Abstract
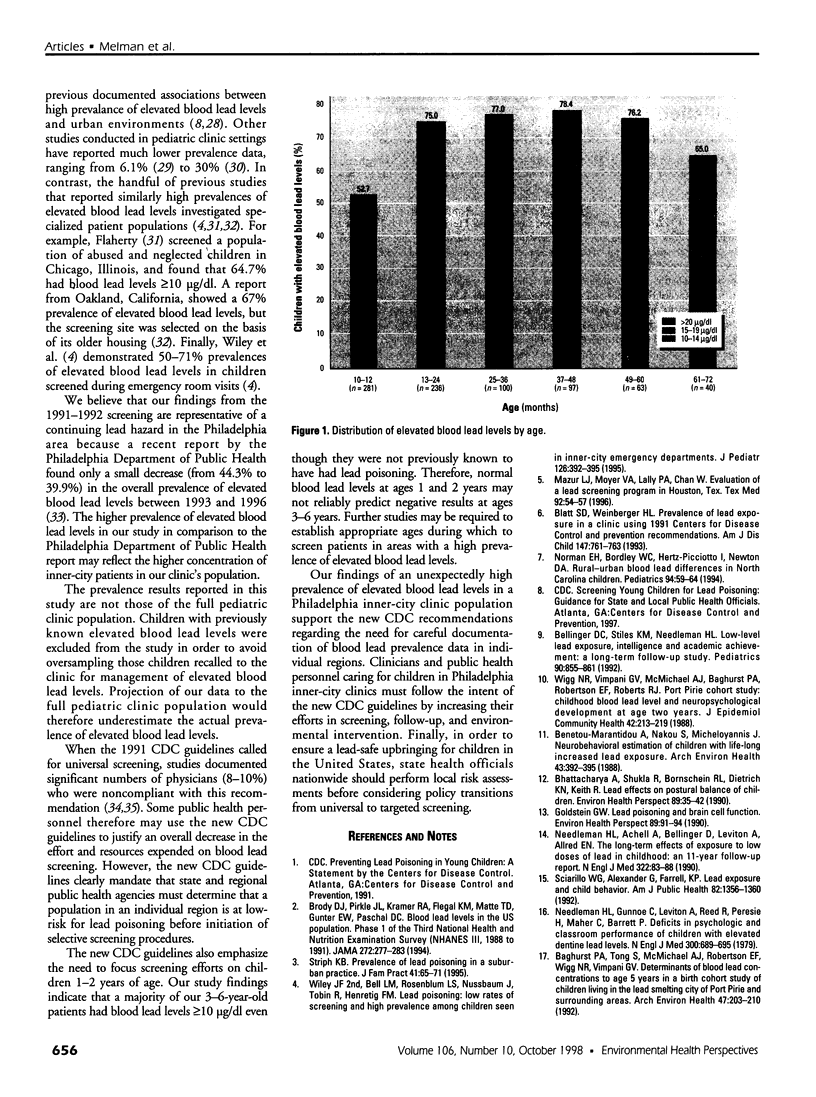
In November 1997, the Centers for Disease Control and Prevention (CDC) released revised guidelines for lead poisoning screening, including a recommendation that states and regions individualize screening policies based on local prevalence of elevated lead levels. The purpose of this study was to collect prevalence data for a Philadelphia, Pennsylvania, inner-city pediatric outpatient population previously not known to have elevated blood lead levels in order to determine its risk for lead exposure and screening requirements. Charts were reviewed for 817 children of 10 months through 6 years of age whose venous blood lead levels were obtained as part of their routine health care over a 12-month period ending October 1992. None of these children had a history of previously elevated lead levels. Prevalence of elevated lead levels was determined for this population and correlated with patient age, sex, race, and insurance type. More than two-thirds (68%) of the study patients had a blood lead level of [Greater than and equal to]10 microg/dl. Elevated blood lead levels were associated with black race (p<0.0001), but not with sex or insurance type. The percentage of children with elevated blood lead levels was highest at ages 37-48 months. A majority of the children screened had lead levels in excess of the CDC threshold for an abnormal lead level (10 microgram/dl). This is the highest reported prevalence within a U.S. pediatric clinic population. In view of this extremely high prevalence, clinicians and public health personnel caring for children in Philadelphia inner-city clinics must follow the intent of the new CDC guidelines by increasing their efforts in the areas of screening, follow-up, and environmental interventions. To ensure a lead-safe upbringing for children in the United States, state health officials nationwide should perform local risk assessments before considering policy transitions from universal to targeted screening.
Full text
PDF
Images in this article
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Baghurst P. A., Tong S. L., McMichael A. J., Robertson E. F., Wigg N. R., Vimpani G. V. Determinants of blood lead concentrations to age 5 years in a birth cohort study of children living in the lead smelting city of Port Pirie and surrounding areas. Arch Environ Health. 1992 May-Jun;47(3):203–210. doi: 10.1080/00039896.1992.9938350. [DOI] [PubMed] [Google Scholar]
- Bellinger D. C., Stiles K. M., Needleman H. L. Low-level lead exposure, intelligence and academic achievement: a long-term follow-up study. Pediatrics. 1992 Dec;90(6):855–861. [PubMed] [Google Scholar]
- Bellinger D., Leviton A., Waternaux C., Needleman H., Rabinowitz M. Longitudinal analyses of prenatal and postnatal lead exposure and early cognitive development. N Engl J Med. 1987 Apr 23;316(17):1037–1043. doi: 10.1056/NEJM198704233161701. [DOI] [PubMed] [Google Scholar]
- Bellinger D., Sloman J., Leviton A., Rabinowitz M., Needleman H. L., Waternaux C. Low-level lead exposure and children's cognitive function in the preschool years. Pediatrics. 1991 Feb;87(2):219–227. [PubMed] [Google Scholar]
- Benetou-Marantidou A., Nakou S., Micheloyannis J. Neurobehavioral estimation of children with life-long increased lead exposure. Arch Environ Health. 1988 Nov-Dec;43(6):392–395. doi: 10.1080/00039896.1988.9935856. [DOI] [PubMed] [Google Scholar]
- Bhattacharya A., Shukla R., Bornschein R. L., Dietrich K. N., Keith R. Lead effects on postural balance of children. Environ Health Perspect. 1990 Nov;89:35–42. doi: 10.1289/ehp.908935. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blatt S. D., Weinberger H. L. Prevalence of lead exposure in a clinic using 1991 Centers for Disease Control and Prevention recommendations. Am J Dis Child. 1993 Jul;147(7):761–763. doi: 10.1001/archpedi.1993.02160310063019. [DOI] [PubMed] [Google Scholar]
- Brody D. J., Pirkle J. L., Kramer R. A., Flegal K. M., Matte T. D., Gunter E. W., Paschal D. C. Blood lead levels in the US population. Phase 1 of the Third National Health and Nutrition Examination Survey (NHANES III, 1988 to 1991) JAMA. 1994 Jul 27;272(4):277–283. doi: 10.1001/jama.272.4.277. [DOI] [PubMed] [Google Scholar]
- Campbell J. R., Schaffer S. J., Szilagyi P. G., O'Connor K. G., Briss P., Weitzman M. Blood lead screening practices among US pediatricians. Pediatrics. 1996 Sep;98(3 Pt 1):372–377. [PubMed] [Google Scholar]
- Casey R., Wiley C., Rutstein R., Pinto-Martin J. Prevalence of lead poisoning in an urban cohort of infants with high socioeconomic status. Clin Pediatr (Phila) 1994 Aug;33(8):480–484. doi: 10.1177/000992289403300806. [DOI] [PubMed] [Google Scholar]
- Dietrich K. N., Krafft K. M., Bornschein R. L., Hammond P. B., Berger O., Succop P. A., Bier M. Low-level fetal lead exposure effect on neurobehavioral development in early infancy. Pediatrics. 1987 Nov;80(5):721–730. [PubMed] [Google Scholar]
- Ferguson S. C., Lieu T. A. Blood lead testing by pediatricians: practice, attitudes, and demographics. Am J Public Health. 1997 Aug;87(8):1349–1351. doi: 10.2105/ajph.87.8.1349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Flaherty E. G. Risk of lead poisoning in abused and neglected children. Clin Pediatr (Phila) 1995 Mar;34(3):128–132. doi: 10.1177/000992289503400302. [DOI] [PubMed] [Google Scholar]
- Goldstein G. W. Lead poisoning and brain cell function. Environ Health Perspect. 1990 Nov;89:91–94. doi: 10.1289/ehp.908991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hunter J. M. The summer disease. An integrative model of the seasonality aspects of childhood lead poisoning. Soc Sci Med. 1977 Nov;11(14-16):691–703. doi: 10.1016/0037-7856(77)90155-x. [DOI] [PubMed] [Google Scholar]
- Hunter J. M. The summer disease. Some field evidence on seasonality in childhood lead poisoning. Soc Sci Med. 1978 Jun;12(2D):85–94. doi: 10.1016/0037-7856(78)90002-1. [DOI] [PubMed] [Google Scholar]
- Mazur L. J., Moyer V. A., Lally P. A., Chan W. Evaluation of a lead screening program in Houston, Tex. Tex Med. 1996 Jan;92(1):54–57. [PubMed] [Google Scholar]
- McMichael A. J., Baghurst P. A., Wigg N. R., Vimpani G. V., Robertson E. F., Roberts R. J. Port Pirie Cohort Study: environmental exposure to lead and children's abilities at the age of four years. N Engl J Med. 1988 Aug 25;319(8):468–475. doi: 10.1056/NEJM198808253190803. [DOI] [PubMed] [Google Scholar]
- Mielke H. W., Dugas D., Mielke P. W., Jr, Smith K. S., Gonzales C. R. Associations between soil lead and childhood blood lead in urban New Orleans and rural Lafourche Parish of Louisiana. Environ Health Perspect. 1997 Sep;105(9):950–954. doi: 10.1289/ehp.97105950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Needleman H. L., Bellinger D. The health effects of low level exposure to lead. Annu Rev Public Health. 1991;12:111–140. doi: 10.1146/annurev.pu.12.050191.000551. [DOI] [PubMed] [Google Scholar]
- Needleman H. L., Gatsonis C. A. Low-level lead exposure and the IQ of children. A meta-analysis of modern studies. JAMA. 1990 Feb 2;263(5):673–678. [PubMed] [Google Scholar]
- Needleman H. L., Gunnoe C., Leviton A., Reed R., Peresie H., Maher C., Barrett P. Deficits in psychologic and classroom performance of children with elevated dentine lead levels. N Engl J Med. 1979 Mar 29;300(13):689–695. doi: 10.1056/NEJM197903293001301. [DOI] [PubMed] [Google Scholar]
- Needleman H. L., Schell A., Bellinger D., Leviton A., Allred E. N. The long-term effects of exposure to low doses of lead in childhood. An 11-year follow-up report. N Engl J Med. 1990 Jan 11;322(2):83–88. doi: 10.1056/NEJM199001113220203. [DOI] [PubMed] [Google Scholar]
- Norman E. H., Bordley W. C., Hertz-Picciotto I., Newton D. A. Rural-urban blood lead differences in North Carolina children. Pediatrics. 1994 Jul;94(1):59–64. [PubMed] [Google Scholar]
- Sciarillo W. G., Alexander G., Farrell K. P. Lead exposure and child behavior. Am J Public Health. 1992 Oct;82(10):1356–1360. doi: 10.2105/ajph.82.10.1356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Snyder D. C., Mohle-Boetani J. C., Palla B., Fenstersheib M. Development of a population-specific risk assessment to predict elevated blood lead levels in Santa Clara County, California. Pediatrics. 1995 Oct;96(4 Pt 1):643–648. [PubMed] [Google Scholar]
- Wigg N. R., Vimpani G. V., McMichael A. J., Baghurst P. A., Robertson E. F., Roberts R. J. Port Pirie Cohort study: childhood blood lead and neuropsychological development at age two years. J Epidemiol Community Health. 1988 Sep;42(3):213–219. doi: 10.1136/jech.42.3.213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wiley J. F., 2nd, Bell L. M., Rosenblum L. S., Nussbaum J., Tobin R., Henretig F. M. Lead poisoning: low rates of screening and high prevalence among children seen in inner-city emergency departments. J Pediatr. 1995 Mar;126(3):392–395. doi: 10.1016/s0022-3476(95)70455-8. [DOI] [PubMed] [Google Scholar]