Abstract
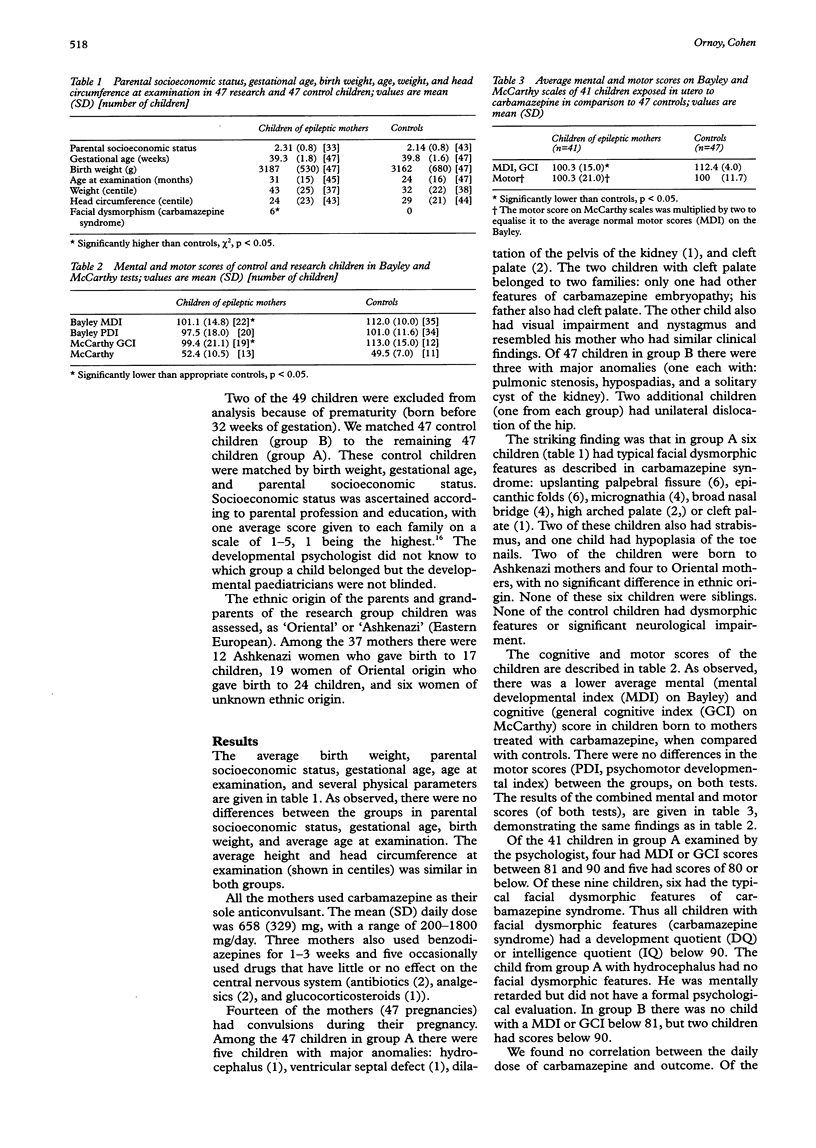
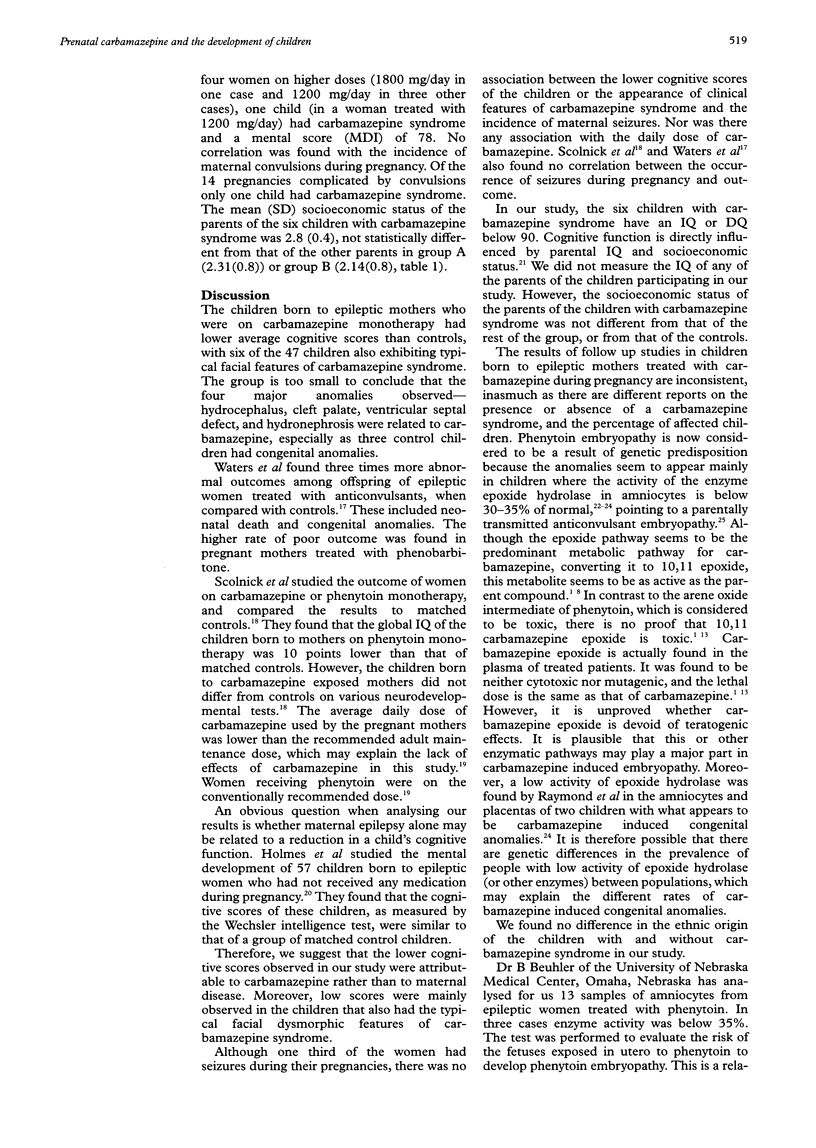
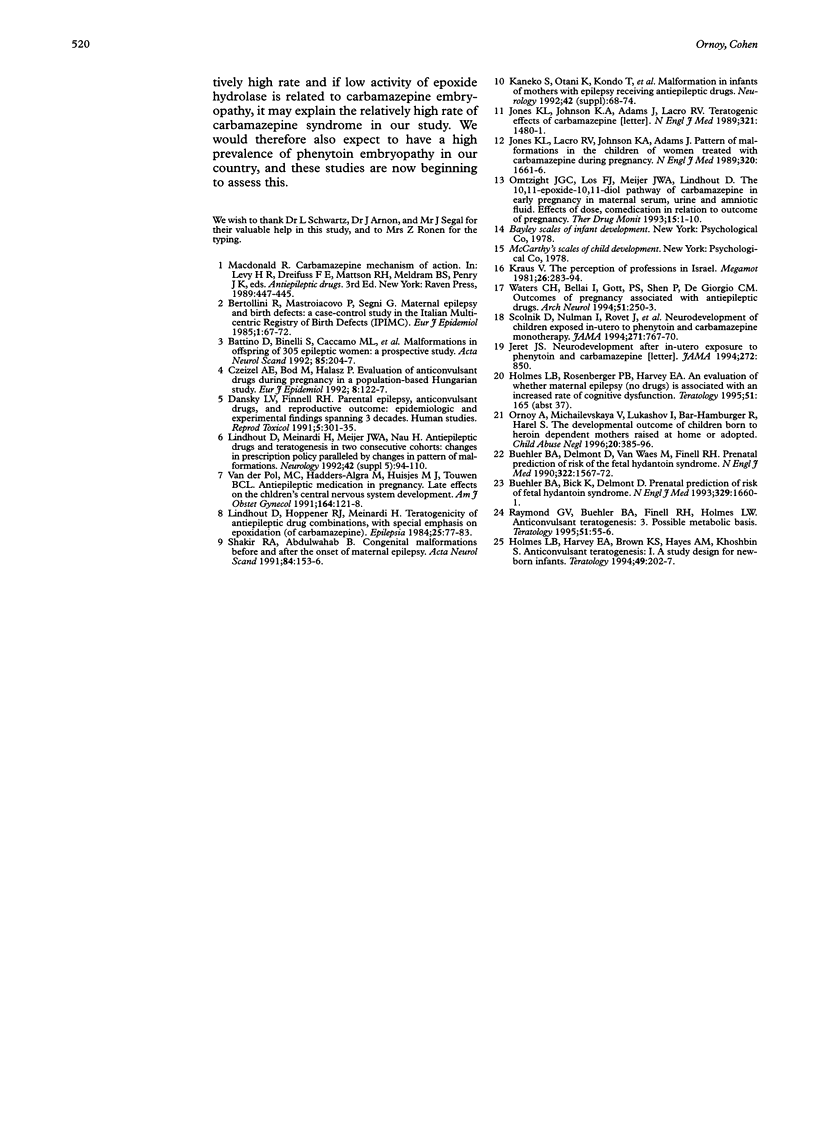
AIM: The purpose of the study was to assess whether there was an increased rate of congenital anomalies or significant developmental delay in infants of women with epilepsy who had been treated with carbamazepine during pregnancy. METHODS: 47 children were studied, aged 6 months-6 years, who were born to 37 epileptic mothers on carbamazepine monotherapy (group A). All children had a complete physical and neurodevelopmental assessment by a developmental paediatrician, and 41 a complete psychological evaluation. They were compared with 47 children of similar socioeconomic status (group B). RESULTS: Six of the 47 children in group A had typical facial features of 'carbamazepine syndrome'. The average cognitive score of children in group A was significantly lower than in group B. This was mainly because all six children with carbamazepine syndrome had a development quotient or intelligence quotient below 90. There were no differences between the two groups in physical growth or in the rate of major anomalies. Two children in group A had cleft palate but in each case this was found in a parent as well. CONCLUSIONS: In utero exposure to carbamazepine may result in 'carbamazepine syndrome' characterised by facial dysmorphic features and mild mental retardation. Prevalence of carbamazepine syndrome does not seem to be related to the dose of carbamazepine or the presence of maternal convulsions. It may depend upon heredofamilial factors that have yet to be defined. One possible factor is decreased activity of the enzyme epoxide hydrolase with resulting increased concentrations of carbamazepine epoxide which may be teratogenic.
Full text
PDF
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Battino D., Binelli S., Caccamo M. L., Canevini M. P., Canger R., Como M. L., Croci D., De Giambattista M., Granata T., Pardi G. Malformations in offspring of 305 epileptic women: a prospective study. Acta Neurol Scand. 1992 Mar;85(3):204–207. doi: 10.1111/j.1600-0404.1992.tb04029.x. [DOI] [PubMed] [Google Scholar]
- Bertollini R., Mastroiacovo P., Segni G. Maternal epilepsy and birth defects: a case-control study in the Italian Multicentric Registry of Birth Defects (IPIMC). Eur J Epidemiol. 1985 Mar;1(1):67–72. doi: 10.1007/BF00162315. [DOI] [PubMed] [Google Scholar]
- Buehler B. A., Bick D., Delimont D. Prenatal prediction of risk of the fetal hydantoin syndrome. N Engl J Med. 1993 Nov 25;329(22):1660–1661. doi: 10.1056/NEJM199311253292219. [DOI] [PubMed] [Google Scholar]
- Buehler B. A., Delimont D., van Waes M., Finnell R. H. Prenatal prediction of risk of the fetal hydantoin syndrome. N Engl J Med. 1990 May 31;322(22):1567–1572. doi: 10.1056/NEJM199005313222204. [DOI] [PubMed] [Google Scholar]
- Czeizel A. E., Bod M., Halász P. Evaluation of anticonvulsant drugs during pregnancy in a population-based Hungarian study. Eur J Epidemiol. 1992 Jan;8(1):122–127. doi: 10.1007/BF03334986. [DOI] [PubMed] [Google Scholar]
- Dansky L. V., Finnell R. H. Parental epilepsy, anticonvulsant drugs, and reproductive outcome: epidemiologic and experimental findings spanning three decades; 2: Human studies. Reprod Toxicol. 1991;5(4):301–335. doi: 10.1016/0890-6238(91)90091-s. [DOI] [PubMed] [Google Scholar]
- Holmes L. B., Harvey E. A., Brown K. S., Hayes A. M., Khoshbin S. Anticonvulsant teratogenesis: I. A study design for newborn infants. Teratology. 1994 Mar;49(3):202–207. doi: 10.1002/tera.1420490316. [DOI] [PubMed] [Google Scholar]
- Jeret J. S. Neurodevelopment after in utero exposure to phenytoin and carbamazepine. JAMA. 1994 Sep 21;272(11):850–851. doi: 10.1001/jama.272.11.850b. [DOI] [PubMed] [Google Scholar]
- Jones K. L., Lacro R. V., Johnson K. A., Adams J. Pattern of malformations in the children of women treated with carbamazepine during pregnancy. N Engl J Med. 1989 Jun 22;320(25):1661–1666. doi: 10.1056/NEJM198906223202505. [DOI] [PubMed] [Google Scholar]
- Kaneko S., Otani K., Kondo T., Fukushima Y., Nakamura Y., Ogawa Y., Kan R., Takeda A., Nakane Y., Teranishi T. Malformation in infants of mothers with epilepsy receiving antiepileptic drugs. Neurology. 1992 Apr;42(4 Suppl 5):68–74. [PubMed] [Google Scholar]
- Lindhout D., Höppener R. J., Meinardi H. Teratogenicity of antiepileptic drug combinations with special emphasis on epoxidation (of carbamazepine). Epilepsia. 1984 Feb;25(1):77–83. doi: 10.1111/j.1528-1157.1984.tb04158.x. [DOI] [PubMed] [Google Scholar]
- Lindhout D., Meinardi H., Meijer J. W., Nau H. Antiepileptic drugs and teratogenesis in two consecutive cohorts: changes in prescription policy paralleled by changes in pattern of malformations. Neurology. 1992 Apr;42(4 Suppl 5):94–110. [PubMed] [Google Scholar]
- Omtzigt J. G., Los F. J., Meijer J. W., Lindhout D. The 10,11-epoxide-10,11-diol pathway of carbamazepine in early pregnancy in maternal serum, urine, and amniotic fluid: effect of dose, comedication, and relation to outcome of pregnancy. Ther Drug Monit. 1993 Feb;15(1):1–10. doi: 10.1097/00007691-199302000-00001. [DOI] [PubMed] [Google Scholar]
- Ornoy A., Michailevskaya V., Lukashov I., Bar-Hamburger R., Harel S. The developmental outcome of children born to heroin-dependent mothers, raised at home or adopted. Child Abuse Negl. 1996 May;20(5):385–396. doi: 10.1016/0145-2134(96)00014-2. [DOI] [PubMed] [Google Scholar]
- Raymond G. V., Buehler B. A., Finnell R. H., Holmes L. B. Anticonvulsant teratogenesis: 3. Possible metabolic basis. Teratology. 1995 Feb;51(2):55–56. doi: 10.1002/tera.1420510202. [DOI] [PubMed] [Google Scholar]
- Scolnik D., Nulman I., Rovet J., Gladstone D., Czuchta D., Gardner H. A., Gladstone R., Ashby P., Weksberg R., Einarson T. Neurodevelopment of children exposed in utero to phenytoin and carbamazepine monotherapy. JAMA. 1994 Mar 9;271(10):767–770. [PubMed] [Google Scholar]
- Shakir R. A., Abdulwahab B. Congenital malformations before and after the onset of maternal epilepsy. Acta Neurol Scand. 1991 Aug;84(2):153–156. doi: 10.1111/j.1600-0404.1991.tb04924.x. [DOI] [PubMed] [Google Scholar]
- Teratogenic effects of carbamazepine. N Engl J Med. 1989 Nov 23;321(21):1480–1481. doi: 10.1056/NEJM198911233212116. [DOI] [PubMed] [Google Scholar]
- Waters C. H., Belai Y., Gott P. S., Shen P., De Giorgio C. M. Outcomes of pregnancy associated with antiepileptic drugs. Arch Neurol. 1994 Mar;51(3):250–253. doi: 10.1001/archneur.1994.00540150044014. [DOI] [PubMed] [Google Scholar]
- van der Pol M. C., Hadders-Algra M., Huisjes H. J., Touwen B. C. Antiepileptic medication in pregnancy: late effects on the children's central nervous system development. Am J Obstet Gynecol. 1991 Jan;164(1 Pt 1):121–128. doi: 10.1016/0002-9378(91)90640-d. [DOI] [PubMed] [Google Scholar]


