Abstract
Despite the increased number of anthrax outbreaks in Georgia and the other Caucasian republics of the former Soviet Union, no data are available on the diversity of the Bacillus anthracis strains involved. There is also little data available on strains from the former Soviet Union, including the strains previously used for vaccine preparation. In this study we used eight-locus variable-number tandem repeat analyses to genotype 18 strains isolated from infected animals and humans at different sites across Georgia, where anthrax outbreaks have occurred in the last 10 years, and 5 strains widely used for preparation of human and veterinary vaccines in the former Soviet Union. Three different genotypes affiliated with the A3.a cluster were detected for the Georgian isolates. Two genotypes were previously shown to include Turkish isolates, indicating that there is a regional strain pattern in the South Caucasian-Turkish region. Four of the vaccine strains were polymorphic, exhibiting three different patterns of the cluster A1.a genotype and the cluster A3.b genotype. The genotype of vaccine strain 71/12, which is considered an attenuated strain in spite of the presence of both of the virulence pXO plasmids, appeared to be a novel genotype in the A1.a cluster.
Bacillus anthracis, a spore-forming, gram-positive, rod-shaped, pathogenic bacterium found throughout the world, is the causative agent of anthrax in mammals. Outbreaks occur in both wild animals and domestic livestock, and recent dramatic events have shown that this bacterium can also be used in bioterrorist attacks. Anthrax remains an endemic disease worldwide and still has the potential to have a significant impact on public health (3, 16, 18, 22).
In recent years efforts to evaluate the diversity of B. anthracis isolates from different geographic areas improved our knowledge of the distribution of this species throughout the world (3, 8, 9, 14, 18, 22, 25). These studies were also undertaken to trace strains deliberately released into the environment back to their origins (10, 15). Most of these studies took advantage of multiple-locus variable-number tandem repeat (VNTR) analysis (MLVA) (14), which is recognized as the “gold standard” for molecular typing of B. anthracis strains. MLVA is based on analysis of VNTRs in eight loci, including six chromosomal loci, vrrA, vrrB1, vrrB2, vrrC1, vrrC2, and CG3, and two plasmid loci, pXO1-aat and pXO2-at. VNTR markers have high genetic stability, which makes MLVA highly reproducible (10) and thus permits direct comparison of data from different laboratories. Following the original work of Keim et al. (13, 14), a number of studies addressed the biogeography of B. anthracis, characterizing strains originating from Kruger National Park in South Africa (25), France (8, 18), Poland (9), China (3), Italy (7), and Korea (22) and strains isolated following terrorist attacks in Japan (15) and the United States (10). These studies provided a clearer picture of the global spread and regional diversity of B. anthracis.
In the Caucasus, anthrax can be considered endemic, and the frequency of outbreaks has increased dramatically in the last 10 years according to the World Anthrax Data Site (http://www.vetmed.lsu.edu/whocc/georgia.htm). Georgia has been considered one of the countries most affected by outbreaks, including human cases (11). However, only a few sporadic reports have documented the occurrence of B. anthracis in the Caucasus (11; http://www.vetmed.lsu.edu/whocc/georgia.htm; http://www.ncdc.ge/Eng/statistics/Communicable%20Diseases%202004_files/frame .html), and very little information and incomplete data on the diversity of B. anthracis in this region are available.
In the other republics of the former Soviet Union (FSU), a similar situation exists, and in general, few strains have been characterized previously using MLVA and other molecular methods. An exception is the strains involved in the incident that occurred in Sverdlovsk (now Ekaterinburg, Russia) in 1979 (12).
There have also not been careful molecular characterizations of strains used in the FSU for both human and veterinary vaccines. Molecular characterization of the vaccine strains that were used in the FSU and are still used in many countries of the FSU would provide further data for evaluating the diversity of the isolates that are used worldwide for production of anthrax vaccines (14).
In the present study MLVA and other molecular typing methods were used to investigate B. anthracis diversity in Georgia and to characterize vaccine strains used in the FSU.
Geographical distribution of B. anthracis in Georgia.
In the South Caucasian region, which is a border area between Europe and the Middle East, there was an increase in anthrax outbreaks following the disintegration of the FSU, making this region an interesting area for studying B. anthracis biodiversity and migration through the region. The World Anthrax Data Site (WHO Collaborating Center for Remote Sensing and Geographic Information Systems, Louisiana State University, United States; http://www.vetmed.lsu.edu/whocc/georgia.htm) shows that anthrax is enzootic in the South Caucasus, is endemic in Georgia, and is sporadic in Armenia and Azerbaijan. However, there is a lack of official data concerning animal infection in the South Caucasus, and official reports are rare and incomplete. According to official data, from 1992 to 2001 only 10 animal anthrax outbreaks were recorded in Georgia. These data are not realistic and likely are an underestimate based on the incidence of human anthrax in the same region. In the period from 1990 to 2003, 196 human cases were recorded in Georgia (P. Imnadze, L. Bakanidze, G. Katsitadze, L. Malania, and M. Kekelidze, Abstr. 5th Int. Conf. Anthrax, abstr. P510, 2003; A. Roberts, N. Chanishvili, S. Rigvava, M. Natidze, M. Tediashvili, B. Cherkasskiy, D. Daffonchio, and R. Sharp, Abstr. 5th Int. Conf. Anthrax, abstr. P507, 2003; http://www.ncdc.ge/Eng/statistics/Communicable%20Diseases%202004_files/frame.html). The geographic distribution of human cases indicates that anthrax foci are located in particular districts. In several districts human cases were recorded occasionally over the last 10 years; in the East Georgia districts of Gardabani and Rustavi, cases occurred every year, and there were also some large outbreaks, such as those in Dedoplistskaro and Gardabani in 1999 (24 and 16 cases, respectively) and in Akhalkalaki in 2000 (20 cases). Human cases were particularly frequent in the Gardabani area, with 39 cases recorded in the period from 1997 to 2002 (Imnadze et al., Abstr. 5th Int. Conf. Anthrax; http://www.ncdc.ge/Eng/statistics/Communicable%20Diseases%202004_files/frame.html).
From August 2002 to May 2003 samples were obtained from several sites in eight different areas of Georgia for isolation of B. anthracis (Table 1). The sites sampled covered a 300-km transect in Georgia, including valley and mountain areas. The sites selected were considered reservoirs of B. anthracis in which the organism is endemic, and in these areas several cases were recorded in the past 5 to 7 years. Three blood samples (from two humans and a goat) and a total of 239 soil samples were collected from animal burial sites, abattoirs, sites where animals died, and animal stalls. Because of the high levels of infection in the Gardabani area, 70 samples were collected there. Sampling expeditions that resulted in isolation of B. anthracis were sent to eastern Georgia in the Gachiani, Gamarjveba, and Gardabani areas; in central Georgia in the Abisi area; and in western Georgia in the Rukhi, Zugdidi, Senaki and Kutaisi areas (Table 1).
TABLE 1.
Characteristics of B. anthracis isolates used in this study, including Georgian isolates and vaccine strains used in the FSU
| Origina | Strain(s) | Source | Availability in the G. Eliava IBMV Collectionb | Place of isolation | GG genotypec | GK genotype(s)d | Genetic clustere | VNTR marker sizes (bp)f
|
|||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| vrrA | vrrB1 | vrrB2 | vrrC1 | vrrC2 | CG3 | pXO1 | pXO2 | ||||||||
| Georgia | G319, G321 | Soil, animal burial | 2003 (July) | Gardabani | I | 35 | A3.a | 313 | 229 | 162 | 613 | 532 | 158 | 132 | 141 |
| G325 | Goat blood | 2003 (July) | Gardabani | I | 35 | A3.a | 313 | 229 | 162 | 613 | 532 | 158 | 132 | 141 | |
| A95 | Soil, animal burial | 2003 (January) | Abisi | II | 40 | A3.a | 313 | 229 | 162 | 613 | 532 | 158 | 132 | 139 | |
| R313 | Soil, animal burial | 2003 (July) | Rukhi | II | 40 | A3.a | 313 | 229 | 162 | 613 | 532 | 158 | 132 | 139 | |
| A83, A96 | Soil, animal stall | 2003 (January) | Abisi | III | 44 | A3.a | 313 | 229 | 162 | 613 | 532 | 158 | 126 | 141 | |
| L40 | Soil, animal burial | 2003 (January) | Gachiani | III | 44 | A3.a | 313 | 229 | 162 | 613 | 532 | 158 | 126 | 141 | |
| L42 | Human blood | 2003 (January) | Gamarjveba | III | 44 | A3.a | 313 | 229 | 162 | 613 | 532 | 158 | 126 | 141 | |
| K187, K189, K197, K199 | Soil, animal burial | 2003 (February) | Kutaisi | III | 44 | A3.a | 313 | 229 | 162 | 613 | 532 | 158 | 126 | 141 | |
| K200 | Soil, abattoir | 2003 (February) | Kutaisi | III | 44 | A3.a | 313 | 229 | 162 | 613 | 532 | 158 | 126 | 141 | |
| R296 | Soil, animal burial | 2003 (June) | Rukhi | III | 44 | A3.a | 313 | 229 | 162 | 613 | 532 | 158 | 126 | 141 | |
| S377 | Soil, field | 2003 (October) | Senaki | III | 44 | A3.a | 313 | 229 | 162 | 613 | 532 | 158 | 126 | 141 | |
| SCh343 | Human blood | 2003 (October) | Senaki | III | 44 | A3.a | 313 | 229 | 162 | 613 | 532 | 158 | 126 | 141 | |
| ZR347 | Soil, abattoir | 2003 (October) | Zugdidi | III | 44 | A3.a | 313 | 229 | 162 | 613 | 532 | 158 | 126 | 141 | |
| FSU vaccines | 34F2g,i | Unknown | 1956 | Unknown | IV | 59, 61h | A3.b | 313 | 229 | 162 | 583 | 532 | 158 | 129 | |
| STI-1i | Unknown | 1962 | Unknown | V | − | A1.a | 313 | 229 | 162 | 613 | 604 | 153 | 129 | ||
| I-17i | Unknown | 1967 | Unknown | VI | 15, 16, 17h | A1.a | 325 | 229 | 162 | 613 | 604 | 153 | 132 | ||
| 55i | Unknown | 1976 | Unknown | VII | 3, 4, 5h | A1.a | 313 | 229 | 162 | 613 | 604 | 153 | 126 | ||
| 71/12i | Unknown | 1985 | Unknown | VIII | − | A1.a | 313 | 229 | 162 | 613 | 532 | 153 | 132 | 135 | |
Strains were isolated in Georgia or were used in the former Soviet Union as vaccine strains.
Year when the strain was isolated or received by the G. Eliava IBMV Collection. The month of isolation is indicated in parentheses.
Genotype of isolate as defined in this study.
Genotype as defined by Keim et al. (14). −, isolate has a novel genotype and no equivalent genotype was described by Keim et al. (14).
Genetic cluster as defined by Keim et al. (14).
Allele sizes determined by capillary electrophoresis with an ABI Prism 310. Sizes were rounded to the nearest whole number and calibrated to the sizes reported by Keim et al. (14).
Strain 34F2 is a Sterne strain.
As a result of missing data for the pXO2 locus, the isolate matches several of the genotypes defined by Keim et al. (14).
Strain received from Tarasevich State Standardization and Control of Medical Preparations Research Institute, Moscow, Russia.
From an initial collection containing 34 isolates a total of 18 strains were identified as B. anthracis (Table 1); these strains included 3 strains isolated from blood, 10 strains isolated from soil from animal burial sites, 2 strains isolated from animal stalls, 2 strains isolated from abattoirs, and 1 strain isolated from a soil with a previous history of an anthrax outbreak.
Notably, control samples collected from the Akhaltsikhe area in southern Georgia, where cases of B. anthracis have never been recorded, did not yield B. anthracis isolates (data not shown).
B. anthracis vaccine strains in the FSU.
Until 1991 the G. Eliava Institute of Bacteriophage, Microbiology and Virology (G. Eliava IBMV) was one of a small number of facilities producing anthrax vaccines in the FSU, and it retains a collection of five B. anthracis strains previously used for vaccine preparation but not yet characterized genetically (Table 1). The Sterne 34F2 strain, lacking the pXO2 plasmid (26), was received by the G. Eliava IBMV collection in 1956. Three other strains, STI-1 (14), I-17, and 55, were pXO2 negative and were received by the G. Eliava IBMV collection in 1962, 1967, and 1976, respectively. Strain 71/12 was received in 1985 and is considered a semivirulent strain in spite of the fact that it has both the pXO plasmids and a full set of virulence and capsule genes (see below).
Strain STI-1 was used in the FSU for preparation of human vaccine (24, 27). The other strains were considered strains for veterinary use.
Phenotypic and molecular characterization of wild B. anthracis isolates and vaccine strains.
All B. anthracis strains were characterized by performing standard tests recommended by the World Health Organization, including tests to determine colony and cell morphology, capsule-forming ability, motility, hemolytic activity, and sensitivity to gamma phage and penicillin and in vivo virulence tests with the white mouse model (27). Virulence was confirmed by injecting suspensions (approximately 10,000 CFU ml−1) into mice (0.05 to 0.1 ml subcutaneously). Virulent B. anthracis killed the animals in 42 to 48 h (27). Prior to bacteriological analysis, the reversed passive hemagglutination test and the Ouchterlony test for double diffusion in agar were performed directly with soil samples, as well as with bacterial isolates (17, 20). Based on immunological analyses of soil samples and a preliminary analysis of colony morphology, 30 of the initial 34 isolates were provisionally identified as B. anthracis and subjected to further analytical tests. Eighteen isolates developed rough-texture white to gray colonies with the classical medusa head appearance on the agar plates and exhibited gelatin degradation and capsule and spore formation. The isolates were all nonmotile, nonhemolytic, and sensitive to penicillin and gamma phage. The virulence of all strains was confirmed using the mouse subcutaneous infection model (27).
Molecular characterization of B. anthracis.
Total DNA was extracted by the standard phenol-chloroform method (23). Amplification of the pag, cya, lef, and cap virulence genes by PCR was performed using primers and conditions described by Ramisse et al. (19). The chromosomal marker SG749 was used to confirm the identity B. anthracis by restriction analysis of the SG749 product amplified with AluI and successive agarose gel electrophoresis (4). Intergenic transcribed spacer homoduplex-heteroduplex polymorphism profiles of the strains were determined by PCR and subsequent separation in mutation detection enhancement-based polyacrylamide gels using the procedures described previously (5, 6). Repetitive element polymorphism PCR profiles of B. anthracis strains were obtained by BOX-A1R primer-based PCR and separation by agarose gel electrophoresis using the conditions described previously (1, 2).
The pag, cya, lef, and cap virulence genes were detected in all 18 newly isolated strains and in vaccine strain 71/12. The other four vaccine strains lacked the cap gene located on the pXO2 plasmid (data not shown). No PCR products were obtained for the remaining isolates of the initial strain collection when sequences were amplified with the primer sets for the four virulence genes. When analyzed to determine the presence of the SG749 marker, all the virulent and vaccine strains produced the typical AluI restriction profile of B. anthracis, i.e., two restriction fragments at 660 bp and 90 bp (4). All of the new isolates and the vaccine strains exhibited the same intergenic transcribed spacer homoduplex-heteroduplex polymorphism profile typical of B. anthracis, with intergenic transcribed spacer homoduplex bands at about 240 and 460 bp and a series of slowly migrating heteroduplex bands (5). The strains were characterized by repetitive element polymorphism PCR with the BOX-A1R primer, and all of them produced major bands at approximately 130, 400, 630, and 770 bp, as previously shown for B. anthracis (2).
Typing virulent and vaccine B. anthracis strains by MLVA.
MLVA of the Georgian and vaccine strains was performed as described by Keim et al. (14). For each strain, four PCR mixtures were prepared. Reactions 1 and 2 were multiplex PCRs for amplification of the VNTR regions vrrA, vrrB1, and CG3 and the VNTR regions vrrB2, pXO1-aat, and pXO2-at, respectively. Reactions 3 and 4 were single PCRs for amplification of the VNTRs vrrC1 and vrrC2. Each of the four PCRs was carried out by using 30-μl mixtures in an I-cycler (Bio-Rad, Milan, Italy) and 1.0 U of Taq DNA polymerase (Fermentas, Milan, Italy). PCR products were labeled with fluorophores by using the fluorescently labeled primers described by Keim et al. (14). The PCR cycling conditions were as follows: initial denaturation at 94°C for 5 min, followed by 35 cycles consisting of 94°C for 30 s, 62°C for 30 s, and 72°C for 30 s and a final extension step at 72°C for 10 min.
PCR products were analyzed with an ABI Prism 310 capillary sequencer (Applied Biosystems). One microliter of each of the four PCR mixtures was mixed with 1 μl of the 1,000-bp ROX internal size standard (Applied Biosystems) labeled with the phosphoramidite dye 6-carboxyrhodamine. Fourteen microliters of deionized formamide was added, and the mixture was denatured at 95°C for 10 min and cooled in an ice bath. For separation of the PCR products, a capillary (47 cm by 50 μm) filled with 4% performance-optimized polymer (Applied Biosystems) was used. The samples were electrophoresed under standard ABI 310 denaturing electrophoresis conditions for 45 min at 60°C. The data were analyzed using the GeneScan 3.1 software program (Applied Biosystems). The output of the analysis was a series of peaks (an electropherogram), the sizes of which were estimated by comparison with the fragments of the internal size standard. A threshold of 50 fluorescent units was used, and analysis of the size standard was performed by the local Southern method and with light data smoothing. If the baseline varied inconsistently, the sample was rerun. The results were compared to B. anthracis genotypes described by Keim et al. (14).
Diversity group clusters were analyzed using the sequential agglomerative hierarchical nested cluster analysis and unweighted pair group method analysis using average linkage clustering routines in the NTSYSpc 3.0 software package (21). Although the isolates lacking pXO2 were subjected to genotyping with seven MLVA markers, the data obtained were not included in the cluster analysis due to incompatibility of the marker number tested. A simple percent distance similarity matrix of the allele values for the isolates was constructed prior to cluster analysis. Individual marker diversity (Simpson diversity index) was calculated by using 1 − Σ(allele frequency)2 (14) and was based on the entire virulent isolate collection used in the study.
The sizes of the alleles detected by MLVA in all the strains analyzed are listed for each of the eight VNTR markers in Table 1, along with the designations of the global diversity groups, based on the analysis performed by Keim et al. (14). Based on marker allele combinations eight genotypes, designated GG I to GG VII in Table 1, were found among the strains analyzed. Table 1 also shows strain genotypes (GK genotypes) defined by Keim et al. (14).
Three distinct MLVA genotypes (GG I to GG III) were found for the Georgian isolates, and all of them belonged to cluster A3.a in the clustering system of Keim et al. (14). In the Georgian isolates, the informative VNTR markers were those from pXO1 and pXO2. These two markers are considered the most discriminatory markers for describing the diversity of B. anthracis (14). The diversity indexes of the pXO1 and pXO2 markers for the Georgian strains were 0.43, and 0.21, respectively. No diversity was observed for the other six VNTR markers.
Most of the isolates (13 of 18) represented the rare genotype GK 44, previously reported for only three strains found in Turkey and Namibia (14). The genotype of three other Georgian isolates was genotype GK 35, which has been found previously in Turkey, Namibia, the United Kingdom, and the United States. The three isolates with this genotype originated from different sources in one place (Gardabani) (Table 1); two were obtained from different animal burial sites, and one was obtained from the blood of a dead goat. The two other isolates represented the GK 40 genotype previously found only in Africa (in particular, Namibia, Mozambique, and Zimbabwe).
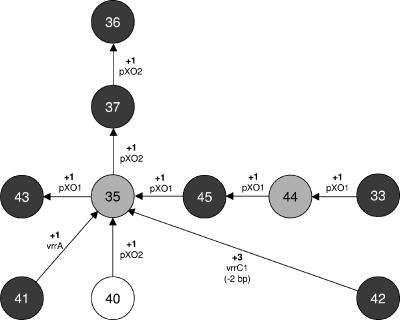
To describe the genetic relationship between genotypes found in the Turkish-Southern Caucasian region, a mutational step model, based on the minimum number of mutations in the MLVA loci needed to create the diversity observed, was developed (Fig. 1). All the GK genotypes belonging to cluster A3.a previously found in Turkey (14) and in Georgia were included in the model. Keim et al. (14) thought that the geographical distribution of the genotypes could be a function of isolate availability rather than the intrinsic diversity in a limited geographic area. Most of the Georgian isolates used in this study were obtained from soils that had a previous history of anthrax, but the anthrax outbreaks occurred long ago, so the collection should have been less biased than other collections that included only strains isolated during outbreaks. The sampling and isolation strategies used to obtain the Turkish isolates are unknown, making any estimate of the sampling bias infeasible.
FIG. 1.
Mutational step model showing the genetic relationships between the B. anthracis MLVA GK genotypes found in Turkey and Georgia and belonging to the A3.a genetic cluster, as defined by Keim et al. (14). Each circle represents a different genotype, and the notations on the lines connecting the genotypes indicate the minimal mutational changes needed to convert one genotype to another. The data are data for Georgian isolates characterized in this work and for the Turkish isolates characterized by Keim et al. (14). The dark gray circles indicate genotypes found in Turkey, the open circle indicates a genotype found only in Georgia, and the light gray circles indicate the genotypes found in both the countries.
The model shown in Fig. 1 indicates that most of the genotypes found in the region are closely related and that there are few mutations in the pXO markers. Genotype GK 35 was the central genotype in the model, at the intersection of the mutational steps of the pXO1 and pXO2 markers, suggesting that it is a significant genotype in the Turkish-Southern Caucasian region. Indeed, genotype GK 35 has been found in both Turkey and Georgia, and in the work of Keim et al. (14) a relatively large number of isolates from Turkey (22 of 41 strains) had this genotype.
Genotype GK 44 was found in both Turkey and Georgia, but considering the number of isolates with this genotype from the two countries, it seems to be a more prevalent genotype in Georgia (South Caucasus) than in Turkey. Thirteen of the 18 Georgian isolates had this genotype, and it was found at seven of the eight locations. The only location where it was not found was Gardabani, a city close to the border with Azerbaijan. Isolates from Gardabani had genotype GK 35, which is a prevalent Turkish genotype. The Gardabani region is a center for commercial exchange of livestock with Azerbaijan, and it is used as a place to pasture Azerbaijani livestock. The fact that genotype GK 35 was found only in Gardabani suggested that it could have been derived from adjacent Azerbaijan and indicates that a careful description of the pattern of B. anthracis spread in the Turkish-Southern Caucasian region requires typing of isolates from Azerbaijan and Armenia.
Although in the study of Keim et al. (14) the third Georgian genotype, genotype GK 40, was found only in African strains, this genotype differs from the other Georgian and Turkish genotypes only by the VNTR marker pXO2; hence, it is related to most of the other Turkish genotypes. The fact that genotype GK 40 was found in Georgia suggests that it could be typical of the Turkish-Southern Caucasian region, resulting from mutation of other genotypes in the region (e.g., genotype GK 35) rather than from independent introduction from other places.
The MLVA-based diversity data presented in this study establish the first picture of the genetic diversity of B. anthracis in the Southern Caucasus. A comparison of the data for the Georgian and Turkish isolates suggests that there is a common regional strain pattern in the Turkish South-Caucasian region, dominated by strictly related genotypes that differ only in a few polymorphisms in the pXO-based VNTR markers. Hence, it can be hypothesized that B. anthracis strains responsible for anthrax outbreaks in the region result from recent evolution of a common ancestral strain. However, the possibility that the pXO1 and pXO2 marker differences between the observed genotypes could be due to spontaneous mutations in these rapidly evolving markers due to strain subculturing cannot be excluded. Indeed, we did not intensively subculture the Georgian isolates to minimize this possible bias. Hence, to confirm the previous conclusion and to clarify the pattern of B. anthracis spread in the east-west and north-south directions in the Caucasian-Turkish region, it will be necessary to type by MLVA clinical and virulent isolates that occur in natural outbreaks in Azerbaijan and Armenia, as well as in the northern Caucasian region.
Four of the five vaccine strains lacked pXO2, and hence, the related plasmid marker could not be included in the analysis. Based on the other seven VNTR marker profiles (Table 1), these strains could be affiliated with several GK genotypes. Strains I-17 and 55 could be affiliated with genotypes in the A1.a cluster (genotype GK 15, GK 16, or GK 17 and genotype GK 3, GK 4, or GK 5, respectively). The strain STI-1 genotype confirmed the genotype reported by Keim et al. (14), with allele sizes (excluding the pXO2 marker) of 313, 229, 162, 613, 604, 153, and 129 bp (Table 1), and although it did not match any previously defined genotype due to the lack of the pXO2 plasmid, it could be affiliated with the A1.a cluster. Also, the Sterne 34F2 strain lacked the pXO2 marker and for the remaining seven markers had the MLVA genotype described by Keim et al. (14), with allele sizes of 313, 229, 162, 583, 532, 158, and 129 bp (Table 1). According to these markers the most similar genotypes were genotypes GK 59 and GK 61 in the A3.b cluster (14).
Strain 71/12 had an MLVA profile that does not match any of the previously described genotypes (Table 1). According to the 153-bp CG3 allele typical of cluster A1.a isolates (14), the strain 71/12 genotype is a novel genotype in the A1.a cluster, which can be distinguished from the other genotypes by means of a 532-bp vrrC2 marker.
In addition to the well-known Sterne 34F2 strain and the previously described STI-1 strain, there were three other strains which represented the Russian strains widely used in the former Soviet Union for vaccine preparation. Despite their origin all of these strains were grouped in the A1.a cluster with other isolates, most of which were from North America. Hence, their relatively high polymorphism is probably the vestigial result of a rather different geographical origin.
Acknowledgments
This study was supported by INTAS, the International Association for the Promotion of Cooperation with Scientists from the New Independent States of the Former Soviet Union, as part of the project “An epidemiological study of outbreaks of B. anthracis in Georgia” (INTAS-01-0725) and by ISPELS as part of project B74/MDL/02. M.M. was supported by a Cariplo Foundation fellowship organized by LNCV-Landau Network-Centro Volta.
REFERENCES
- 1.Cherif, A., S. Borin, A. Rizzi, H. Ouzari, A. Boudabous, and D. Daffonchio. 2002. Characterisation of a rep-PCR chromosomal marker that discriminates Bacillus anthracis from related species. J. Appl. Microbiol. 93:456-462. [DOI] [PubMed] [Google Scholar]
- 2.Cherif, A., L. Brusetti, S. Borin, A. Rizzi, A. Boudabous, H. Khyami-Horani, and D. Daffonchio. 2003. Genetic relationship in the ‘Bacillus cereus group’ by rep-PCR fingerprinting and sequencing of a Bacillus anthracis-specific rep-PCR fragment. J. Appl. Microbiol. 94:1108-1119. [DOI] [PubMed] [Google Scholar]
- 3.Cheung, D. T., K. M. Kam, K. L. Hau, T. K. Au, C. K. Marston, J. E. Gee, T. Popovic, M. N. Van Ert, L. Kenefic, P. Keim, and A. R. Hoffmaster. 2005. Characterization of a Bacillus anthracis isolate causing a rare case of fatal anthrax in a two-year-old boy from Hong Kong. J. Clin. Microbiol. 43:1992-1994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Daffonchio, D., S. Borin, G. Frova, R. Gallo, E. Mori, R. Fani, and C. Sorlini. 1999. A randomly amplified polymorphic DNA marker specific for the Bacillus cereus group is diagnostic for Bacillus anthracis. Appl. Environ. Microbiol. 65:1298-1303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Daffonchio, D., A. Cherif., and S. Borin. 2000. Homoduplex and heteroduplex polymorphisms of the amplified ribosomal 16S-23S internal transcribed spacers describe genetic relationships in the “Bacillus cereus group”. Appl. Environ. Microbiol. 66:5460-5468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Daffonchio, D., A. Cherif, L. Brusetti, A. Rizzi, D. Mora, A. Boudabous, and S. Borin. 2003. On the nature of polymorphisms in 16S-23S rDNA intergenic transcribed spacer fingerprinting of Bacillus and related genera. Appl. Environ. Microbiol. 69:5128-5137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Fasanella, A., M. Van Ert, S. A. Altamura, G. Garofolo, C. Buonavoglia, G. Leori, L. Huynh, S. Zanecki, and P. Keim. 2005. Molecular diversity of Bacillus anthracis in Italy. J. Clin. Microbiol. 43:3398-3401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Fouet, A., K. L. Smith, C. Keys, J. Vaissaire, C. Le Doujet, M. Lévy, M. Mock, and P. Keim. 2002. Diversity among French Bacillus anthracis isolates. J. Clin. Microbiol. 40:4732-4734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gierczynski, R., S. Kałuzewski, A. Rakin, M. Jagielski, A. Zasada, A. Jakubczak, B. Borkowska-Opacka, and W. Rastawicki. 2004. Intriguing diversity of Bacillus anthracis in eastern Poland the molecular echoes of the past outbreaks. FEMS Microbiol. Lett. 239:235-240. [DOI] [PubMed] [Google Scholar]
- 10.Hoffmaster, A. R., C. C. Fitzgerald, E. Ribot, L. W. Mayer, and T. Popovic. 2002. Molecular subtyping of Bacillus anthracis and the 2001 bioterrorism-associated anthrax outbreak, United States. Emerg. Infect. Dis. 8:1111-1116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Imnadze, P., L. Bakanidze, M. Manrikyan, T. Kukhalashvili, E. Zangaladze, M. Kekelidze, D. Tsereteli, M. Nadiradze, S. Tsanava, and N. Tserstvadze. 2002. Anthrax in southern Caucasus. Antibiot. Monit. 18:17-18. [Google Scholar]
- 12.Jackson, P. J., M. E. Hugh-Jones, D. M. Adair, G. Green, K. K. Hill, C. R. Kuske, L. M. Grinberg, F. A. Abramova, and P. Keim. 1998. PCR analysis of tissue samples from the 1979 Sverdlovsk anthrax victims: the presence of multiple Bacillus anthracis strains in different victims. Proc. Natl. Acad. Sci. USA 95:1224-1229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Keim, P., A. Kalif, J. Schupp, K. Hill, S. E. Travis, K. Richmond, D. M. Adair, M. Hugh-Jones, C. R. Kuske, and P. Jackson. 1997. Molecular evolution and diversity in Bacillus anthracis as detected by amplified fragment length polymorphism markers. J. Bacteriol. 179:818-824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Keim, P., L. B. Price, A. M. Klevytska, K. L. Smith, J. M. Schupp, R. Okinaka, P. J. Jackson, and M. E. Hugh-Jones. 2000. Multiple-locus variable-number tandem repeat analysis reveals genetic relationships within Bacillus anthracis. J. Bacteriol. 182:2928-2936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Keim, P., K. L. Smith, C. Keys, H. Takahashi, T. Kurata, and A. Kaufmann. 2001. Molecular investigation of the Aum Shinrikyo anthrax release in Kameido, Japan. J. Clin. Microbiol. 39:4566-4567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mock, M., and A. Fouet. 2001. Anthrax. Annu. Rev. Microbiol. 55:647-671. [DOI] [PubMed] [Google Scholar]
- 17.Ouchterlony, O. 1962. Diffusion-in-gel methods for immunological analysis II. Prog. Allergy 6:30-154. [DOI] [PubMed] [Google Scholar]
- 18.Patra, G., J. Vaissaire, M. Weber-Levy, C. Le Doujet, and M. Mock. 1998. Molecular characterization of Bacillus strains involved in outbreaks of anthrax in France in 1997. J. Clin. Microbiol. 36:3412-3414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ramisse, V., G. Patra, H. Garrigue, J.-L. Gusdon, and M. Mock. 1996. Identification and characterization of Bacillus anthracis by multiplex PCR analysis of sequences on plasmids pXO1 and pXO2 and chromosomal DNA. FEMS Microbiol. Lett. 145:9-16. [DOI] [PubMed] [Google Scholar]
- 20.Rigvava, S., M. Natidze, R. Sharp, M. Bubashvili, D. Gogiashvili, L. Kavtaradze, N. Vardzelashvili, M. Karukhnishvili, N. Chanishvili, and M. Tediashvili. 2004. Application of RPHA for express diagnostics of anthrax. Proc. Georg. Acad. Sci. Biol. Ser. 30:565-570. [Google Scholar]
- 21.Rohlf, F. J. 1998. NTSYSpc, ed. 2.02. Exeter Software, Stony Brook, N.Y.
- 22.Ryu, C., K. Lee, H.-J. Hawng, C.-K. Yoo, W.-K. Seong, and H.-B. Oh. 2005. Molecular characterization of Korean Bacillus anthracis isolates by amplified fragment length polymorphism analysis and multilocus variable-number tandem repeat analysis. Appl. Environ. Microbiol. 71:4664-4671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Sambrook, J., E. F. Fritsch, and T. Maniatis. 1989. Molecular cloning: a laboratory manual, 2nd ed. Cold Spring Harbor Laboratory Press, Cold Spring Harbor, N.Y.
- 24.Shlyakhov, E. N., and E. Rubinstein. 1994. Human live anthrax vaccine in the former USSR. Vaccine 12:727-730. [DOI] [PubMed] [Google Scholar]
- 25.Smith, K. L., V. DeVos, H. Bryden, L. B. Price, M. E. Hugh-Jones, and P. Keim. 2000. Bacillus anthracis diversity in Kruger National Park. J. Clin. Microbiol. 38:3780-3784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Turnbull, P. C. 1991. Anthrax vaccines: past, present and future. Vaccine 9:533-539. [DOI] [PubMed] [Google Scholar]
- 27.Turnbull, P. C. B., et al. 1998. Guidelines for the surveillance and control of anthrax in humans and animals, 3rd ed. WHO/EMC/ZDI./98.6. World Health Organization, Geneva, Switzerland.