Abstract
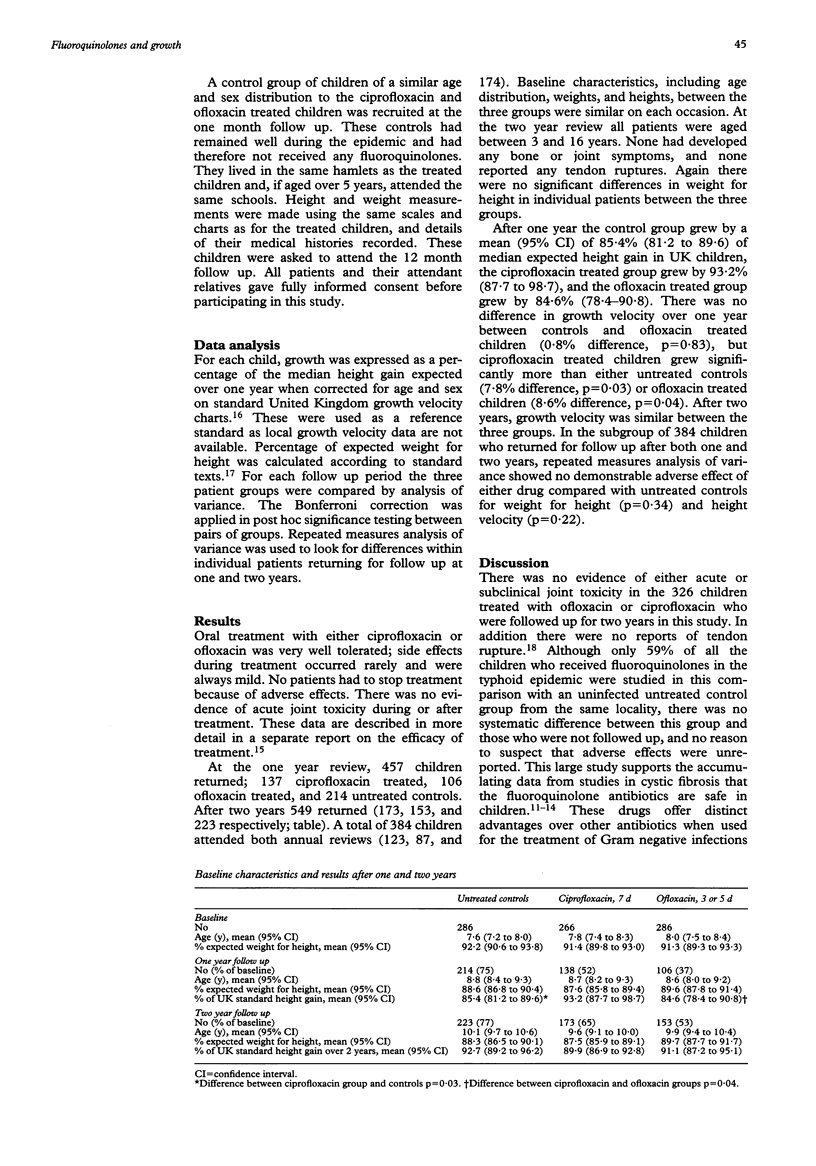
The aim of the study was to document the effects of short courses of fluoroquinolones given during an outbreak of multidrug resistant typhoid fever in southern Viet Nam on the growth of children over a period of two years. In a prospective cohort study, 326 Vietnamese children aged between 1 and 14 years were followed up for two years after receiving either ciprofloxacin (70 mg/kg given over 7 d) (n = 173) or ofloxacin (45-50 mg/kg given over 3-5 d) (n = 153) for suspected typhoid fever. Growth velocity and weight for height were compared with an age matched control group of children from the same locality (n = 223) who had not contracted typhoid or received any fluoroquinolones. In the ofloxacin and ciprofloxacin treated patients there was no evidence of acute joint toxicity, nor of any joint symptoms attributable to either of the fluoroquinolones. There was no difference in expected weight for height measurements between the three groups of children over the two year period. During the first year, height velocity in ciprofloxacin treated children was greater than in either ofloxacin treated children or untreated controls. Height velocity in the latter two groups was not significantly different. After two years height velocity was similar in the three groups. The results support the use of short course fluoroquinolone treatment in childhood typhoid, especially when caused by strains resistant to other antibiotics.
Full text
PDF
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Adam D. Use of quinolones in pediatric patients. Rev Infect Dis. 1989 Jul-Aug;11 (Suppl 5):S1113–S1116. doi: 10.1093/clinids/11.supplement_5.s1113. [DOI] [PubMed] [Google Scholar]
- Burkhardt J. E., Hill M. A., Carlton W. W., Kesterson J. W. Histologic and histochemical changes in articular cartilages of immature beagle dogs dosed with difloxacin, a fluoroquinolone. Vet Pathol. 1990 May;27(3):162–170. doi: 10.1177/030098589002700303. [DOI] [PubMed] [Google Scholar]
- Gough A., Barsoum N. J., Mitchell L., McGuire E. J., de la Iglesia F. A. Juvenile canine drug-induced arthropathy: clinicopathological studies on articular lesions caused by oxolinic and pipemidic acids. Toxicol Appl Pharmacol. 1979 Oct;51(1):177–187. doi: 10.1016/0041-008x(79)90020-6. [DOI] [PubMed] [Google Scholar]
- Heyworth B., Brown J. Jejunal microflora in malnourished Gambian children. Arch Dis Child. 1975 Jan;50(1):27–33. doi: 10.1136/adc.50.1.27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hirschhorn N. Can small daily doses of antibiotics prevent the cycle of diarrhea, malabsorption, and malnutrition in children? Am J Clin Nutr. 1971 Jul;24(7):872–875. doi: 10.1093/ajcn/24.7.872. [DOI] [PubMed] [Google Scholar]
- LeBel M. Fluoroquinolones in the treatment of cystic fibrosis: a critical appraisal. Eur J Clin Microbiol Infect Dis. 1991 Apr;10(4):316–324. doi: 10.1007/BF01967005. [DOI] [PubMed] [Google Scholar]
- Maggiolo F., Caprioli S., Suter F. Risk/benefit analysis of quinolone use in children: the effect on diarthrodial joints. J Antimicrob Chemother. 1990 Oct;26(4):469–471. doi: 10.1093/jac/26.4.469. [DOI] [PubMed] [Google Scholar]
- Mourad A. S., Metwally M., el Deen A. N., Threlfall E. J., Rowe B., Mapes T., Hedstrom R., Bourgeois A. L., Murphy J. R. Multiple-drug-resistant Salmonella typhi. Clin Infect Dis. 1993 Jul;17(1):135–136. doi: 10.1093/clinids/17.1.135. [DOI] [PubMed] [Google Scholar]
- Royer R. J., Pierfitte C., Netter P. Features of tendon disorders with fluoroquinolones. Therapie. 1994 Jan-Feb;49(1):75–76. [PubMed] [Google Scholar]
- Schaad U. B., Stoupis C., Wedgwood J., Tschaeppeler H., Vock P. Clinical, radiologic and magnetic resonance monitoring for skeletal toxicity in pediatric patients with cystic fibrosis receiving a three-month course of ciprofloxacin. Pediatr Infect Dis J. 1991 Oct;10(10):723–729. [PubMed] [Google Scholar]
- Schaad U. B., Wedgwood J. Lack of quinolone-induced arthropathy in children. J Antimicrob Chemother. 1992 Oct;30(4):414–416. doi: 10.1093/jac/30.4.414. [DOI] [PubMed] [Google Scholar]
- Schaad U. B., abdus Salam M., Aujard Y., Dagan R., Green S. D., Peltola H., Rubio T. T., Smith A. L., Adam D. Use of fluoroquinolones in pediatrics: consensus report of an International Society of Chemotherapy commission. Pediatr Infect Dis J. 1995 Jan;14(1):1–9. doi: 10.1097/00006454-199501000-00001. [DOI] [PubMed] [Google Scholar]
- Smith M. D., Duong N. M., Hoa N. T., Wain J., Ha H. D., Diep T. S., Day N. P., Hien T. T., White N. J. Comparison of ofloxacin and ceftriaxone for short-course treatment of enteric fever. Antimicrob Agents Chemother. 1994 Aug;38(8):1716–1720. doi: 10.1128/aac.38.8.1716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spread of multiresistant Salmonella typhi. Lancet. 1990 Oct 27;336(8722):1065–1066. [PubMed] [Google Scholar]
- Stahlmann R., Merker H. J., Hinz N., Chahoud I., Webb J., Heger W., Neubert D. Ofloxacin in juvenile non-human primates and rats. Arthropathia and drug plasma concentrations. Arch Toxicol. 1990;64(3):193–204. doi: 10.1007/BF02010725. [DOI] [PubMed] [Google Scholar]
- Tanner J. M., Whitehouse R. H. Clinical longitudinal standards for height, weight, height velocity, weight velocity, and stages of puberty. Arch Dis Child. 1976 Mar;51(3):170–179. doi: 10.1136/adc.51.3.170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tran T. H., Bethell D. B., Nguyen T. T., Wain J., To S. D., Le T. P., Bui M. C., Nguyen M. D., Pham T. T., Walsh A. L. Short course of ofloxacin for treatment of multidrug-resistant typhoid. Clin Infect Dis. 1995 Apr;20(4):917–923. [PubMed] [Google Scholar]
- Tran T. H., Nguyen M. D., Huynh D. H., Nguyen T. T., To S. D., Le T. P., Arnold K. A randomized comparative study of fleroxacin and ceftriaxone in enteric fever. Trans R Soc Trop Med Hyg. 1994 Jul-Aug;88(4):464–465. doi: 10.1016/0035-9203(94)90435-9. [DOI] [PubMed] [Google Scholar]
- Uwaydah A. K., Matar I., Chacko K. C., Davidson J. C. The emergence of antimicrobial resistant Salmonella typhi in Qatar: epidemiology and therapeutic implications. Trans R Soc Trop Med Hyg. 1991 Nov-Dec;85(6):790–792. doi: 10.1016/0035-9203(91)90457-a. [DOI] [PubMed] [Google Scholar]


