Abstract
The authors describe a pragmatic approach to the introduction of clinical decision support at the point of care, based on a decade of experience in developing and evolving Vanderbilt’s inpatient “WizOrder” care provider order entry (CPOE) system. The inpatient care setting provides a unique opportunity to interject CPOE-based decision support features that restructure clinical workflows, deliver focused relevant educational materials, and influence how care is delivered to patients. From their empirical observations, the authors have developed a generic model for decision support within inpatient CPOE systems. They believe that the model’s utility extends beyond Vanderbilt, because it is based on characteristics of end-user workflows and on decision support considerations that are common to a variety of inpatient settings and CPOE systems. The specific approach to implementing a given clinical decision support feature within a CPOE system should involve evaluation along three axes: what type of intervention to create (for which the authors describe 4 general categories); when to introduce the intervention into the user’s workflow (for which the authors present 7 categories), and how disruptive, during use of the system, the intervention might be to end-users’ workflows (for which the authors describe 6 categories). Framing decision support in this manner may help both developers and clinical end-users plan future alterations to their systems when needs for new decision support features arise.
Keywords: CPOE, Clinical decision support
1. Introduction
The need for decision support systems in medicine has been understood for 2500 years: Hippocrates noted “Life is short, the art long, opportunity fleeting, experience treacherous, judgment difficult.” (Aphorisms, sec. I, ca. 460–400 BC). While the basis for clinical decision support has been recognized throughout the ages, careful studies in the recent medical literature document those needs specifically [1–14]. Early pioneers, such as McDonald, Tierney, and their colleagues at the Regenstrief Medical Institute [15–25; Warner, Gardner and their colleagues at LDS Hospital [26–38]; and many other groups have confirmed, through controlled studies, the initial report of Shakespeare in 1597: “If to do were as easy as to know what were good to do, chapels had been churches, and poor men’s cottages princes’ palaces. … I can easier teach twenty what were good to be done than to be one of the twenty to follow my own teaching.” (The Merchant of Venice, Act I, Scene ii). Busy clinicians have so many diverse tasks to perform that they are constantly distracted from being able to accomplish what is known to them as good medical practice. “Men are men; the best sometimes forget.” (Shakespeare, Othello, 1605; Act II, Scene iii). Reminding systems and other forms of clinical decision support have been shown to be effective in overcoming such lapses of memory in a number of clinical situations [15–40]. However, the success of systems intended to be used by busy practitioners is not guaranteed. A significant number of clinical informatics systems (not all documented in the literature) implemented with good intentions have been met with anger and resentment [41–44]. Providing decision support capabilities in a timely and convenient manner can add value to otherwise lackluster or marginal systems, and improve quality of care and reduce costs [15–40].
This article addresses the following questions: (1) “What steps or stages in care provider order entry represent appropriate “breakpoints” (both computationally and with respect to end-user workflows) at which one can introduce clinical decision support?” (2) “What categories of decision support are relevant during care provider order entry (CPOE) sessions?” and, (3) “What methods for workflow interruption should one consider to implement decision support interventions based on end-user tolerance and clinical urgency?”
The authors use the Vanderbilt WizOrder CPOE system as the primary context for discussing decision support interventions. Through longstanding partnerships with clinician end-users, Vanderbilt Biomedical Informatics faculty members, fellows and staff developed a CPOE system (“WizOrder”), implemented it on the wards of an academic teaching hospital, and evolved it in response to ongoing feedback [45–55]. The approach to decision support described in this manuscript was derived through generalization from experience. The authors describe the pre-commercialization version of WizOrder at Vanderbilt. The Acknowledgements section discloses the authors’ non-conflict of interests regarding commercialization. While the authors draw heavily on their Vanderbilt experience, the above questions and their answers are generic enough that others may find value from the descriptions provided herein.
2. Basic CPOE system functionality
Order entry within most CPOE systems parallels manual paper chart-based order creation. Manual ordering involves: (1) finding the patient’s chart; (2) finding the topmost “blank” order page; (3) handwriting new orders as a block; (4) signing the orders to make them “legal”; (5) after setting a flag indicating presence of new orders, placing the chart where clerical unit staff expect to find charts with new orders; and, (6) informing unit staff (patient’s nurse, others) when life-critical or extremely urgent orders have been written. For the corresponding electronic CPOE processes, the user: (1) authenticates with user name and password; (2) invokes the CPOE application and selects a patient for order entry; (3) enters and modifies orders, using an electronic “scratchpad” (buffer) that holds orders but does not deliver them to ancillary departments (e.g., lab or pharmacy) for immediate action; (4) indicates when he or she is ready to “finalize” the set of orders on the “scratchpad” to send them out for processing; and, (5) reviews and edits orders on the scratchpad before they are dispatched to be carried out. With electronic CPOE, person-to-person manual communication of life critical or otherwise very urgent orders remains essential for patient safety.
The panes of Fig. 1 represent one (Vanderbilt) approach to implementing key components of an order entry interface. Vanderbilt end users strongly recommended that the CPOE system interface should have “geographical consistency”—meaning that the same types of clinical information always displayed in the same areas of the screen, and limited pop-up windows and pull-down menus that could obscure display of clinically important information. Wiz-Order’s left-sided window displays currently active (or expired in the previous 24 h) orders for the “current CPOE patient” (Fig. 1, pane #1). The upper right window presents context-dependent “pick lists” of options available for order creation or modification (Fig. 1, pane #2). The middle right window represents a context-sensitive help window that instructs the user on available next actions (Fig. 1, pane #3). The bottom right window contains a text input region (Fig. 1, panel #4).
Fig. 1.
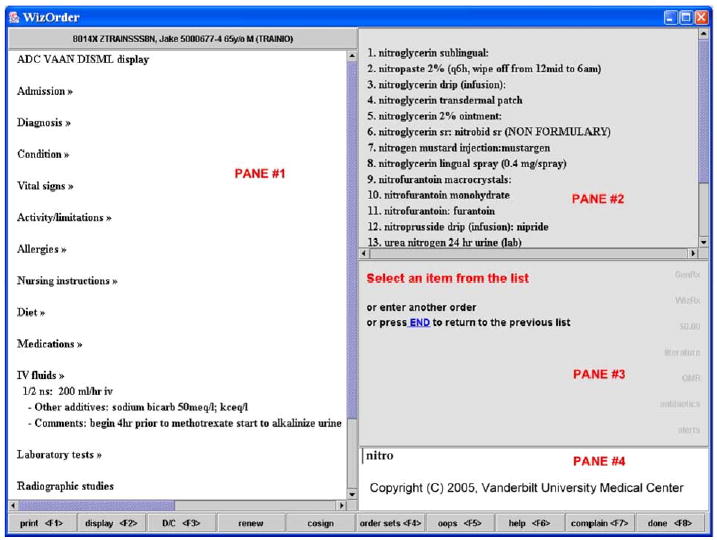
WizOrder primary user interface screen panes: #1, current and recent orders display; #2, selectable “pick list” display; #3, in-context instructions; #4, user input text entry area. User had previously typed “nitro” into completer in pane #4; pane #2 shows results.
2.1. Creating orders
A key CPOE system design consideration involves how clinicians specify what they want to order. Many systems [56–59] utilize a hierarchical organization of orders, illustrated by the following example (bold font indicates hypothetical selection made at each level):
Orderable Pick List Level 1: Pharmacy, Laboratory, Radiology, Dietary, Nursing [orders] …
Orderable Pick List Level 2: Hematology Tests, Serum Chemistry Tests, Urinalysis, …
Orderable Pick List Level 3: Complete blood count (CBC), platelet count, blood Rh type, …
Many systems also have a “completer” function that allows the clinician-user to type “shorthand” word fragments, derived from the desired order name (or its synonyms). The completer then searches for potentially matching terms from the orderables dictionary, and provides the user with a “pick list” of order names, from which the user can select. For example, typing “nitro” into an orders completer (Fig. 1, pane #4) would return a pick list (shown in Fig. 1, pane #2) of orderable items’ names, with “nitroglycerin sublingual” at or near the top of the list, and lesser/partial/wordier matches (e.g., nitrogen mustard, urea nitrogen blood) farther down the list. Vanderbilt users typically specify new orders using the completer function and only rarely use WizOrder’s hierarchies for order entry—usually when they do not know the specific name for the item they want to order.
After selecting an order name, users must specify (enter) an individual order’s components (e.g., dose, route, frequency, etc., for a medication order). Many CPOE systems formally define orderables and their components—using a data dictionary with structured templates that specify necessary and optional “fields” required to fully create an individual order. Fig. 2 illustrates WizOrder sequential prompts for building an order for sublingual nitroglycerin (based on stored templates), and Fig. 3 indicates how the order, once fully specified for WizOrder, transfers to the left-sided “active orders” area (Fig. 3, pane #1 as previously described). Another mechanism for generating new orders (used often, but less than half the time at Vanderbilt) is order sets—groupings of diagnosis or procedure-related selectable orders [60]. If the user selects an order set name from a completer pick list or from the WizOrder order set hierarchy, the order set’s component orders are retrieved and displayed as selectable items in the upper right “pick list” window (Fig. 4, pane #2).
Fig. 2.
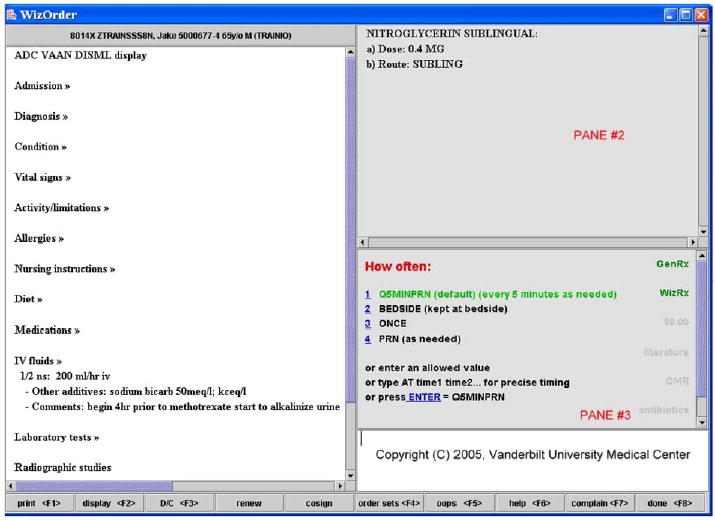
Frequency prompts (medication-specific) for “nitroglycerin sublingual” orderable, after dose already specified by similar process.
Fig. 3.
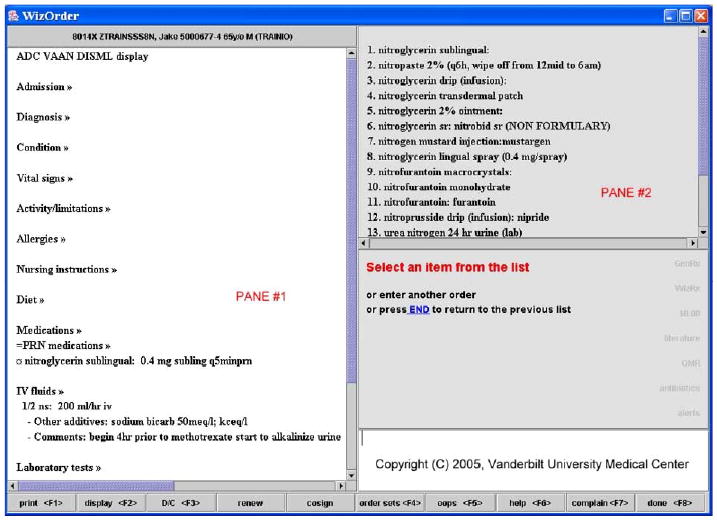
Order for “nitroglycerin” moves to left window (pane #1) once fully completed.
Fig. 4.
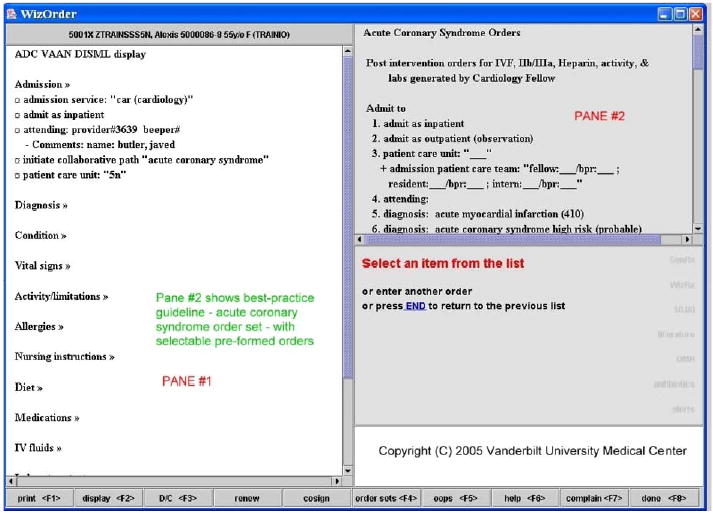
First six orders in the acute coronary syndrome orderset.
2.2. Displaying active orders
Most CPOE user interfaces manage the display of currently active orders. In complex patient cases, the number of active orders may exceed 100. Therefore, simply listing all such orders in a display panel (sorted alphabetically by order name) will not be helpful to clinicians unfamiliar with the patient’s case, since locating an arbitrarily named specific order within a long list is difficult. Early in the development of WizOrder, end-users requested that display of active orders follow a grouping based on the ADC VAAN DISML acronym (familiar to physicians)—Admission, Diagnosis, Condition, Vital signs, Activity, Allergies, and so on (Fig. 1, pane #1). Most CPOE systems use similar methods to segment the active orders display into clinically useful “buckets.” Many CPOE systems facilitate electronic re-arrangements of the active orders display to accommodate different users’ workflows (e.g., nurses, attending physicians). Vanderbilt’s specialized Intensive Care Units and the Emergency Department, for example, required location-specific specialized views of active orders. As WizOrder displays active orders, it also displays recently expired orders (within the past 24 h)—with a special symbol in the left margin to indicate that those orders that have expired; a different left-margin symbol indicates orders soon to expire.
2.3. Modifying and finalizing orders
On-line Fig. 5 (available via online data supplement at JBI web site) illustrates the result of a “mouse click” on an order in the left WizOrder pane. WizOrder displays a series of options listing what the user can do to the order at that point (modify, discontinue, renew, etc.) After the WizOrder user is finished entering orders for a session, clicking a designated button on the CPOE screen transfers the user to a “final accept” screen (see on-line Fig. 6). This screen gives users a last chance to verify (or to change) their orders from the current ordering session. Once “final accepted” the orders are sent to the appropriate ancillary systems for action, and committed to a relational database for archival. Similar features are available in most CPOE systems.
2.4. Displaying information and supporting complex decision support
A final WizOrder component consists of an intermittently displayed, pop-up window that contains an internal HTML browser (labeled “pane #5” in various Figures). The WizOrder program uses this capability to display static web documents with educational content, or dynamically generated CPOE-related pages that provide complex, patient-specific decision support capabilities [49,50].
3. Philosophy underlying decision support during CPOE
Use of a CPOE system during patient care provides a unique opportunity to interject decision support features that improve clinical workflows, provide focused relevant educational materials, and influence how care is delivered to patients. It is somewhat of an art to be able to provide clinical decision support that is well accepted and used widely. Key considerations in the approach to provide decision support include: what content to provide (see below, Section 4); when to intervene in the clinical work-flow process (see below, Section 5); and, how to intervene, in terms of both degree of disruption of workflows and mechanism of interruption (see below, Section 6).
The nature of the clinical application domain determines what types of decision support content to provide. It is not appropriate to allow a clinician to spend 1–2 min constructing an intricate medication order only to later inform the clinician that the medication is contra-indicated due to a previously documented patient allergy. Allergy warnings should take place at the time the clinician first indicates the name of a new medication to be prescribed. Conversely, delivering a warning to a clinician to order a partial thromboplastin time (PTT) monitoring test—immediately as the clinician completes a heparin order—may cause both exasperation and a lost sense of autonomy when that is exactly what the clinician intends to order next. Checking whether a PTT monitoring test has been ordered at the end of an order entry session during which intravenous heparin therapy was initiated may be more appropriate, since the user is “done” entering orders at that stage. Oppenheim et al. [61] observed that permitting the physician to enter an order with feedback provided only at the conclusion of order construction, and then only if the order is possibly incorrect, serves dual purposes. First, delayed warnings make clinicians first commit to a preferred course of action, thus discouraging reliance on CPOE systems to make clinical decision for the users. Second, delayed warnings give the clinician-user the opportunity to correct problems they detect spontaneously, whereas early warnings may impart negative reinforcement by underscoring clinicians’ errors.
In the authors’ experience, busy clinical users value CPOE system responsiveness and intuitiveness. A key aspect of responsiveness involves creating orders at an appropriate clinical level (both for users’ levels of training and for their knowledge of their patients). The physicians and nurses entering orders into a CPOE system typically have a different mindset than individuals who will carry out the orders in ancillary areas (e.g., Pharmacy, Radiology, and Dietary Departments). Problems in creating CPOE system “orderable item” names can occur when the technical terms used in ancillary departments are carried forward as the orderable items vocabulary for clinicians. So while radiology technicians might think in terms of “chest X-ray 2 views” and “knee X-ray 3 views,” clinicians are more comfortable ordering “chest X-ray PA and lateral,” and “knee X-ray AP, lateral and oblique.” Similarly, if the CPOE system asks the physician ordering a chest X-ray how the patient should be transported to the Radiology Department, the physician is unlikely to give an optimal response because physicians are rarely involved in determining a patient’s transport. Thus, CPOE systems should not ask clinicians to perform tasks that fall outside of their job responsibilities, or about which they have little knowledge. Structuring orderable items with the clinician in mind helps to overcome major barriers to adoption.
“Intelligent middleware” system interfaces can dramatically decrease the burden of ancillary departments in dealing with CPOE-system-generated orders. For example, pharmacists use the pharmacy system to fill and dispense the “clinical orderables” specified within the CPOE system; if a high-level order is issued by the physician, it may require more work on the pharmacy system side of the interface to specify all components of an order correctly. Once the physician specifies a medication order at a clinical level, an “intelligent interface” within the CPOE system can evaluate both the pharmacy’s formulary and the floor stock inventory on patient’s unit, and then automatically determine the correct “dispensable” within the pharmacy system. Currently, the “intelligent pharmacy interface” within WizOrder “guesses” the correct pharmacy-level dispensable item over 90% of the time. This allows the pharmacist to devote more time to evaluating each order’s clinical validity, safety, and efficacy.
As a frequently used clinician data entry tool, an institution’s CPOE system becomes a target for administrators and researchers wishing to capture additional data “at the point of care.” It is important to avoid overburdening clinicians with requests that interrupt their workflows, and when extra information is required, the system should only ask clinicians for information about which they are the definitive source. For example, at Vanderbilt, upon patient admission, the attending physician of record was originally input into the ADT system by an admitting clerk. However, the admitting clerks were not always informed of the specifics of physician group coverage schedules, and often did not know the correct name to enter. The problem was addressed by finding a more definitive data source—the admitting house staff team, who must discuss each admission with the attending physician—and having them enter the name into the CPOE system. Conversely, if one wants to record whether a patient received aspirin in the Emergency Department just prior to admission, asking an intern who is entering discharge orders for the patient several days later (and who did not admit the patient) could be viewed as a nuisance, and cause lower-than-optimal data quality.
While some decision support functions not directly related to order entry can be delivered during an order entry session, they will not be discussed in this article. For example, a laboratory system that generates alerts whenever abnormal patient results occur might notify clinicians responsible for the patient’s care by paging them, via e-mail, or via an asynchronous “pop-up” alarm that occurs when the clinician is currently “logged into” the CPOE application [62]. Such alerts originate outside of the CPOE session context. Many CPOE systems, including WizOrder, display permanent “taskbars,” an array of useful links, continuously during the application session [45,59,63–65]; however, such taskbars rarely provide context-specific decision support of the sort described here—they instead allow the user to access common CPOE functions. For instance, the BICS (Brigham Integrated Computer System, in Boston) toolbar allows the clinician to quickly view orders and search for patients, among other functions [64,66].
4. Four roles for decision support within CPOE—categories of interventions
4.1. Creating legible, complete, correct, rapidly actionable orders
A CPOE system can avert problems associated with handwritten order creation [67]: illegibility, incompleteness, and incorrectness. Improved legibility not only reduces errors, but also saves staff time because nurses, pharmacists, and medical technicians spend time and energy as they decipher the meaning of ambiguous handwritten orders, and then make phone calls to clarify what was meant. “Complete” orders contain all the necessary parameters to make an order actionable (order name, start date and time, duration, frequency, etc.). “Correct” orders have parameter values that meet requirements for safe, prudent patient care (e.g., drug doses are appropriate for the patient’s age, weight, and renal function). Most CPOE system interfaces ensure completeness, and promote correctness of orders [67–69].
4.2. Providing patient-specific clinical decision support
An important CPOE system capability is generation of decision support recommendations customized to individual patients’ specific conditions. A CPOE system can provide a safety net through “behind the scenes” reconciliation of patient-specific information (laboratory results, age, allergies, existing medications from the clinical data repository [70]) with stored “best practice” rules. For example, most CPOE systems screen patient orders against dosing rules and drug interaction references to reduce medication prescribing errors [53,66,71–74]. A CPOE system can also facilitate clinical care improvement by promoting use of evidence-based clinical practice guidelines [58,75,76] through end-user order generation via diagnosis or procedure specific order sets [56,59,65,70,76] or via computer-based advisors [58,64,73,77,78], as detailed below.
4.3. Optimizing clinical care (improved workflow, more cost-effective, and regulatory compliant)
Often, complex software systems functionally become high-level programming languages for their end-users. Once clinicians regularly use a CPOE system, they begin to make suggestions about modifying it to make their work easier and more effective. For example, to improve work-flows, several surgical services at Vanderbilt encouraged WizOrder developers to create “registry” orders. The orders place patients on a registry that allows clinicians to track, via a census, diagnoses, and procedures performed on registry patients (e.g., neurosurgery service). At the same time, registries enabled efficient transfer of appropriate information to the billing office, relieving physicians of that responsibility. Early CPOE users at Vanderbilt requested printed rounding reports to facilitate patient care during work rounds and attending (teaching) rounds. The rounding reports concisely summarize, on the front and back of an 8.5 × 11 inch piece of paper, both the patient’s active orders and all laboratory results reported in the prior 72 h with “highlight” markers next to significant (e.g., abnormal) results. After several years, the institution’s administration began to view the CPOE system as a tool to implement quality of care, cost containment, and compliance initiatives [52–54]. Institution-wide CPOE interventions can discourage the ordering of inappropriate, recurring tests [20,52,79]; advise against costly tests or require further justification before allowing them to proceed [22,55,80]; display formulary information [55,57]; and, help the ordering clinician to enter requisite third-party payer compliance codes (e.g., ICD-9 or CPT) for diagnostic tests. Clinicians are not always familiar with compliance rules, and tend to write reasons for tests based on suspected diagnoses (e.g., “rule out MI” for an electrocardiogram, or “possible pneumonia” for a chest X-ray) rather than indications for testing approved by third party payers. Orders that require specific reasons for compliance can be made to trigger the WizOrder internal web browser to display and capture order-specific compliance-related reasons for testing. This can increase the rate of third-party payer reimbursements for those tests due to more accurate, complete capture of compliant reasons.
Clinical decision support features within CPOE systems can also promote implementation and enforcement of local hospital policies. The Regenstrief Medical Record System, a CPOE system developed by McDonald and colleagues at Indiana University, successfully used computer reminders to increase discussion about, and completion of, advanced directives (end-of-life, “do not resuscitate” related orders) [81]. Previous studies had indicated that too few patients completed advance directives [82]. In Boston, the BICS was modified in order to prevent the appearance of vancomycin-resistant microorganisms by requiring clinicians ordering vancomycin to enter a reason for using the antibiotic [83].
The challenge for CPOE system developers is to honor the care improvement goals while keeping the system responsive and intuitive. Developers must strike a proper balance between clinical improvements versus cost containment. At times both goals may be achieved in a single intervention—judiciously ordering fewer tests does not mandate a lower quality of care [52]. However, care improvement interventions may themselves have unintended consequences that require continuous monitoring and feedback to optimize [54].
4.4. Providing just-in-time, focused education relevant to patient care
Most CPOE systems provide relevant educational prompts, and in addition, links to more detailed educational information resources. Educational prompts can be introduced as in-line summaries that appear while prescribing a medication. Fig. 7 shows in the upper right WizOrder panel in-line suggestions for vancomycin dosing adjustments in neonates with meningitis or with renal impairment. The CPOE web browser content can also provide effective educational information—for example, presenting a summary of disease-specific national guidelines, links to educational monographs, or a summary of indications and contra-indications for a specific therapy. Educational links can assist clinician-users to perform complex ordering, such as for total parenteral nutrition in a neonatal intensive care unit. The design of a CPOE system user interface can significantly influence the rate with which users follow educational links and read the related materials [55].
Fig. 7.
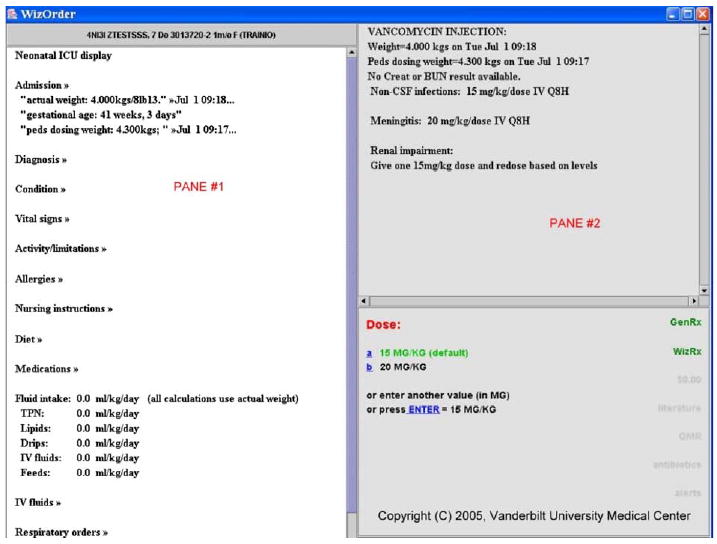
In-line recommendations for dosing vancomycin in neonatal intensive care unit (NICU) include: (A) pane #2, suggested doses for regular use, for meningitis, and for renal impairment; (B) pane #1, passive display of weight, dosing weight, and gestational age; and (C) pane #2, display of renal function test results (not available for training patient in this example).
5. Six critical points at which to implement decision support within CPOE
Each stage of use of a CPOE system permits a focused repertoire of decision support interventions, both in terms of user community affected, patients affected, and appropriateness of the intervention for the task the end-user is performing. For example, as the CPOE system is launched from a clinical workstation desktop, systemwide messages can appear, but patient-specific advice cannot (since typically a patient has not yet been selected).
5.1. Stage of CPOE session initiation
Upon initial launching the CPOE application, the identity of the clinician-user is known, but not the identity of the patient. At this stage, users may be advised of new CPOE system features on a one-time-only basis. To avoid annoying users, such interventions should be used sparingly—for features of general interest to all users, such as a new method of entering a specific group of commonly used orders that replaces the previous method of doing so. Once the alert is displayed, the system removes the current user from the list of users who still need to see that message again. At launch, the CPOE system can also inform users of information related to their personal use of the system, such as the number of orders (and number of patients) requiring their counter-signature, and provide a link to facilitate completing the task.
5.2. Stage of selecting CPOE patient from hospital ward census
After CPOE system launch, users typically select an individual patient for order entry. A number of alerts can occur at the stage of displaying the census of available patients for CPOE. Similar to the BICS system in Boston (and other CPOE systems), WizOrder provides, via the patient census screen, an inpatient-unit-wide view of the status of recently issued orders (see Fig. 8). A “map” view of the given hospital ward shows all beds and indicates which beds have new unacknowledged, “stat” (red) orders and which have unacknowledged “routine” orders. A care provider wishing to enter new orders (or acknowledge recent orders) can click on a bed on the display screen to initiate an order entry session for that particular patient. An alternative to the “map” view of a hospital unit census is a “list” view that lists patients on the unit that can be sorted by patient name or by ascending bed number. In WizOrder, icons located beside patients’ names in the “list” view provide useful information (Fig. 9). Using a similar “list” census screen, the BICS system presents a renewal reminder next to the patient’s name when a medication order for a given patient nears expiration [84].
Fig. 8.
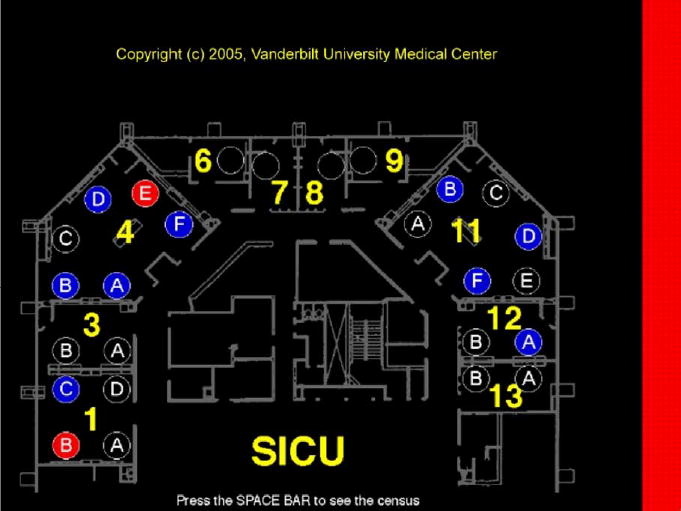
CPOE “map” view of hospital ward. Map indicates beds (circles) with new, urgent “stat” (red shading in circle) orders and those with new “routine” orders (blue shading in circle); right border shading (red or blue) indicates highest priority of new orders not yet acknowledged (across all beds) by nursing staff. (For interpretation of the references to color in this figure legend, the reader is referred to the web version of this paper.)
Fig. 9.
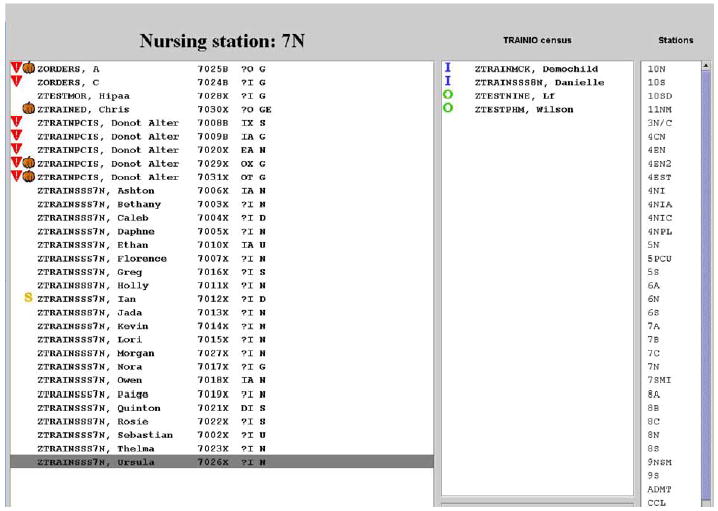
“Patient list” view of CPOE ward census. Several graphical “icon” alerts (left margin next to patient name) provide useful information regarding ward census at a glance. The inverted triangles provide duplicate last name warnings; “S” indicates patients on whom medical students have entered orders that must be reviewed by a licensed MD to become “activated”; and pumpkins indicate patients who have been bedded as outpatients long enough that conversion to inpatient status (or discharge to home) should be considered.
5.3. Stage of individual patient session initiation
Once the order entry session becomes specific to a selected patient, several new types of decision support-related events can occur. In WizOrder, once the patient is identified, the system retrieves all relevant past (active and inactive) orders for the patient, and previously stored patient-specific information such as weight, height, coded allergies, and active protocols (with related “date of protocol initiation” information). As the user waits for the initial patient-specific CPOE screen to appear, WizOrder queries the patient data repository to obtain the patient’s recent laboratory results for common important tests, in order to assist with subsequent CPOE decision support recommendations.
Ability to recover from an interrupted CPOE session without loss of work (time and effort) is critical to busy clinicians’ acceptance of such systems. Lost sessions can occur due to system “bugs” (such as a disk becoming unexpectedly full), due to environmental factors (such as network outages or power failures), and due to user factors (such as abandoning a workstation during a medical emergency, with subsequent “session timeout”). On-line Fig. 10 shows the alert that occurs upon initiation of a patient-specific CPOE session for a patient with a previously interrupted session. The user is then given option to “play back” and recover the orders from the previously interrupted session.
Among the many other types of alerts that can occur at the stage of initiating a patient-specific CPOE session are: presentation of a summary of past alerts and warnings related to the patient’s orders—e.g., allergies and drug interactions; notification of medications about to expire; display of the names of active protocols for the patient (e.g., “Deep Venous Thrombosis prophylaxis protocol”); and, promotion via reminders of new protocols for which patient is eligible. Fig. 11 illustrates an “admission wizard” which indicates to the user, for the ward on which the patient is bedded, the commonly used, evidence-based “best of care” order sets that are available within the system, and encourages the user to select one for use on the patient, if applicable. The structure of such an order set, once selected, is shown in Fig. 4 in the upper right window (pane #2).
Fig. 11.
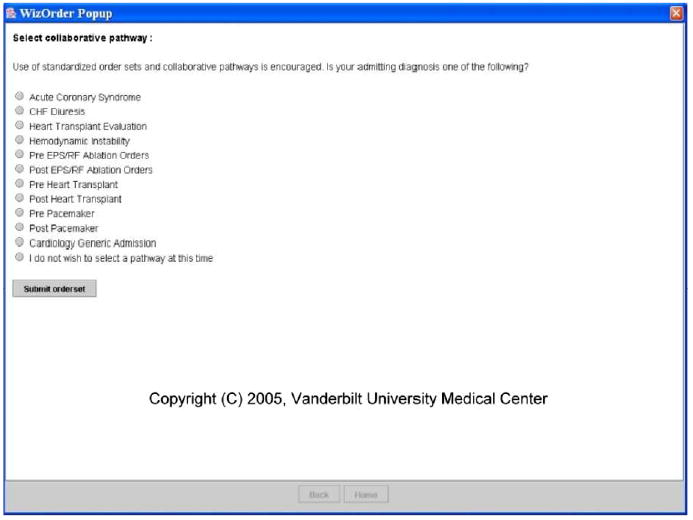
Admission Wizard prompts user to select evidence-based protocol for patient when relevant to case.
5.4. Stage of individual (single) order selection
Upon selecting a specific CPOE orderable item, and before the details of the order are provided by the user, certain decision support checks may be appropriate. In order to not waste the user’s time, once a drug name is identified as being “the next order,” and before the user specifies the details of the drug order (dose, route, frequency, etc), CPOE-based allergy and drug interaction checking should issue any relevant warnings. Fig. 12 illustrates a WizOrder drug–drug interaction warning after entry of new medication name.
Fig. 12.
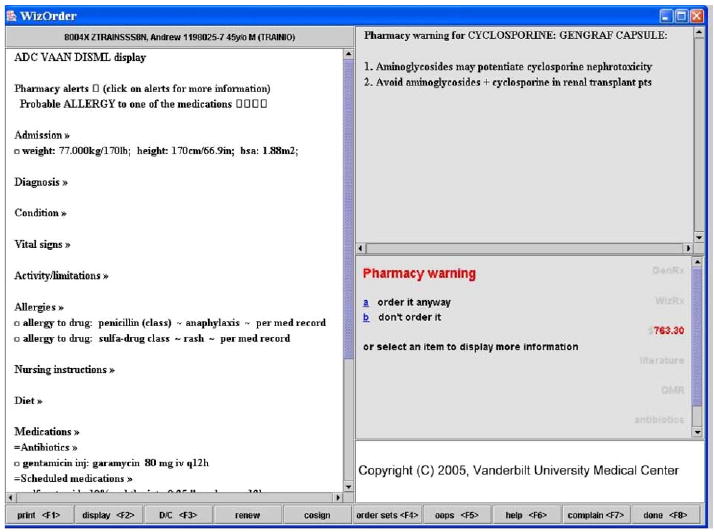
Drug–drug interaction warning after entry of new medication name.
Individual order selection can also trigger protocol-based interventions—such as recommending drug substitutions (suggesting a less expensive or more effective medication than the one originally selected). Similarly, single order selection can initiate computer-based advisers related to the specific order (on-line Figs. 13A and B). A similar mechanism that redirects physician workflow occurs in the BloodLink-Guideline system for test ordering [58]. Many CPOE systems offer the capability to link order sets to individual selectable orders (i.e., to transfer the user to an order set when an individual order is selected)[56,59,65,70,76]]. Order sets are described in detail in Section 5.
5.5. Stage of individual (single) order construction
Once the order name has been selected, the CPOE system assists the user in completing required steps for order construction (see Fig. 14 for example of instructions during cyclosporine ordering), and present alerts for potentially incorrect decisions. Both the BICS CPOE application and WizOrder guide medication order construction by highlighting recommended drug doses and drug frequencies [66,73]. Many CPOE systems also provide computer-based advisors to enforce compliance with established, evidence-based guidelines [58,77]. For instance, the antimicrobial advisor order entry system at LDS Hospital in Salt Lake City recommends therapy options for critically ill patients based on patient vital signs and serology, microbiology, pathology, and radiology results [77].
Fig. 14.
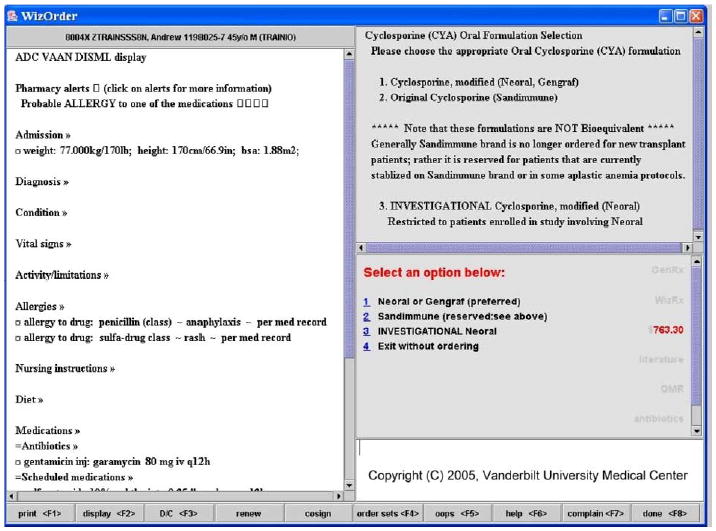
“In-line,” patient-specific, interactive advice for clinician while attempting to prescribe cyclosporine for patient; developed by experts in Pharmacy to guide clinician to best choice.
Based on ongoing studies involving the BICS [73,85], Bates et al. [86] observed that clinicians generally take the path of least resistance (see “Ten Commandments of Effective Clinical Decision Support”). Providing effective decision support involves not only alerting the provider about a potential error, but providing a correct alternative option as well. For instance, in the BICS system, if meperidine hydrochloride is prescribed for a patient whose creatinine clearance (a measure of renal function), is significantly diminished, an alert notifies the user that the drug might possibly promote seizures in this patient, and suggests a substitute medication [84].
5.6. Stage of individual order completion
Once an individual order’s components have been fully specified (and any allergy or other alerts that might have prevented order construction have been dealt with), a number of decision support functions related to the order as a whole become appropriate. Upon completed order construction, many CPOE systems suggest corollary orders—”follow-up” tasks clinically indicated after certain orders [73,84,87,88]. For example, after ordering gentamicin, an antibiotic, it is often appropriate to order serum drug levels. On-line Fig. 15 illustrates this capability in WizOrder. The Regenstrief Medical Record System (RMRS) system presents corollary orders for many drug–drug monitoring test pairs (e.g., warfarin prescriptions and related INR/prothrombin time tests) and for drug–drug side effect pairs (e.g., prescription of class II narcotics and orders for stool softeners to treat/prevent the constipation caused by narcotics) [87]. Another example is the BICS system offering clinicians the opportunity to order heparin (to prevent deep venous thrombosis, DVT) after a completed order for bed rest (which predisposes to DVT) [84].
5.7. Stage of ordering session completion
Once the user has specified all individual new (or modified) orders and wishes to finalize the ordering session, various decision support-related “exit checks” are appropriate. As noted in Section 3, recurring reminders to do what the clinician-user already intendeds to do are not well tolerated. Instead of using corollary orders to prompt PTT and INR monitoring after orders for heparin and warfarin, respectively, WizOrder waits until the ordering session is complete. At that point, it becomes “fair game” to issue warnings if appropriate monitoring tests have not been issued. Conversely, if during a given ordering session, a clinician discontinues either the heparin infusion or the PTT monitoring tests but not the other item of the pair, it is appropriate to use an “exit check” that warns the clinician that parallel actions to discontinue both are usually called for. Fig. 16 and on-line Fig. 17 illustrate the two-part WizOrder exit check for ordering (or updating) the Richmond Agitation and Sedation Score (RASS) target score whenever pain medications or sedatives are ordered for a patient in an intensive care unit (ICU).
Fig. 16.
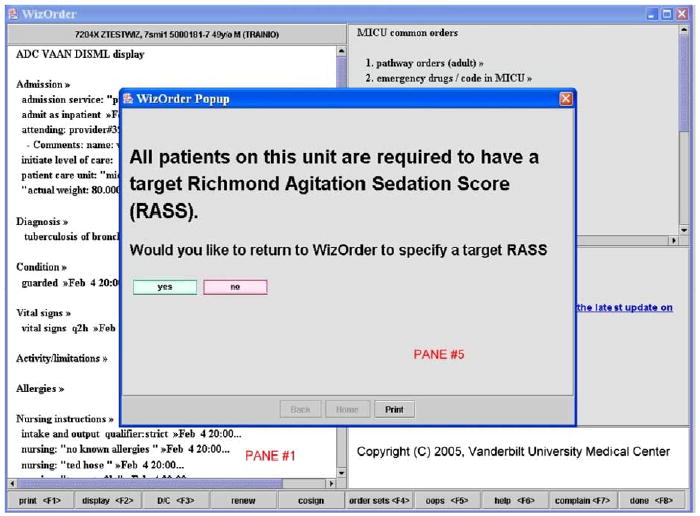
WizOrder “exit check”—on completing admission orders on an ICU patient, if the clinician-user has not specified a target RASS (Richmond Agitation Sedation Scale) score, the system uses a pop-up alert to remind the clinician that it is ICU policy to do so.
6. Six CPOE intervention approaches—from “subtle” to “intrusive”
While the interfaces of successful CPOE systems are rarely “seamless,” users adapt to their styles of workflow after training and repeated use. Once acclimated to the CPOE system workflows, users do not appreciate interruptions that deter them from the previously noted “path of least resistance” [86]. Determining whether, how, and when to disrupt clinician workflows to provide appropriate decision support is critical to end-user acceptance of both the decision support and the CPOE system overall. The authors describe a number of approaches to introducing decision support, from non-disruptive to very disruptive, and give examples of where each may be called for.
6.1. Incidental display of relevant information
Presentation of “additional” viewable text on a portion of the “usual” application screen allows the user direct access to relevant information with minimal interruption to workflow. Because no user input (e.g. acknowledgment of the information) is required, and no additional information is available (e.g., the user cannot “click on” or “select” the displayed information to learn more), the clinician is free to read or to ignore the displayed information. For example, the RMRS Gopher CPOE system [57] displays the guidelines for vaccine administration alongside an order set menu for pneumonia and flu vaccines [81]. Wiz-Order displays the most recent results of serum electrolyte tests during ordering of intravenous fluid therapy (on-line Fig. 18 shows a variant web-based version of this genre). WizOrder also display of relevant dosing information for prescribing medications—for example, on pediatric units, the patient’s actual weight, dosing weight, and pharmacy-recommended dosing guidelines (see Fig. 7). Information relating to costs may be displayed as well.
6.2. Incidental display of linked education opportunities
A CPOE system may have order-related educational information that is too voluminous to intercalate into the “usual” order entry screen. Under such circumstances, the CPOE system can present links for users to select (“click on”) that lead to a separate screen/window providing the relevant textual information. The Medicator CPOE system in Amsterdam displays links to relevant drug guidelines and formulary information [59]. The Vanderbilt Patient Care Provider Order Entry with Integrated Tactical Support study [55] provided links to pharmacotherapy-related information (illustrated by the “GenRx” and “WizRx” links on the right margin of pane #3, Fig. 2), and reference material for diagnosis in internal medicine. On-line Fig. 19 provides an example, in pane #5, of displaying an evidence-based summary of what is known about a specific drug interaction (selected by the user from the drug interaction warnings list of Fig. 19, pane #2). In the BICS system, as clinicians review recommended drug doses for patients with renal impairment, they can display of the data used to calculate creatinine clearance using a keyboard shortcut link [64].
6.3. Interactive sequential advice for user-directed clinical activity
By presenting stepwise instructions in context, CPOE systems help users to carry out discrete tasks. Fig. 2 presents the default “minimum” type of advice that WizOrder provides for order construction; Fig. 14 provides a more complex example whereby the user is sequentially prompted, through questions and answers, to order the most appropriate form of cyclosporine for the patient. The BloodLink-Guideline system [58] directs blood test ordering decisions by first having the clinician select the appropriate guideline, then presenting a menu of related indications, and finally, presenting a menu of relevant tests for a selected indication.
6.4. “Recallable” best practice guidelines with actionable pre-formed “pick list” selections
Order sets are pick lists containing constituent individual “pre-specified” full orders, often representing standardized protocols. Fig. 4 illustrates a portion of the WizOrder order set for “acute coronary syndrome.” Order sets are often presented in hierarchies for easy access, organized by Clinical Department [40,59] by organ system or by clinical diagnosis, condition or procedure [57,76,89]. While picking orders from order sets may be viewed as disruptive to the usual workflow of creating individual orders, in many CPOE systems, appropriate use of order sets can increase users’ time-efficiency [90] and promote completeness and correctness of orders [60]. The BloodLink-Guideline, test ordering system used guideline-driven order sets to achieve a 20% reduction in test ordering [58].
6.5. “Pop-up” alerts that interrupt workflow and require a response for the user to continue
Pop-up alerts can present clinically important information (in a separate user interface window) that must be “acknowledged” by the user before resuming previous CPOE activity. Use of such interventions is typically viewed by users as disruptive, and should be reserved for only the most severe clinical indications. “Pop-up fatigue” can occur when too many alerts of this type disrupt clinical workflows [91]. In both the BICS system [92] and WizOrder [48], pop-up windows alert physicians when excessive chemotherapy doses are ordered. On-line Fig. 20 illustrates how a WizOrder user is notified that the most recently laboratory test ordered will be “sent out” to a reference laboratory for completion, and provides advice on how to optimize ordering with respect to institutional policies regarding reimbursement for testing. This mechanism is used in both the BICS system and WizOrder to display hospital approved drug substitution regimens. For example, in BICS, if any other histamine-2 blocker is ordered, a pop-up informs the user that nizatidine will be substituted [73]. Fig. 21 shows a corresponding WizOrder drug substitution pop-up (implemented as an advisor, method 6 below). Fig. 16 shows how the RASS exit check was implemented as a pop-up alert in WizOrder. Fig. 12 illustrates how WizOrder uses the pop-up method to present a drug interaction alert.
Fig. 21.
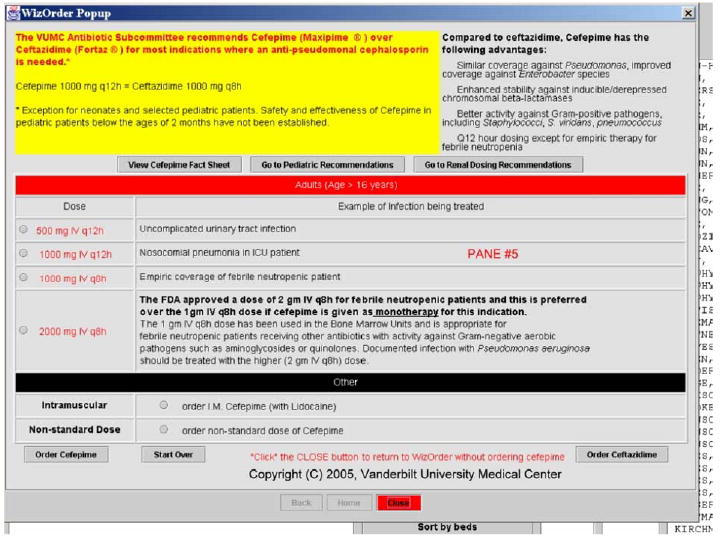
User ordered an antibiotic for which the Pharmaceuticals and Therapeutics (P&T) Committee had recommended a substitution. A variant “pop-up,” this educational advisor guides clinician through ordering alternative antibiotic. Links to “package inserts” (via buttons) detail how to prescribe recommended drug under various circumstances. A physician who knows little about the recommended drug could learn enough to prescribe it appropriately.
6.6. Complex, computer-based protocols that interact with the user to make patient-specific calculations and recommendations
The most complex form of decision support is an interactive advisor that integrates patient-specific information (laboratory results, active orders, weight, allergies, etc) with complex guidelines or protocols, and presents calculated/derived information to the user for decision-making, typically involving a two-way dialogue between the application and the user. Complex advisors may combine educational advice, “calculators” for patient-specific dosing, and other functionality in one screen. The LDS Hospital in Salt Lake City uses an antimicrobial advisor to assist clinicians in determining treatment for microbial diseases [77]. The LDS advisor analyzes patient data and laboratory results in order to determine likely pathogens and then determines the optimal treatment for the patient, including factors such as patient allergies and local patterns of antimicrobial functions into its assessment [77]. In WizOrder, the web-browser pop-up window is used to dynamically generate patient-specific advisor content [49,50]. Fig. 22 illustrates the WizOrder total parenteral nutrition (TPN) ordering advisor for the neonatal intensive care unit.
Fig. 22.
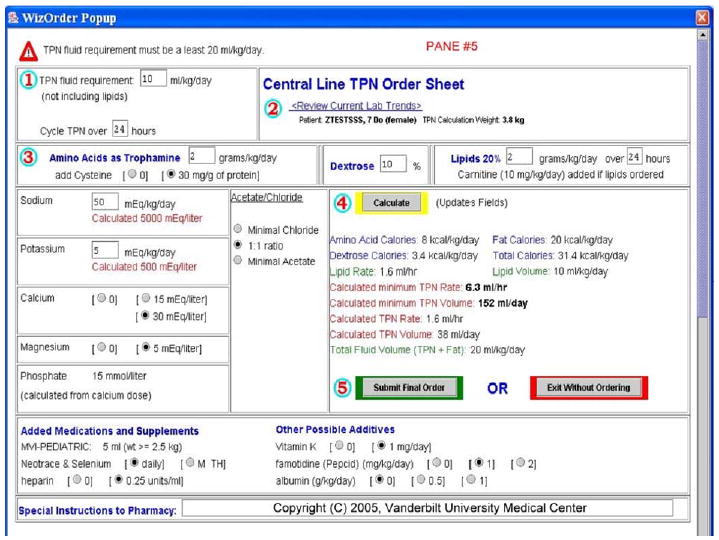
Neonatal Intensive Care Unit (NICU) Total Parenteral Nutrition (TPN) Advisor provides complex interactive advice and performs various calculations.
7. Conclusion
It is critical that system developers, the technologists maintaining the system, and clinical experts collaborate in managing clinical systems during development. Implementing decision support capabilities within clinical systems requires an understanding of the clinical significance of a proposed intervention, detailed knowledge of the intervention itself, and a good understanding of the workflows of the clinicians who will be affected by the intervention. The authors have described multiple mechanisms for delivering decision support within the context of CPOE systems. There are three important axes to consider: the role for decision support, when to intervene, and the method of intervention. Framing decision support in this manner may help both developers and clinical end-users to understand how to tailor the system whenever new decision support needs arise. This framework may also be useful when evaluating and reviewing decision support within CPOE systems.
Offering decision support within a CPOE system provides both clinical end-users and institutional administrators with the opportunity to change substantially the way that an institution carries out its work, and to improve patient care processes in terms of quality and safety.
Supplementary Material
Acknowledgments
Drs. Miller and Waitman’s efforts were supported in part by National Library of Medicine Grants R01-LM-007995 and R01-LM-06226. Dr. Rosenbloom’s efforts were supported in part by a National Library of Medicine Grant K22-LM-08576. Ms. Chen’s efforts were supported by the Vanderbilt University School of Medicine. The ‘WizOrder’ CPOE system was developed by Vanderbilt University faculty within the School of Medicine beginning in 1994. The product was not commercialized until May–June of 2001. At that time, Vanderbilt University entered into a marketing agreement with McKesson to commercially sell and distribute the ‘WizOrder Care’ Provider Order Entry (CPOE) System, after rewriting and recasting it as “Horizon Expert Orders” in McKesson’s product line. The authors have referred to the system throughout the manuscript by its name at Vanderbilt, WizOrder. All descriptions are of system components developed at Vanderbilt University and not by the commercial vendor. Drs. Miller and Waitman, coauthors of the manuscript, have been recognized by Vanderbilt as contributing authors of the WizOrder software, or have received compensation from Vanderbilt as part of its effort to commercialize the software. They will continue to receive royalties from Vanderbilt under the University’s intellectual property policies. None of the authors is an employee of McKesson or a stockholder in the company, and all compensation related to the commercialization has come from Vanderbilt University to the authors (and none directly from the company). Dr. Rosenbloom has in the past been paid by McKesson to demonstrate the software to potential clients. McKesson has neither seen nor approved of this manuscript. While these involvements of the authors could potentially be viewed as a conflict of interest with respect to the submitted manuscript, the authors note that by publishing this description in a widely available journal, it is possible that competitor CPOE system vendors could benefit from the information provided, potentially offsetting any increased publicity for the system gained through this publication. Dr. Antoine Geissbuhler was the original author of the WizOrder program at Vanderbilt, and Dr. Douglas Talbert later added to the WizOrder code. Dr. Asli Ozdas helped to design the Admission Wizard shown in Fig. 11. The authors thank Ms. Elizabeth Madsen for copy-editing assistance. A talk describing limited aspects of this work was presented by Dr. Miller at a Symposium honoring Dr. Jochen Moehr at the University of Victoria, British Columbia, in June 2005.
Appendix A. Supplementary data
Supplementary data associated with this article can be found, in the online version, at doi:10.1016/j.jbi.2005.08. 009.
References
- 1.Kassirer JP, Gorry GA. Clinical problem solving: a behavioral analysis. Ann Intern Med. 1978;89(2):245–55. doi: 10.7326/0003-4819-89-2-245. [DOI] [PubMed] [Google Scholar]
- 2.Covell DG, Uman GC, Manning PR. Information needs in office practice: are they being met? Ann Intern Med. 1985;103(4):596–599. doi: 10.7326/0003-4819-103-4-596. [DOI] [PubMed] [Google Scholar]
- 3.Kassirer JP, Kopelman RI. Knowledge and clinical expertise. Hosp Pract (Off Ed) 1988;23(3):46. doi: 10.1080/21548331.1988.11703436. 53, 57 passim. [DOI] [PubMed] [Google Scholar]
- 4.Jelovsek FR, Rittwage J, Pearse WH, Visscher HC. Information management needs of the obstetrician-gynecologist—a survey. Obstet Gynecol. 1989;73(3 Pt 1):395–9. [PubMed] [Google Scholar]
- 5.Williamson JW, German PS, Weiss R, Skinner EA, Bowes third F. Health science information management and continuing education of physicians. A survey of U.S. primary care practitioners and their opinion leaders. Ann Intern Med. 1989;110(2):151–60. doi: 10.7326/0003-4819-110-2-151. [DOI] [PubMed] [Google Scholar]
- 6.Timpka T, Arborelius E. The GP’s dilemmas: a study of knowledge need and use during health care consultations. Methods Inf Med. 1990;29(1):23–9. [PubMed] [Google Scholar]
- 7.Berner ES, Shugerman AA. Needs assessment for diagnostic decision support systems (DDSS) Proc Annu Symp Comput Appl Med Care. 1991:605–8. [PMC free article] [PubMed] [Google Scholar]
- 8.Osheroff JA, Forsythe DE, Buchanan BG, Bankowitz RA, Blumenfeld BH, Miller RA. Physicians’ information needs: analysis of questions posed during clinical teaching. Ann Intern Med. 1991;114(7):576–81. doi: 10.7326/0003-4819-114-7-576. [DOI] [PubMed] [Google Scholar]
- 9.Forsythe DE, Buchanan BG, Osheroff JA, Miller RA. Expanding the concept of medical information: an observational study of physicians’ information needs. Comput Biomed Res. 1992;25(2):181–200. doi: 10.1016/0010-4809(92)90020-b. [DOI] [PubMed] [Google Scholar]
- 10.Bowden VM, Kromer ME, Tobia RC. Assessment of physicians’ information needs in five Texas counties. Bull Med Libr Assoc. 1994;82(2):189–96. [PMC free article] [PubMed] [Google Scholar]
- 11.Gorman PN, Ash J, Wykoff L. Can primary care physicians’ questions be answered using the medical journal literature? Bull Med Libr Assoc. 1994;82(2):140–6. [PMC free article] [PubMed] [Google Scholar]
- 12.Lundeen GW, Tenopir C, Wermager P. Information needs of rural health care practitioners in Hawaii. Bull Med Libr Assoc. 1994;82(2):197–205. [PMC free article] [PubMed] [Google Scholar]
- 13.Wildemuth BM, de Bliek R, Friedman CP, Miya TS. Information-seeking behaviors of medical students: a classification of questions asked of librarians and physicians. Bull Med Libr Assoc. 1994;82(3):295–304. [PMC free article] [PubMed] [Google Scholar]
- 14.Verhoeven AA, Boerma EJ, Meyboomde Jong B. Use of information sources by family physicians: a literature survey. Bull Med Libr Assoc. 1995;83(1):85–90. [PMC free article] [PubMed] [Google Scholar]
- 15.McDonald CJ. Protocol-based computer reminders, the quality of care and the non-perfectability of man. N Engl J Med. 1976;295(24):1351–5. doi: 10.1056/NEJM197612092952405. [DOI] [PubMed] [Google Scholar]
- 16.McDonald CJ, Wilson GA, McCabe GP., Jr Physician response to computer reminders. JAMA. 1980;244(14):1579–81. [PubMed] [Google Scholar]
- 17.Tierney WM, Hui SL, McDonald CJ. Delayed feedback of physician performance versus immediate reminders to perform preventive care. Effects on physician compliance. Med Care. 1986;24(8):659–66. doi: 10.1097/00005650-198608000-00001. [DOI] [PubMed] [Google Scholar]
- 18.Tierney WM, McDonald CJ, Martin DK, Rogers MP. Computerized display of past test results. Effect on outpatient testing. Ann Intern Med. 1987;107(4):569–74. doi: 10.7326/0003-4819-107-4-569. [DOI] [PubMed] [Google Scholar]
- 19.McDonald CJ, Tierney WM. Computer-stored medical records. Their future role in medical practice. JAMA. 1988;259(23):3433–40. [PubMed] [Google Scholar]
- 20.Tierney WM, McDonald CJ, Hui SL, Martin DK. Computer predictions of abnormal test results. Effects on outpatient testing. JAMA. 1988;259(8):1194–8. [PubMed] [Google Scholar]
- 21.McDonald CJ. Computers. JAMA. 1989;261(19):2834–6. [PubMed] [Google Scholar]
- 22.Tierney WM, Miller ME, McDonald CJ. The effect on test ordering of informing physicians of the charges for outpatient diagnostic tests. N Engl J Med. 1990;322(21):1499–504. doi: 10.1056/NEJM199005243222105. [DOI] [PubMed] [Google Scholar]
- 23.McDonald CJ, Tierney WM, Overhage JM, Martin DK, Wilson GA. The Regenstrief Medical Record System: 20 years of experience in hospitals, clinics, and neighborhood health centers. MD Comput. 1992;9(4):206–17. [PubMed] [Google Scholar]
- 24.Tierney WM, Miller ME, Overhage JM, McDonald CJ. Physician inpatient order writing on microcomputer workstations. Effects on resource utilization. JAMA. 1993;269(3):379–83. [PubMed] [Google Scholar]
- 25.McDonald CJ, Overhage JM. Guidelines you can follow and can trust. An ideal and an example [Editorial; comment] JAMA. 1994;271(11):872–3. [PubMed] [Google Scholar]
- 26.Warner HR, Olmsted CM, Rutherford BD. HELP—a program for medical decision-making. Comput Biomed Res. 1972;5(1):65–74. doi: 10.1016/0010-4809(72)90007-9. [DOI] [PubMed] [Google Scholar]
- 27.Evans RS, Larsen RA, Burke JP, Gardner RM, Meier FA, Jacobson JA, et al. Computer surveillance of hospital-acquired infections and antibiotic use. JAMA. 1986;256(8):1007–11. [PubMed] [Google Scholar]
- 28.Larsen RA, Evans RS, Burke JP, Pestotnik SL, Gardner RM, Classen DC. Improved perioperative antibiotic use and reduced surgical wound infections through use of computer decision analysis. Infect Control Hosp Epidemiol. 1989;10(7):316–20. doi: 10.1086/646035. [DOI] [PubMed] [Google Scholar]
- 29.Gardner RM, Golubjatnikov OK, Laub RM, Jacobson JT, Evans RS. Computer-critiqued blood ordering using the HELP system. Comput Biomed Res. 1990;23(6):514–28. doi: 10.1016/0010-4809(90)90038-e. [DOI] [PubMed] [Google Scholar]
- 30.Pestotnik SL, Evans RS, Burke JP, Gardner RM, Classen DC. Therapeutic antibiotic monitoring: surveillance using a computerized expert system. Am J Med. 1990;88(1):43–8. doi: 10.1016/0002-9343(90)90126-x. [DOI] [PubMed] [Google Scholar]
- 31.Evans RS, Pestotnik SL, Classen DC, Bass SB, Menlove RL, Gardner RM, et al. Development of a computerized adverse drug event monitor. Proc Annu Symp Comput Appl Med Care. 1991:23–7. [PMC free article] [PubMed] [Google Scholar]
- 32.Lepage EF, Gardner RM, Laub RM, Jacobson JT. Assessing the effectiveness of a computerized blood order “consultation” system. Proc Annu Symp Comput Appl Med Care. 1991:33–7. [PMC free article] [PubMed] [Google Scholar]
- 33.Classen DC, Evans RS, Pestotnik SL, Horn SD, Menlove RL, Burke JP. The timing of prophylactic administration of antibiotics and the risk of surgical-wound infection [See comments] N Engl J Med. 1992;326(5):281–6. doi: 10.1056/NEJM199201303260501. [DOI] [PubMed] [Google Scholar]
- 34.Evans RS, Pestotnik SL, Classen DC, Bass SB, Burke JP. Prevention of adverse drug events through computerized surveillance. Proc Annu Symp Comput Appl Med Care. 1992:437–41. [PMC free article] [PubMed] [Google Scholar]
- 35.Hales JW, Gardner RM, Huff SM. Integration of a stand-alone expert system with a hospital information system. Proc Annu Symp Comput Appl Med Care. 1992:427–31. [PMC free article] [PubMed] [Google Scholar]
- 36.Evans RS, Classen DC, Stevens LE, Pestotnik SL, Gardner RM, Lloyd JF. Using a hospital information system to assess the effects of adverse drug events. Proc Annu Symp Comput Appl Med Care. 1993:161–5. [PMC free article] [PubMed] [Google Scholar]
- 37.Gardner RM, Christiansen PD, Tate KE, Laub MB, Holmes SR. Computerized continuous quality improvement methods used to optimize blood transfusions. Proc Annu Symp Comput Appl Med Care. 1993:166–70. [PMC free article] [PubMed] [Google Scholar]
- 38.Evans RS, Classen DC, Pestotnik SL, Lundsgaarde HP, Burke JP. Improving empiric antibiotic selection using computer decision support. Arch Intern Med. 1994;154(8):878–84. [PubMed] [Google Scholar]
- 39.White KS, Lindsay A, Pryor TA, Brown WF, Walsh K. Application of a computerized medical decision-making process to the problem of digoxin intoxication. J Am Coll Cardiol. 1984;4(3):571–6. doi: 10.1016/s0735-1097(84)80104-7. [DOI] [PubMed] [Google Scholar]
- 40.Halpern NA, Thompson RE, Greenstein RJ. A computerized intensive care unit order-writing protocol. Ann Pharmacother. 1992;26(2):251–4. doi: 10.1177/106002809202600222. [DOI] [PubMed] [Google Scholar]
- 41.Dambro MR, Weiss BD, McClure CL, Vuturo AF. An unsuccessful experience with computerized medical records in an academic medical center. J Med Educ. 1988;63(8):617–23. doi: 10.1097/00001888-198808000-00005. [DOI] [PubMed] [Google Scholar]
- 42.Williams LS. Microchips versus stethoscopes: Calgary hospital, MDs face off over controversial computer system [See comments] CMAJ. 1992;147(10):1534–40. 1543–4, 1547. [PMC free article] [PubMed] [Google Scholar]
- 43.Massaro TA. Introducing physician order entry at a major academic medical center: II. Impact on medical education. Acad Med. 1993;68(1):25–30. doi: 10.1097/00001888-199301000-00004. [DOI] [PubMed] [Google Scholar]
- 44.Massaro TA. Introducing physician order entry at a major academic medical center: I. Impact on organizational culture and behavior. Acad Med. 1993;68(1):20–5. doi: 10.1097/00001888-199301000-00003. [DOI] [PubMed] [Google Scholar]
- 45.Geissbuhler A, Miller RA. A new approach to the implementation of direct care-provider order entry. Proc AMIA Annu Fall Symp. 1996:689–93. [PMC free article] [PubMed] [Google Scholar]
- 46.Stead WW, Borden R, Bourne J, Giuse D, Giuse N, Harris TR, et al. The Vanderbilt University fast track to IAIMS: transition from planning to implementation. J Am Med Inform Assoc. 1996;3(5):308–17. doi: 10.1136/jamia.1996.97035022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Geissbuhler A, Grande JF, Bates RA, Miller RA, Stead WW. Design of a general clinical notification system based on the publish-subscribe paradigm. Proc AMIA Annu Fall Symp. 1997:126–30. [PMC free article] [PubMed] [Google Scholar]
- 48.Geissbuhler A, Miller RA, Stead WWThe clinical spectrum of decision-support in oncology with a case report of a real world system. In: AIME. Grenoble: Springer Berlin; 1997.
- 49.Heusinkveld J, Geissbuhler A, Sheshelidze D, Miller R. A programmable rules engine to provide clinical decision support using HTML forms. Proc AMIA Symp. 1999:800–3. [PMC free article] [PubMed] [Google Scholar]
- 50.Starmer JM, Talbert DA, Miller RA. Experience using a programmable rules engine to implement a complex medical protocol during order entry. Proc AMIA Symp. 2000:829–32. [PMC free article] [PubMed] [Google Scholar]
- 51.Stead WW, Bates RA, Byrd J, Giuse DA, Miller RA, Shultz EK. Case Study: The Vanderbilt University Medical Center Information Management Architecture. In: Van De Velde R, Degoulet P, editors. Clinical information systems: a component-based approach. Springer-Verlag; 2003.
- 52.Neilson EG, Johnson KB, Rosenbloom ST, Dupont WD, Talbert D, Giuse DA, et al. The impact of peer management on test-ordering behavior. Ann Intern Med. 2004;141(3):196–204. doi: 10.7326/0003-4819-141-3-200408030-00008. [DOI] [PubMed] [Google Scholar]
- 53.Potts AL, Barr FE, Gregory DF, Wright L, Patel NR. Computerized physician order entry and medication errors in a pediatric critical care unit. Pediatrics. 2004;113(1 Pt 1):59–63. doi: 10.1542/peds.113.1.59. [DOI] [PubMed] [Google Scholar]
- 54.Rosenbloom ST, Chiu KW, Byrne DW, Talbert DA, Neilson EG, Miller RA. Interventions to regulate ordering of serum magnesium levels: an unintended consequence of decision support. J Am Med Inform Assoc 2005. [DOI] [PMC free article] [PubMed]
- 55.Rosenbloom ST, Geissbuhler AJ, Dupont WD, Giuse DA, Talbert DA, Tierney WM, et al. Effect of CPOE user interface design on user-initiated access to educational and patient information during clinical care. J Am Med Inform Assoc 2005. [DOI] [PMC free article] [PubMed]
- 56.Teich JM, Spurr CD, Schmiz JL, O’Connell EM, Thomas D. Enhancement of clinician workflow with computer order entry. Proc Annu Symp Comput Appl Med Care. 1995:459–63. [PMC free article] [PubMed] [Google Scholar]
- 57.McDonald CJ, Overhage JM, Tierney WM, Dexter PR, Martin DK, Suico JG, et al. The Regenstrief Medical Record System: a quarter century experience. Int J Med Inform. 1999;54(3):225–53. doi: 10.1016/s1386-5056(99)00009-x. [DOI] [PubMed] [Google Scholar]
- 58.van Wijk MA, van der Lei J, Mosseveld M, Bohnen AM, van Bemmel JH. Assessment of decision support for blood test ordering in primary care: a randomized trial. Ann Intern Med. 2001;134(4):274–81. doi: 10.7326/0003-4819-134-4-200102200-00010. [DOI] [PubMed] [Google Scholar]
- 59.Kalmeijer MD, Holtzer W, van Dongen R, Guchelaar HJ. Implementation of a computerized physician medication order entry system at the Academic Medical Centre in Amsterdam. Pharm World Sci. 2003;25(3):88–93. doi: 10.1023/a:1024008600247. [DOI] [PubMed] [Google Scholar]
- 60.Payne TH, Hoey PJ, Nichol P, Lovis C. Preparation and use of preconstructed orders, order sets, and order menus in a computerized provider order entry system. J Am Med Inform Assoc. 2003;10(4):322–9. doi: 10.1197/jamia.M1090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Oppenheim MI, Vidal C, Velasco FT, Boyer AG, Cooper MR, Hayes JG, et al. Impact of a computerized alert during physician order entry on medication dosing in patients with renal impairment. Proc AMIA Symp. 2002:577–81. [PMC free article] [PubMed] [Google Scholar]
- 62.Kuperman GJ, Teich JM, Tanasijevic MJ, Ma’Luf N, Rittenberg E, Jha A, et al. Improving response to critical laboratory results with automation: results of a randomized controlled trial. J Am Med Inform Assoc. 1999;6(6):512–22. doi: 10.1136/jamia.1999.0060512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Stead WW, Miller RA, Musen MA, Hersh WR. Integration and beyond: linking information from disparate sources and into work-flow [See comments] J Am Med Inform Assoc. 2000;7(2):135–45. doi: 10.1136/jamia.2000.0070135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Chertow GM, Lee J, Kuperman GJ, Burdick E, Horsky J, Seger DL, et al. Guided medication dosing for inpatients with renal insufficiency. JAMA. 2001;286(22):2839–44. doi: 10.1001/jama.286.22.2839. [DOI] [PubMed] [Google Scholar]
- 65.Murff HJ, Kannry J. Physician satisfaction with two order entry systems. J Am Med Inform Assoc. 2001;8(5):499–509. doi: 10.1136/jamia.2001.0080499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Kuperman GJ, Teich JM, Gandhi TK, Bates DW. Patient safety and computerized medication ordering at Brigham and Women’s Hospital. Jt Comm J Qual Improv. 2001;27(10):509–21. doi: 10.1016/s1070-3241(01)27045-x. [DOI] [PubMed] [Google Scholar]
- 67.Bizovi KE, Beckley BE, McDade MC, Adams AL, Lowe RA, Zechnich AD, et al. The effect of computer-assisted prescription writing on emergency department prescription errors. Acad Emerg Med. 2002;9(11):1168–75. doi: 10.1111/j.1553-2712.2002.tb01572.x. [DOI] [PubMed] [Google Scholar]
- 68.Barlow IW, Flynn NA, Britton JM. The Basingstoke Orthopaedic Database: a high quality accurate information system for audit. Ann R Coll Surg Engl. 1994;76(Suppl 6):285–7. [PubMed] [Google Scholar]
- 69.Apkon M, Singhaviranon P. Impact of an electronic information system on physician workflow and data collection in the intensive care unit. Intensive Care Med. 2001;27(1):122–30. doi: 10.1007/s001340000777. [DOI] [PubMed] [Google Scholar]
- 70.Teich JM, Glaser JP, Beckley RF, Aranow M, Bates DW, Kuperman GJ, et al. The Brigham integrated computing system (BICS): advanced clinical systems in an academic hospital environment. Int J Med Inform. 1999;54(3):197–208. doi: 10.1016/s1386-5056(99)00007-6. [DOI] [PubMed] [Google Scholar]
- 71.Bates DW, Kuperman G, Teich JM. Computerized physician order entry and quality of care. Qual Manag Health Care. 1994;2(4):18–27. [PubMed] [Google Scholar]
- 72.Bates DW. Using information technology to reduce rates of medication errors in hospitals. BMJ. 2000;320(7237):788–91. doi: 10.1136/bmj.320.7237.788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Teich JM, Merchia PR, Schmiz JL, Kuperman GJ, Spurr CD, Bates DW. Effects of computerized physician order entry on prescribing practices. Arch Intern Med. 2000;160(18):2741–7. doi: 10.1001/archinte.160.18.2741. [DOI] [PubMed] [Google Scholar]
- 74.Bates DW, Cohen M, Leape LL, Overhage JM, Shabot MM, Sheridan T. Reducing the frequency of errors in medicine using information technology. J Am Med Inform Assoc. 2001;8(4):299–308. doi: 10.1136/jamia.2001.0080299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Tierney WM, Overhage JM, McDonald CJ. Computerizing guidelines: factors for success. Proc AMIA Annu Fall Symp. 1996:459–62. [PMC free article] [PubMed] [Google Scholar]
- 76.Chin HL, Wallace P. Embedding guidelines into direct physician order entry: simple methods, powerful results. Proc AMIA Symp. 1999:221–5. [PMC free article] [PubMed] [Google Scholar]
- 77.Evans RS, Pestotnik SL, Classen DC, Clemmer TP, Weaver LK, Orme JF, Jr, et al. A computer-assisted management program for antibiotics and other antiinfective agents. N Engl J Med. 1998;338(4):232–8. doi: 10.1056/NEJM199801223380406. [DOI] [PubMed] [Google Scholar]
- 78.Maviglia SM, Zielstorff RD, Paterno M, Teich JM, Bates DW, Kuperman GJ. Automating complex guidelines for chronic disease: lessons learned. J Am Med Inform Assoc. 2003;10(2):154–65. doi: 10.1197/jamia.M1181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Bates DW, Kuperman GJ, Rittenberg E, Teich JM, Fiskio J, Ma’luf N, et al. A randomized trial of a computer-based intervention to reduce utilization of redundant laboratory tests. Am J Med. 1999;106(2):144–50. doi: 10.1016/s0002-9343(98)00410-0. [DOI] [PubMed] [Google Scholar]
- 80.Bates DW, Kuperman GJ, Jha A, Teich JM, Orav EJ, Ma’luf N, et al. Does the computerized display of charges affect inpatient ancillary test utilization? Arch Intern Med. 1997;157(21):2501–8. [PubMed] [Google Scholar]
- 81.Dexter PR, Wolinsky FD, Gramelspacher GP, Zhou XH, Eckert GJ, Waisburd M, et al. Effectiveness of computer-generated reminders for increasing discussions about advance directives and completion of advance directive forms. A randomized, controlled trial. Ann Intern Med. 1998;128(2):102–10. doi: 10.7326/0003-4819-128-2-199801150-00005. [DOI] [PubMed] [Google Scholar]
- 82.Gamble ER, McDonald PJ, Lichstein PR. Knowledge, attitudes, and behavior of elderly persons regarding living wills. Arch Intern Med. 1991;151(2):277–80. [PubMed] [Google Scholar]
- 83.Shojania KG, Yokoe D, Platt R, Fiskio J, Ma’luf N, Bates DW. Reducing vancomycin use utilizing a computer guideline: results of a randomized controlled trial. J Am Med Inform Assoc. 1998;5(6):554–62. doi: 10.1136/jamia.1998.0050554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Fischer MA, Solomon DH, Teich JM, Avorn J. Conversion from intravenous to oral medications: assessment of a computerized intervention for hospitalized patients. Arch Intern Med. 2003;163(21):2585–9. doi: 10.1001/archinte.163.21.2585. [DOI] [PubMed] [Google Scholar]
- 85.Harpole LH, Khorasani R, Fiskio J, Kuperman GJ, Bates DW. Automated evidence-based critiquing of orders for abdominal radiographs: impact on utilization and appropriateness. J Am Med Inform Assoc. 1997;4(6):511–21. doi: 10.1136/jamia.1997.0040511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Bates DW, Kuperman GJ, Wang S, Gandhi T, Kittler A, Volk L, et al. Ten commandments for effective clinical decision support: making the practice of evidence-based medicine a reality. J Am Med Inform Assoc. 2003;10(6):523–30. doi: 10.1197/jamia.M1370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Overhage JM, Tierney WM, Zhou XH, McDonald CJ. A randomized trial of “corollary orders” to prevent errors of omission. J Am Med Inform Assoc. 1997;4(5):364–75. doi: 10.1136/jamia.1997.0040364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Horsky J, Kaufman DR, Patel VL. Computer-based drug ordering: evaluation of interaction with a decision-support system. Medinfo. 2004;11(Pt 2):1063–77. [PubMed] [Google Scholar]
- 89.Payne TH. The transition to automated practitioner order entry in a teaching hospital: the VA Puget Sound experience. Proc AMIA Symp. 1999:589–93. [PMC free article] [PubMed] [Google Scholar]
- 90.Lovis C, Chapko MK, Martin DP, Payne TH, Baud RH, Hoey PJ, et al. Evaluation of a command-line parser-based order entry pathway for the Department of Veterans Affairs electronic patient record. J Am Med Inform Assoc. 2001;8(5):486–98. doi: 10.1136/jamia.2001.0080486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Ash JS, Berg M, Coiera E. Some unintended consequences of information technology in health care: the nature of patient care information system-related errors. J Am Med Inform Assoc. 2004;11(2):104–12. doi: 10.1197/jamia.M1471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Gainer A, Pancheri K, Zhang J. Improving the human computer interface design for a physician order entry system. AMIA Annu Symp Proc. 2003:847. [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


