp in India. Ophthalmic Surg Lasers 2001;32: 446-55. [PubMed] [Google Scholar]
- 16.Ruit S, Tabin GC, Nissman SA, Paudyal G, Gurung R. Low-cost high-volume extracapsular cataract extraction with posterior chamber intraocular lens implantation in Nepal. Ophthalmology 1999;106: 1887-92. [DOI] [PubMed] [Google Scholar]
- 17.Gillies M, Brian G, La Nauze J, Le Mesurier R, Moran D, Taylor H, et al. Modern surgery for global cataract blindness: preliminary considerations. Arch Ophthalmol 1998;116: 90-2. [DOI] [PubMed] [Google Scholar]
- 18.Civerchia L, Ravindran RD, Apoorvananda SW, Ramakrishnan R, Balent A, Spencer MH, et al. High-volume intraocular lens surgery in a rural eye camp in India. Ophthalmic Surg Lasers 1996;27: 200-8. [PubMed] [Google Scholar]
- 19.Royal College of Ophthalmologists. Outcomes and complications. In: Cataract surgery guidelines. London: RCOphth, 2004: 39-44. (www.rcophth.ac.uk/docs/publications/CataractSurgeryGuidelinesMarch2005Updated.pdf)