Abstract
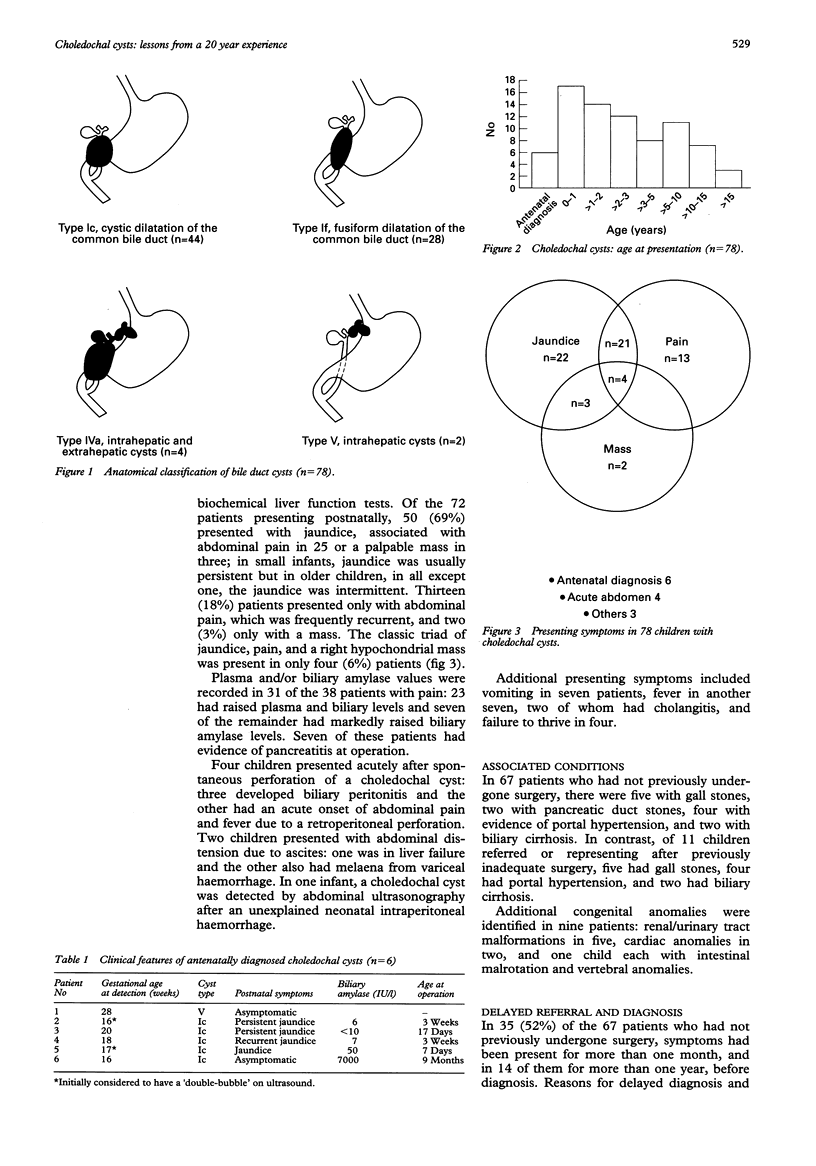
Cystic dilatation of the biliary tree is a rare congenital anomaly. To determine mode of presentation, diagnostic pitfalls, and long term outcome after surgery, 78 children (57 girls, 21 boys) with choledochal cyst treated between 1974 and 1994 were reviewed. Anatomical types were: Ic (n = 44), If (n = 28), IVa (n = 4), and V (n = 2); a common pancreaticobiliary channel was identified in 76% patients. Age at presentation ranged from 0-16 (median 2.2) years, six patients being diagnosed by prenatal ultrasonography. Of the 72 patients diagnosed postnatally, 50 (69%) presented with jaundice, associated with abdominal pain in 25 or a palpable mass in three, 13 (18%) presented with pain alone, and two (3%) with a palpable mass. The classic triad of jaundice, pain, and a right hypochondrial mass was present in only four (6%). Four children presented acutely after spontaneous perforation of a choledochal cyst, two presented with ascites and one cyst was discovered incidentally. Plasma and/or biliary amylase values were raised in 30 of 31 patients investigated for abdominal pain; seven had evidence of pancreatitis at operation. In 35 of 67 (52%) patients referred without previous surgery, symptoms had been present for more than one month, and in 14 of them for more than one year, before diagnosis. Delayed referral was due to misdiagnosis as hepatitis (n = 12), incomplete investigation of abdominal pain (n = 6), and failure to note the significance of ultrasonographic findings (n = 10). Two patients referred late died from liver failure. Of the 76 patients with type I or IV cysts, 59 underwent radical cyst excision and hepaticojejunostomy as a primary procedure and 10 as a secondary operation after previously unsuccessful surgery. Sixteen patients have been lost to follow up but most of the remainder are well after a mean period of 4.1 (0.1-13) years. Choledochal cysts are often misdiagnosed, but prognosis is excellent if radical excision is performed.
Full text
PDF


Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Bancroft J. D., Bucuvalas J. C., Ryckman F. C., Dudgeon D. L., Saunders R. C., Schwarz K. B. Antenatal diagnosis of choledochal cyst. J Pediatr Gastroenterol Nutr. 1994 Feb;18(2):142–145. doi: 10.1097/00005176-199402000-00004. [DOI] [PubMed] [Google Scholar]
- Davenport M., Stringer M. D., Howard E. R. Biliary amylase and congenital choledochal dilatation. J Pediatr Surg. 1995 Mar;30(3):474–477. doi: 10.1016/0022-3468(95)90059-4. [DOI] [PubMed] [Google Scholar]
- Greenholz S. K., Lilly J. R., Shikes R. H., Hall R. J. Biliary atresia in the newborn. J Pediatr Surg. 1986 Dec;21(12):1147–1148. doi: 10.1016/0022-3468(86)90029-1. [DOI] [PubMed] [Google Scholar]
- Harris V. J., Kahler J. Choledochal cyst: Delayed diagnosis in a jaundiced infant. Pediatrics. 1978 Aug;62(2):235–237. [PubMed] [Google Scholar]
- Hernanz-Schulman M., Ambrosino M. M., Freeman P. C., Quinn C. B. Common bile duct in children: sonographic dimensions. Radiology. 1995 Apr;195(1):193–195. doi: 10.1148/radiology.195.1.7892467. [DOI] [PubMed] [Google Scholar]
- Iwai N., Deguchi E., Yanagihara J., Iwai M., Matsuo H., Todo S., Imashuku S. Cancer arising in a choledochal cyst in a 12-year-old girl. J Pediatr Surg. 1990 Dec;25(12):1261–1263. doi: 10.1016/0022-3468(90)90525-e. [DOI] [PubMed] [Google Scholar]
- Joseph V. T. Surgical techniques and long-term results in the treatment of choledochal cyst. J Pediatr Surg. 1990 Jul;25(7):782–787. doi: 10.1016/s0022-3468(05)80019-3. [DOI] [PubMed] [Google Scholar]
- Okada A., Oguchi Y., Kamata S., Ikeda Y., Kawashima Y., Saito R. Common channel syndrome--diagnosis with endoscopic retrograde cholangiopancreatography and surgical management. Surgery. 1983 May;93(5):634–642. [PubMed] [Google Scholar]
- Raffensperger J. G., Given G. Z., Warrner R. A. Fusiform dilatation of the common bile duct with pancreatitis. J Pediatr Surg. 1973 Dec;8(6):907–910. doi: 10.1016/0022-3468(73)90009-2. [DOI] [PubMed] [Google Scholar]
- Schroeder D., Smith L., Prain H. C. Antenatal diagnosis of choledochal cyst at 15 weeks' gestation: etiologic implications and management. J Pediatr Surg. 1989 Sep;24(9):936–938. doi: 10.1016/s0022-3468(89)80600-1. [DOI] [PubMed] [Google Scholar]
- Stringel G., Filler R. M. Fictitious pancreatitis in choledochal cyst. J Pediatr Surg. 1982 Aug;17(4):359–361. doi: 10.1016/s0022-3468(82)80488-0. [DOI] [PubMed] [Google Scholar]
- Tan C. E., Howard E. R., Driver M., Murray-Lyon I. M. Non-communicating multiseptate gall bladder and choledochal cyst: a case report and review of publications. Gut. 1993 Jun;34(6):853–856. doi: 10.1136/gut.34.6.853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tan K. C., Howard E. R. Choledochal cyst: a 14-year surgical experience with 36 patients. Br J Surg. 1988 Sep;75(9):892–895. doi: 10.1002/bjs.1800750921. [DOI] [PubMed] [Google Scholar]
- Todani T., Watanabe Y., Narusue M., Tabuchi K., Okajima K. Congenital bile duct cysts: Classification, operative procedures, and review of thirty-seven cases including cancer arising from choledochal cyst. Am J Surg. 1977 Aug;134(2):263–269. doi: 10.1016/0002-9610(77)90359-2. [DOI] [PubMed] [Google Scholar]
- Wheeler R. A., Colquhoun-Flannery W. A., Johnson C. D. Plasma amylase estimation in recurrent abdominal pain in children. Ann R Coll Surg Engl. 1992 Sep;74(5):335–337. [PMC free article] [PubMed] [Google Scholar]
- Yeong M. L., Nicholson G. I., Lee S. P. Regression of biliary cirrhosis following choledochal cyst drainage. Gastroenterology. 1982 Feb;82(2):332–335. [PubMed] [Google Scholar]


