Abstract
Tenosynovial giant cell tumor (TSGCT) is a disease of disputed etiology and pathogenesis. Some investigations indicate a neoplastic origin of the tumors; others indicate that they are polyclonal and inflammatory. The cytogenetic and molecular genetic features of TSGCTs are largely unknown, as only some 20 localized and 30 diffuse tumors with cytogenetic aberrations have been reported. The most common karyotypic aberrations have been trisomy for chromosomes 5 and 7 and translocations involving chromosomal area 1p11-13. We decided to screen the genomes of TSGCTs by comparative genomic hybridization (CGH) to perform interphase fluorescence in situ hybridization (IP-FISH), looking for numerical aberrations of chromosomes 1, 5, and 7, and to analyze the tumors for microsatellite instability. Except for two diffuse TSGCTs that came fresh to us, and which, by karyotyping, exhibited t(1;22)(p13;q12) and a t(1;1)(q21;p11) and +7, respectively, all studies had to be performed on formalin-fixed, paraffin-embedded material. DNA was extracted from 51 localized and nine diffuse TSGCTs. CGH was successful for 24 tumors, but none of them showed copy number changes. The IP-FISH studies showed trisomy 7 in 56% of the tumors (15/27), whereas chromosomes 1 and 5 seemed to be disomic in all TSGCTs. All informative tumors were wild-type by microsatellite instability analysis.
Keywords: Cytogenetics, TSGCT, trisomy 7, CGH, solid tumors
Introduction
Tenosynovial giant cell tumor (TSGCT), also called nodular tenosynovitis or (pigmented) villonodular synovitis, tenosynovitis, and bursitis [1], presumably arises from the synovium of tendon sheaths, joints, or bursae [2]; mostly affects adults between 30 and 50 years of age; and is slightly more common in women. Microscopically, the lesion consists of mononuclear, xanthomatous, and giant cells with variable degrees of collagenization, and it may or may not be well circumscribed by a dense, collagenous capsule. TSGCTs may be either intraarticular or extraarticular, diffuse or localized [3–5]. A mass, joint swelling, and/or pain is the most common presenting sign and symptom.
As is apparent from the variable-naming practices alluded to above, considerable uncertainties exist as to the pathogenetic mechanisms behind TSGCTs. Lyonization studies have shown a random pattern of X-inactivation [6,7] and TSGCT-like lesions have been produced experimentally with inflammatory agents [8], both suggesting a polyclonal and inflammatory pathogenesis. In contrast, another X-inactivation study found that the lesion was monoclonal [9], and also the detection of clonal chromosomal aberrations [4] and DNA aneuploidy [10] in TSGCTs point toward a neoplastic disease process. The reports of metastasizing TSGCTs [11–15] and their sometimes invasive growth further support the neoplastic hypothesis.
The cytogenetics and molecular genetics of TSGCT are not well known. To our knowledge, only 33 diffuse tumors [1,16–24] and 23 localized TSGCTs [1,22] have been karyotyped. The most frequent findings are trisomy 7 and/or trisomy 5 as well as translocations, both balanced and unbalanced, involving chromosomal areas 1p11-13, 2q35-37, and 16q22-24. Interphase fluorescence in situ hybridization (IP-FISH) with probes specific for chromosome 7 has also been performed, revealing variable percentages of trisomy 7 [16,18,21].
In an attempt to further extend our knowledge about the genomic changes of these tumors, we decided to perform comparative genomic hybridization (CGH) and IP-FISH with probes specific for chromosomes 1, 5, and 7. The former type of analysis has never been performed on TSGCTs before. In addition, we present the karyotypes of three diffuse TSGCTs subjected to chromosome banding analysis. Because in colon cancer there is an association between a diploid tumor karyotype and an abundance of inflammatory cells, on one hand, and microsatellite instability, on the other hand [25], and because the former two features are also seen in TSGCT, we also chose to perform analysis of the microsatellite markers BAT25 and BAT26 to look for microsatellite instability [26,27].
Materials and Methods
Samples and Cytogenetics
Fifty-eight consecutive formalin-fixed, paraffin-embedded (FFPE) TSGCTs arriving at our hospital between 1998 and 2002 and two fresh frozen TSGCTs were obtained from the Department of Pathology. Fifty-one of the FFPE tumors were localized, whereas the remaining seven were of the diffuse type, as were also the two fresh frozen tumors. Thirty-seven of 60 (62%) tumor samples were from women, and 23 (38%) were from men. Seven tumors were recurrences and 53 were primary tumors. The median patient age at diagnosis was 44 years (range 14–77 years). For the subset of diffuse tumors, median patient age was 30 years, three of nine samples were recurrences, and five patients were male. Table 1 summarizes the clinical and molecular cytogenetic data on the 27 tumors analyzed by IP-FISH (see below).
Table 1.
Clinical and Molecular Cytogenetic Data on 27 TSGCTs.
| Sample Number | Subtype | Location | Recurrence | Sex | Age | CGH | Trisomy 7 (%) |
| 03-02 | L | Finger | F | 26 | Normal | 1 | |
| 05-02 | L | Hand | + | F | 71 | Normal | 3 |
| 06-02 | L | Finger | F | 27 | Normal | 3.5 | |
| 11-02 | L | Knee | F | 38 | Normal | 11 | |
| 12-02 | L | Finger | M | 77 | Normal | 6.5 | |
| 14-02 | L | Finger | M | 31 | Normal | 9 | |
| 18-02 | L | Finger | F | 59 | Normal | 8 | |
| 25-02 | L | Finger | F | 27 | Normal | 3 | |
| 26-02 | L | Hand | F | 41 | Normal | 5 | |
| 27-02 | L | Finger | M | 35 | Normal | 6.5 | |
| 28-02 | L | Hand | F | 53 | Normal | 5.5 | |
| 30-02 | L | Finger | F | 36 | Normal | 0 | |
| 31-02 | D | Knee | M | 15 | Normal | 5.5 | |
| 32-02 | L | Finger | M | 64 | Normal | 6 | |
| 33-02 | L | Ankle | M | 18 | Normal | 6.5 | |
| 35-02 | L | Finger | F | 35 | Normal | 1 | |
| 41-02 | L | Foot | + | M | 50 | Normal | 0 |
| 43-02 | L | Finger | F | 58 | Normal | 9.5 | |
| 48-02 | D | Hand | + | F | 36 | Normal | 8.5 |
| 53-02 | L | Finger | F | 41 | Normal | 2 | |
| 54-02 | D | Finger | + | F | 55 | Normal | 7 |
| 57-02 | L | Finger | M | 43 | Normal | 0 | |
| 59-02 | D | Knee | F | 14 | Normal | 7 | |
| R02-885 | D | Unknown | F | 20 | Normal | 0 | |
| 13-02 | D | Knee | M | 33 | ND | 1.5 | |
| 46-02 | D | Hand | + | M | 20 | ND | 3 |
| 52-02 | D | Knee | M | 28 | ND | 10.5 | |
L, localized; D, diffuse; +, recurrence; M, male; F, female; ND, not determined.
Trisomy 7 percentages in italics when more than 5% of the cells in a sample showed three signals for the chromosome 7-specific probe.
The two tumors that were surgically removed at The Norwegian Radium Hospital while the studies on archival material were in progress were processed for cytogenetic analysis. Fresh material was manually minced and treated with collagenase, hyaluronidase, and neuraminidase until a suitable suspension of cells and cell clumps was obtained. After 3 days of culturing in a medium consisting of RPMI 1640, 13% fetal calf serum, and antibiotics, colchicine was added for the last 4 hours and the short-term culture was harvested according to standard protocols [28]. The chromosomes in the dividing cells were then G-banded and a karyotype was established in accordance with the recommendations of the International System of Cytogenetic Nomenclature [29]. This procedure had also been carried out earlier on one of the FFPE tumors.
CGH
DNA was isolated by the phenol chloroform method as previously described [30]. Briefly, the tissue was deparaffinized in xylene, washed in alcohol, and digested in lysis buffer, proteinase K, and RNAse, followed by phenol chloroform extraction and ethanol precipitation. Metaphase target slides were prepared by dropping fixed cells from peripheral blood of a healthy person onto moist slides. The preparations were evaluated according to the following criteria: adequate chromosomal length, black color, minimal overlapping, minimal cytoplasm, and adequate number of mitoses [31]. Slides were stored at room temperature 1 to 4 weeks before use.
CGH was performed on 49 of 60 tumors as previously described [32–34], with minor modifications. For the remaining 11 tumors, no high-molecular-weight DNA (HMW-DNA) was obtained. Briefly, equal amounts of test and reference DNA were differentially labeled with fluorochrome-conjugated nucleotides, mixed together, denatured at 70°C for 5 minutes together with 33 µg of human cot-DNA, and then hybridized onto normal metaphase spreads that had been denatured for 3 minutes at 70°C to 73°C. The samples were then incubated at 37°C for 2 to 3 days. After washing, the slides were counterstained with an antifade solution consisting of 4′,6-diamino-2-phenylindole (DAPI) and Vectashields H-1200 (Vectashield; Vector Laboratories, Burlingame, CA), and examined in a fluorescence microscope (Zeiss Axioplan, Oberkochen, Germany). Single-color images [fluorescein isothiocyanate (FITC), Texas Red, and DAPI] of metaphase spreads were sequentially photographed with a Cohu 4900 CCD (12-bit gray scale) camera, using Cytovision hardware and software.
Chromosomes were karyotyped based on their inverted DAPI banding appearance. Fluorescence ratio profiles (green to red) were calculated for individual chromosomes, data from 11 to 20 representative copies of each chromosome were combined, and average ratio profiles with 95% confidence intervals were calculated for each tumor. The centromeric and pericentromeric heterochromatic regions were not evaluated. Poor hybridizations, mostly resulting from either suboptimal slide or DNA quality, were not accepted. One knows from karyotyping studies that TSGCTs are mostly diploid, and we therefore chose thresholds corresponding to loss or gain of one chromosome homologue in 50% of the cells analyzed (i.e., 0.75 and 1.25, respectively). To reduce the problem with potentially false-positive areas [32,33,35], we used a modified CGH protocol with a mixture of fluorochrome dUTP and dCTP during nick translation. Additionally, we also used a negative control in all experiments, and all tumor changes were evaluated against this control. Finally, the human colon cancer cell line lovo was used as a positive control in each experiment.
IP-FISH
Dual-color IP-FISH with α-satellite probes specific for chromosomes 1 and 7, and with a dual-color probe for chromosome arms 5p and 5q, was performed on 27 TSGCTs altogether. Directly labelled spectrum green and spectrum orange probes and appropriate hybridization and counterstaining solutions were supplied by Vysis (AH Diagnostics, Oslo, Norway). The tumors with informative CGH results and three of the other four diffuse TSGCTs were included; for the fourth one, no more material was available. The nuclei were extracted by a method modified from Liehr et al. [36]. Briefly, two to four 50-µm tissue sections were deparaffinized in xylene and washed in alcohol before rehydration. The preparations were then washed in phosphate-buffered saline (PBS), prewarmed protease (Sigma Protease XXIV; 0.5 mg/ml) in PBS was added, and the preparations were incubated in a shaking water bath for 1 hour at 37°C. The resulting cell suspensions were then pipetted vigorously to release nuclei, filtrated through a 60-µm nylon mesh, followed by centrifugation and washing in PBS. Finally, the nuclear suspension was spread on poly-l-lysine-coated slides using a cytospin centrifuge. The slides were left at room temperature for one night before freezing at -70°C or -20°C.
From the day before hybridization was begun, the slides were kept at room temperature and pretreated as described earlier with but minor modifications [37]. Briefly, the slides were treated with xylene in order to remove remaining paraffin, and washed in alcohol. The preparations were then boiled for 15 minutes in a microwave oven and cooled for 20 minutes at room temperature; both procedures took place with the slides immersed in sodium citrate. Finally, the slides were treated with variable concentrations of pepsin (P-7012; Sigma-Aldrich, Steinheim, Germany) for 5 to 13 minutes, washed in PBS, and dehydrated in alcohol.
For denaturation and hybridization of probes and slides, we used the following procedure [38]. The dehydrated slides were denatured in formamide at 73°C for 5 minutes, dehydrated again, and dried. The probes were denatured at 73°C for 5 minutes before application onto the slide. After 2 to 3 days of incubation at 37°C to 42°C, the slides were washed in formamide, 2 x standard saline citrate (2 x SSC), and 2 x SSC/0.1% NP-40. Then air drying was carried out before application of 10 µl of DAPI in antifade solution and sealing with a coverslip. Two hundred successive, whole, and single nuclei were examined in a Zeiss fluorescence microscope and images were captured using a Cohu camera. The specificity of the probe was validated by FISH experiments on slides with metaphases and interphase nuclei from a karyotypically normal person.
Cutoff levels for defining trisomy in IP-FISH studies vary in the literature, mostly from 5% to 10%. We chose to use 5% as the cutoff level based on findings on control slides and the results reached using chromosome 1-specific, chromosome arm 5p-specific, and chromosome arm 5q-specific probes; for none of them, more than 3.0% of the cells showed three signals. The probes for chromosomes 1 and 7 were cohybridized, and, in this way, the first of them served as an internal control.
Microsatellite Instability Analyses
Duplex polymerase chain reaction (PCR) analyses of two mononucleotide microsatellites (BAT25 and BAT26) were performed using a fluorescent-labeled forward primer and PCR conditions as described earlier [39]. The PCR products were separated by capillary electrophoresis on an ABI PRISM 310 Genetic Analyzer (PE Biosystems, Oslo, Norway). Because these microsatellites are quasimonomorphic, only tumor DNA was analyzed. Samples with a PCR product within the correct size range were considered informative.
Results
Samples and Cytogenetics
One of the three tumors subjected to G-banding analysis had a normal karyotype. The second tumor had a t(1;22) (p13;q12) in all 20 cells analyzed (Figure 1A), whereas the third tumor had a t(1;1)(q21;p11) in nine cells (Figure 1B), an unrelated clone with +7 as the only aberration in two cells, and 14 cells were normal. All three were of the diffuse type.
Figure 1.
(A) Partial karyotype from the diffuse TSGCT of case 46-02 showing normal chromosomes 1 and 22 paired up with the derivative chromosomes 1 and 22 resulting from the t(1;22)(p13;q12) that was the only chromosomal aberration of this case. (B) Partial karyotype from the diffuse TSGCT of case 59-02 showing the two copies of chromosome 1 resulting from a t(1;1)(q21;p11), the only structural chromosomal aberration of this case.
CGH
Eleven of 58 FFPE tumor samples did not yield any HMW-DNA at all, but 22 of the remaining 47 FFPE TSGCTs could be analyzed by CGH, as were the two fresh frozen TSGCTs. Nineteen of the successfully analyzed tumors were localized. All genomic profiles were normal. For 25 of the TSGCTs, the hybridizations were not satisfactory, and these tumors were therefore not analyzed by CGH.
IP-FISH
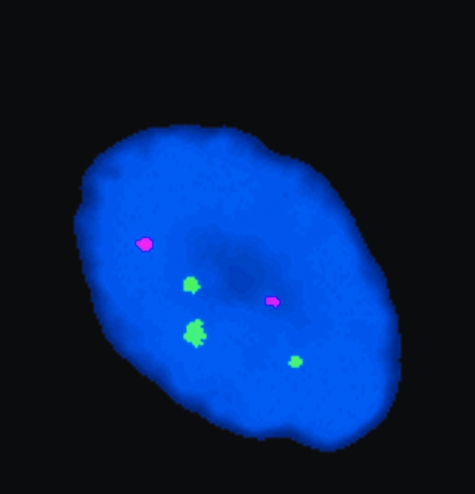
Trisomy 7 was detected in 15 of 27 samples (56%) as analyzed by IP-FISH (Figure 2, Table 1). There was no striking difference between localized and diffuse tumors, as five of eight (63%) diffuse tumors and 10 of 19 (53%) localized tumors exhibited trisomy 7. Three signals for chromosome 1 and chromosome arms 5p and 5q were detected in 0% to 2.5%, 0% to 3%, and 0% to 3% of the cells in each sample, respectively. As this is below our cutoff limit, no trisomies for these probes were detected.
Figure 2.
IP-FISH image from case 14-02 showing three signals for the FITC-labeled (green) chromosome 7-specific probe and two signals for the Texas Red-labeled (red) chromosome 1-specific probe.
Microsatellite Instability Analyses
Fifty-two of the tumors were wild-type for BAT25; for the remaining eight tumors, the analyses were not successful. The corresponding numbers for BAT26 were 53 wild-type tumors and seven tumors with unsuccessful analysis.
Discussion
Based on earlier studies by others and from our own previous work with CGH on FFPE material, we know that the success rate is fairly low but variable [30,40,41]. The reasons for this are, first and foremost, the problems associated with degraded DNA and parameters relevant to the fixation process, the time the samples spent in fixative, and the composition of the fixation fluid. All tumors in the present series were routinely treated in buffered formalin. For the 11 TSGCTs that yielded no HMW-DNA, it was of course impossible to proceed with CGH. For the 25 tumors with some HMW-DNA but which nevertheless gave no satisfactory hybridization by CGH, we can only speculate that they had spent a relatively long time in formalin because we have no specific information for individual samples regarding this matter.
The pathogenetic mechanism(s) of TSGCTs has been debated much, as has the nosologic position and subgrouping of this imprecisely defined entity. The confusing terminology reflects this state of affairs: some names imply an inflammatory pathogenesis (itis), others a neoplastic one (tumor). Additionally, the distinction between diffuse and localized and/or between extraarticular and intraarticular lesions is not always precise. Some authors tend to see the lesions as histopathologically similar but clinically distinct [10], whereas others regard them as one disease entity [3,42].
We included 60 consecutive TSGCTs in our study, 51 of them of the localized type. Most patients were in the age group 25 to 60 years, and most of them were women, which is in accordance with known incidence data [2]. In previous studies [1,16–24], 26 of 33 hitherto karyotyped diffuse TSGCTs have been demonstrated to carry clonal chromosomal aberrations, whereas the corresponding number for localized tumors is 15 of 23 [1,22]. We now add karyotypic data on three diffuse TSGCTs: one normal, one demonstrating a t(1;22)(p13;q12) as the sole chromosomal change, and one exhibiting a t(1;1)(q21;p11) in nine cells and an unrelated clone with +7 as the only aberration in another two cells. 1p11-13 is the chromosomal region most frequently involved in structural rearrangements in TSGCTs, together with different translocation partners [1,22]. 22q12 and 1q21 have not been reported rearranged together with 1p11-13 in TSGCTs before. How the observed translocations might act pathogenetically is unknown.
Because acquired genomic abnormalities are a hallmark of neoplastic cells and because the nature of TSGCT is still debated, we decided it was of interest to screen the genome of these disease lesions by chromosomal CGH to look for loss or gain of genetic material. It is important to remember that this method is unable to detect balanced rearrangements, some of which have been found by karyotyping in TSGCTs. Another limitation of the technique is that it only detects changes present in many cells in a sample, and one should keep in mind that TSGCTs contain a considerable admixture of many different cell types. If a neoplastic parenchyma exists in TSGCTs, it is therefore severely diluted by other elements. Finally, small deletions and gains (<10 Mb) are not detectable by chromosomal CGH. All these aspects are important for the interpretation of the results. Obviously, the fact that all analyzable samples were normal by CGH does not argue for a neoplastic origin of TSGCTs, but it does not strongly contradict it either, given the aforementioned limitations.
Nor did the microsatellite analyses shed much light on the pathogenetic process of TSGCT because all informative tumors were wild-type for both BAT25 and BAT26. Nevertheless, this negative finding makes the possibility of microsatellite instability as a major contributing pathogenetic mechanism in TSGCT unlikely.
There are some issues regarding our IP-FISH analyses that need to be addressed. First, there are different cell types in TSGCTs, and when we extract nuclei, all types of cells/nuclei are treated the same. Because at least some of these cells supposedly are nonneoplastic, the findings by IP-FISH are correspondingly diluted, as it is impossible to know which type of cell any individual nucleus represents. Second, we were not able to perform investigations of chromosomes 5 and 7 on the same cells. However, this fact cannot affect the actual frequencies of trisomies detected.
The IP-FISH results for chromosome 7 were of considerable interest. In previous studies, only diffuse TSGCTs have been examined with chromosome 7-specific probes to check for trisomy 7, the most frequent numerical aberration found by karyotyping in these tumors, as it has been found in 8 of 26 (31%) aberrant cases [43]. Trisomy 7 percentages between 3.0% and 26.5% were seen [16], and +7 could also be found by IP-FISH in cases which by karyotyping had been normal [21]. We examined both diffuse and localized TSGCTs, finding similar frequencies of trisomy 7 in both. In total, 56% of TSGCTs (15 of 27) exhibited trisomy 7 at frequencies from 5.0% to 11% of all cells. Our results thus confirm that trisomy 7 is a common aberration in TSGCT and also show that there is no difference between diffuse and localized disease in this regard.
Trisomy 7 is a controversial aberration in cancer cytogenetics as it can sometimes be found also in nonneoplastic disease lesions and in normal tissues [44], underscoring that the acquisition of somatic mutations is not always sufficient to unleash neoplastic behavior by the cells harboring them. It has been speculated that inflammatory cells may be more prone to acquire +7 than other cell types and that this could be the reason behind the finding of trisomy 7 also in chronic inflammatory lesions [44]. Also many other studies and reviews [17,21,45] have concluded that trisomy 7 may be found in a number of inflammatory conditions including different types of synovitis, both in vitro and in vivo, and cells with +7 are suggested to have a polyclonal origin and a proliferative advantage in vitro in some of these cases [17]. It has been proposed that trisomy 7 might be a result of local inflammatory mechanisms [46] and that the aberration reflects an intermediate state between self-limiting inflammation and neoplastic transformation. Furthermore, the frequency of +7 has been reported to increase with age in both nonneoplastic synovia and solid tumors, often as the sole change in nonneoplastic tissue [47]. This was not markedly so in the present study, in which the mean patient age for trisomy 7-positive samples was about the same as the mean age for the total sample material (42 vs 44 years), whereas the mean age for the +7-negative samples was only 36 years. At the same time, trisomy 7 has also been reported as an early imbalance in many neoplasms, presumably signifying an important early event in the development of some tumors [48]. In conclusion, therefore, our finding of trisomy 7 by IP-FISH in TSGCTs can be interpreted as conclusive support for neither the neoplastic nor the inflammatory theory of pathogenesis. This is particularly so when we consider that trisomy 7 was the only registered chromosomal abnormality in this series, making its information value in this regard even more uncertain.
Acknowledgements
We thank Lisbeth Haugom, Kristin Andersen, and Nadja Urban for expert technical assistance. This work was supported by the Norwegian Cancer Society.
Abbreviations
- CGH
comparative genomic hybridization
- FFPE
formalin-fixed, paraffin-embedded
- HMW-DNA
high-molecular-weight DNA
- IP-FISH
interphase fluorescence in situ hybridization
- TSGCT
tenosynovial giant cell tumor
- DAPI
4′,6-diamino-2-phenylindole
- FITC
fluorescein isothiocyanate
References
- 1.Sciot R, Rosai J, Dal Cin P, De WI, Fletcher CD, Mandahl N, Mertens F, Mitelman F, Rydholm A, Tallini G, den Van BH, Vanni R, Willen H. Analysis of 35 cases of localized and diffuse tenosynovial giant cell tumor: a report from the Chromosomes and Morphology (CHAMP) study group. Mod Pathol. 1999;12:576–579. [PubMed] [Google Scholar]
- 2.Weiss SW, Goldblum JR. Enzinger and Weiss's Soft Tissue Tumors. 4th ed. St. Louis: Mosby; 2001. [Google Scholar]
- 3.Jaffe HL, Lichtenstein L, Sutro CJ. Pigmented villonodular synovitis, bursitis and tenosynovitis. A discussion of the synovial and bursal equivalents of the tenosynovial lesion commonly denoted as xanthoma, xanthogranuloma, giant cell tumor or myeloplaxoma of the tendon sheath, with some consideration of this tendon sheath lesion itself. Arch Pathol. 1941;31:731–764. [Google Scholar]
- 4.Somerhausen NS, Dal Cin P. WHO classification of tumours. Pathology and genetics of tumours of soft tissue and bone. In: Fletcher KK, Unni KK, Mertens F, editors. So-Called Fibrohistiocytic Tumours. Lyon: IARC; 2002. pp. 110–114. [Google Scholar]
- 5.Kempson RL, Fletcher CDM, Evans HL, Hendrickson MR, Sibley RK. Atlas of Tumor Pathology. Bethesda: Tumors of the Soft Tissues Armed Forces Institute of Pathology; 2001. [Google Scholar]
- 6.Vogrincic GS, O'Connell JX, Gilks CB. Giant cell tumor of tendon sheath is a polyclonal cellular proliferation. Hum Pathol. 1997;28:815–819. doi: 10.1016/s0046-8177(97)90155-6. [DOI] [PubMed] [Google Scholar]
- 7.Sakkers RJ, de Jong D, van der Heul RO. X-chromosome inactivation in patients who have pigmented villonodular synovitis. J Bone Jt Surg Am. 1991;73:1532–1536. [PubMed] [Google Scholar]
- 8.Singh R, Grewal DS, Chakravarti RN. Experimental production of pigmented villonodular synovitis in the knee and ankle joints of rhesus monkeys. J Pathol. 1969;98:137–142. doi: 10.1002/path.1710980207. [DOI] [PubMed] [Google Scholar]
- 9.Choong PF, Willen H, Nilbert M, Mertens F, Mandahl N, Carlen B, Rydholm A. Pigmented villonodular synovitis. Monoclonality and metastasis—a case for neoplastic origin? Acta Orthop Scand. 1995;66:64–68. doi: 10.3109/17453679508994643. [DOI] [PubMed] [Google Scholar]
- 10.Abdul-Karim FW, el Naggar AK, Joyce MJ, Makley JT, Carter JR. Diffuse and localized tenosynovial giant cell tumor and pigmented villonodular synovitis: a clinicopathologic and flow cytometric DNA analysis. Hum Pathol. 1992;23:729–735. doi: 10.1016/0046-8177(92)90340-9. [DOI] [PubMed] [Google Scholar]
- 11.Carstens PHB, Howell RS. Malignant giant cell tumor of tendon sheath. Virchows Arch A. 1979;243:237–243. doi: 10.1007/BF01102878. [DOI] [PubMed] [Google Scholar]
- 12.Kahn LB. Malignant giant cell tumor of the tendon sheath. Ultra-structural study and review of the literature. Arch Pathol. 1973;95:203–208. [PubMed] [Google Scholar]
- 13.Nielsen AL, Kiaer T. Malignant giant cell tumor of synovium and locally destructive pigmented villonodular synovitis: ultrastructural and immunohistochemical study and review of the literature. Hum Pathol. 1989;20:765–771. doi: 10.1016/0046-8177(89)90070-1. [DOI] [PubMed] [Google Scholar]
- 14.Bertoni F, Unni KK, Beabout JW, Sim FH. Malignant giant cell tumor of the tendon sheaths and joints (malignant pigmented villonodular synovitis) Am J Surg Pathol. 1997;21:153–163. doi: 10.1097/00000478-199702000-00004. [DOI] [PubMed] [Google Scholar]
- 15.Layfield LJ, Meloni-Ehrig A, Liu K, Shepard R, Harrelson JM. Malignant giant cell tumor of synovium (malignant pigmented villonodular synovitis) Arch Pathol Lab Med. 2000;124:1636–1641. doi: 10.5858/2000-124-1636-MGCTOS. [DOI] [PubMed] [Google Scholar]
- 16.Fletcher JA, Henkle C, Atkins L, Rosenberg AE, Morton CC. Trisomy 5 and trisomy 7 are nonrandom aberrations in pigmented villonodular synovitis: confirmation of trisomy 7 in uncultured cells. Genes Chromosomes Cancer. 1992;4:264–266. doi: 10.1002/gcc.2870040312. [DOI] [PubMed] [Google Scholar]
- 17.Mertens F, Örndal C, Mandahl N, Heim S, Bauer HF, Rydholm A, Tufvesson A, Willén H, Mitelman F. Chromosome aberrations in tenosynovial giant cell tumors and nontumorous synovial tissue. Genes Chromosomes Cancer. 1993;6:212–217. doi: 10.1002/gcc.2870060404. [DOI] [PubMed] [Google Scholar]
- 18.Ohjimi Y, Iwasaki H, Ishiguro M, Kaneko Y, Tashiro H, Emoto G, Ogata K, Kikuchi M. Short arm of chromosome 1 aberration recurrently found in pigmented villonodular synovitis. Cancer Genet Cytogenet. 1996;90:80–85. doi: 10.1016/0165-4608(96)00064-7. [DOI] [PubMed] [Google Scholar]
- 19.Rowlands CG, Roland B, Hwang WS, Sevick RJ. Diffuse-variant tenosynovial giant cell tumor: a rare and aggressive lesion. Hum Pathol. 1994;25:423–425. doi: 10.1016/0046-8177(94)90154-6. [DOI] [PubMed] [Google Scholar]
- 20.Gonzalez-Campora R, Salas HE, Otal-Salaverri CV, San MD, Hevia VA, Galera DH. Diffuse tenosynovial giant cell tumor of soft tissues. Report of a case with cytologic and cytogenetic findings. Acta Cytol. 1995;39:770–776. [PubMed] [Google Scholar]
- 21.Dahlen A, Broberg K, Domanski HA, Toksvig-Larsen S, Lindstrand A, Mandahl N, Mertens F. Analysis of the distribution and frequency of trisomy 7 in vivo in synovia from patients with osteoarthritis and pigmented villonodular synovitis. Cancer Genet Cytogenet. 2001;131:19–24. doi: 10.1016/s0165-4608(01)00488-5. [DOI] [PubMed] [Google Scholar]
- 22.Nilsson M, Höglund M, Panagopoulos I, Sciot R, Dal Cin P, Debiec-Rychter M, Mertens F, Mandahl N. Molecular cytogenetic mapping of recurrent chromosomal breakpoints in tenosynovial giant cell tumors. Virchows Arch. 2002;441:475–480. doi: 10.1007/s00428-002-0640-y. [DOI] [PubMed] [Google Scholar]
- 23.Ray RA, Morton CC, Lipinski KK, Corson JM, Fletcher JA. Cytogenetic evidence of clonality in a case of pigmented villonodular synovitis. Cancer. 1991;67:121–125. doi: 10.1002/1097-0142(19910101)67:1<121::aid-cncr2820670122>3.0.co;2-p. [DOI] [PubMed] [Google Scholar]
- 24.Ferrer J, Namiq A, Carda C, Lopez-Gines C, Tawfik O, Llombart-Bosch A. Diffuse type of giant-cell tumor of tendon sheath: an ultrastructural study of two cases with cytogenetic support. Ultrastruct Pathol. 2002;26:15–21. doi: 10.1080/01913120252934288. [DOI] [PubMed] [Google Scholar]
- 25.Ilyas M, Straub J, Tomlinson IP, Bodmer WF. Genetic pathways in colorectal and other cancers. Eur J Cancer. 1999;35:1986–2002. doi: 10.1016/s0959-8049(99)00298-1. [DOI] [PubMed] [Google Scholar]
- 26.Hoang JM, Cottu PH, Thuille B, Salmon RJ, Thomas G, Hamelin R. BAT-26, an indicator of the replication error phenotype in colorectal cancers and cell lines. Cancer Res. 1997;57:300–303. [PubMed] [Google Scholar]
- 27.Zhou XP, Hoang JM, Li YJ, Seruca R, Carneiro F, Sobrinho-Simoes M, Lothe RA, Gleeson CM, Russell SE, Muzeau F, Flejou JF, Hoang-Xuan K, Lidereau R, Thomas G, Hamelin R. Determination of the replication error phenotype in human tumors without the requirement for matching normal DNA by analysis of mononucleotide repeat microsatellites. Genes Chromosomes Cancer. 1998;21:101–107. doi: 10.1002/(sici)1098-2264(199802)21:2<101::aid-gcc4>3.0.co;2-4. [DOI] [PubMed] [Google Scholar]
- 28.Mandahl N. In: Human Cytogenetics—A Practical Approach: Vol. II. Malignancy and Acquired Abnormalities. Rooney DE, Czepulkowski H, editors. Oxford: IRL Press; 1992. pp. 155–187. [Google Scholar]
- 29.ISCN H, author. An International System for Human Cytogenetic Nomenclature. Basel, Switzerland: S. Karger AG; 1995. [Google Scholar]
- 30.Brandal P, Micci F, Bjerkehagen B, Eknaes M, Larramendy M, Lothe RA, Knuutila S, Heim S. Molecular cytogenetic characterization of desmoid tumors. Cancer Genet Cytogenet. 2003;146:1–7. doi: 10.1016/s0165-4608(03)00122-5. [DOI] [PubMed] [Google Scholar]
- 31.Karhu R, Kahkonen M, Kuukasjarvi T, Pennanen S, Tirkkonen M, Kallioniemi O. Quality control of CGH: impact of metaphase chromosomes and the dynamic range of hybridization. Cytometry. 1997;28:198–205. doi: 10.1002/(sici)1097-0320(19970701)28:3<198::aid-cyto3>3.0.co;2-a. [DOI] [PubMed] [Google Scholar]
- 32.Kallioniemi A, Kallioniemi OP, Sudar D, Rutovitz D, Gray JW, Waldman F, Pinkel D. Comparative genomic hybridization for molecular cytogenetic analysis of solid tumors. Science. 1992;258:818–821. doi: 10.1126/science.1359641. [DOI] [PubMed] [Google Scholar]
- 33.Kallioniemi OP, Kallioniemi A, Piper J, Isola J, Waldman FM, Gray JW, Pinkel D. Optimizing comparative genomic hybridization for analysis of DNA sequence copy number changes in solid tumors. Genes Chromosomes Cancer. 1994;10:231–243. doi: 10.1002/gcc.2870100403. [DOI] [PubMed] [Google Scholar]
- 34.Kraggerud SM, Szymanska J, Abeler VM, Kaern J, Eknaes M, Heim S, Teixeira MR, Trope CG, Peltomäki P, Lothe RA. DNA copy number changes in malignant ovarian germ cell tumors. Cancer Res. 2000;60:3025–3030. [PubMed] [Google Scholar]
- 35.el Rifai W, Larramendy ML, Bjorkqvist AM, Hemmer S, Knuutila S. Optimization of comparative genomic hybridization using fluorochrome conjugated to dCTP and dUTP nucleotides. Lab Invest. 1997;77:699–700. [PubMed] [Google Scholar]
- 36.Liehr T, Grehl H, Rautenstrauss B. FISH analysis of interphase nuclei extracted from paraffin-embedded tissue. Trends Genet. 1995;11:377–378. doi: 10.1016/s0168-9525(00)89113-1. [DOI] [PubMed] [Google Scholar]
- 37.Knuutila S, Nylund SJ, Wessman M, Larramendy ML. Analysis of genotype and phenotype on the same interphase or mitotic cell. A manual of MAC (morphology antibody chromosomes) methodology. Cancer Genet Cytogenet. 1994;72:1–15. doi: 10.1016/0165-4608(94)90102-3. [DOI] [PubMed] [Google Scholar]
- 38.Persons DL, Hartmann LC, Herath JF, Borell TJ, Cliby WA, Keeney GL, Jenkins RB. Interphase molecular cytogenetic analysis of epithelial ovarian carcinomas. Am J Pathol. 1993;142:733–741. [PMC free article] [PubMed] [Google Scholar]
- 39.Thorstensen L, Diep CB, Meling GI, Aagesen TH, Ahrens CH, Rognum TO, Lothe RA. WNT1 inducible signaling pathway protein 3, WISP-3, a novel target gene in colorectal carcinomas with microsatellite instability. Gastroenterology. 2001;121:1275–1280. doi: 10.1053/gast.2001.29570. [DOI] [PubMed] [Google Scholar]
- 40.Køsel S, Grasbon-Frodl EM, Arima K, Chimelli L, Hahn M, Hashizume Y, Hulette C, Ikeda K, Jacobsen PF, Jones M, Kobayashi M, Love S, Mizutani T, Rosemberg S, Sasaki A, Smith TW, Takahashi H, Vortmeyer AO, Graeber MB. Inter-laboratory comparison of DNA preservation in archival paraffin-embedded human brain tissue from participating centres on four continents. Neurogenetics. 2001;3:163–170. doi: 10.1007/s100480100114. [DOI] [PubMed] [Google Scholar]
- 41.Isola J, DeVries S, Chu L, Ghazvini S, Waldman F. Analysis of changes in DNA sequence copy number by comparative genomic hybridization in archival paraffin-embedded tumor samples. Am J Pathol. 1994;145:1301–1308. [PMC free article] [PubMed] [Google Scholar]
- 42.Somerhausen NS, Fletcher CD. Diffuse-type giant cell tumor: clinicopathologic and immunohistochemical analysis of 50 cases with extraarticular disease. Am J Surg Pathol. 2000;24:479–492. doi: 10.1097/00000478-200004000-00002. [DOI] [PubMed] [Google Scholar]
- 43.Mitelman F, Johansson B, Mertens F, editors. Mitelman Database of Chromosome Aberrations in Cancer. 2004. [4-2-2004]. http://cgap.nci.nih.gov/Chromosomes/Mitelman.
- 44.Johansson B, Heim S, Mandahl N, Mertens F, Mitelman F. Trisomy 7 in nonneoplastic cells. Genes Chromosomes Cancer. 1993;6:199–205. doi: 10.1002/gcc.2870060402. [DOI] [PubMed] [Google Scholar]
- 45.Broberg K, Höglund M, Lindstrand A, Toksvig-Larsen S, Mandahl N, Mertens F. Polyclonal expansion of cells with trisomy 7 in synovia from patients with osteoarthritis. Cytogenet Cell Genet. 1998;83:30–34. doi: 10.1159/000015160. [DOI] [PubMed] [Google Scholar]
- 46.Kinne RW, Kunisch E, Beensen V, Zimmermann T, Emmrich F, Petrow P, Lungershausen W, Hein G, Braun RK, Foerster M, Kroegel C, Winter R, Liesaus E, Fuhrmann RA, Roth A, Claussen U, Liehr T. Synovial fibroblasts and synovial macrophages from patients with rheumatoid arthritis and other inflammatory joint diseases show chromosomal aberrations. Genes Chromosomes Cancer. 2003;38:53–67. doi: 10.1002/gcc.10242. [DOI] [PubMed] [Google Scholar]
- 47.Broberg K, Toksvig-Larsen S, Lindstrand A, Mertens F. Trisomy 7 accumulates with age in solid tumors and non-neoplastic synovia. Genes Chromosomes Cancer. 2001;30:310–315. [PubMed] [Google Scholar]
- 48.Höglund M, Gisselsson D, Säll T, Mitelman F. Coping with complexity multivariate analysis of tumor karyotypes. Cancer Genet Cytogenet. 2002;135:103–109. doi: 10.1016/s0165-4608(01)00645-8. [DOI] [PubMed] [Google Scholar]