Abstract
The clinical value of immunoenzymatic (enzyme-linked immunosorbent assay) detection of anti-Toxoplasma immunoglobulin E (IgE) was assessed by studying 2,036 sera from 792 subjects, comprising seronegative controls and subjects with acute, active, reactivated, or congenital toxoplasmosis. Included were nonimmunized adults; pregnant women with recently acquired infection (acute toxoplasmosis); immunocompetent subjects with recently acquired severe infection (active toxoplasmosis) expressed as fever, adenopathies, splenomegaly, pneumonia, meningitis, or disseminated infection; subjects—some of them immunocompromised—whose previously moderate IgG antibody levels rose, suggesting a reactivation of quiescent toxoplasmosis; and infants born to seroconverted mothers and evaluated for diagnosis of congenital infection and therapeutic management. Specific IgE antibodies were never detected in seronegative subjects. They were present in 85.7% of asymptomatic seroconverters and in 100% of seroconverters with overt toxoplasmosis, following two different kinetics: in the former, the specific IgE titer generally presented a brief peak 2 to 3 months postinfection and then fell rapidly, whereas specific IgE persisted at a very high titer for several months in the latter. IgE emerged concomitantly with the increase in IgG during toxoplasmic reactivation. For neonatal diagnosis of congenital toxoplasmosis, IgE was less informative than IgM and IgA (sensitivities, 59.5, 64.3, and 76.2%, respectively) and had a specificity of 91.9%. Nevertheless, simultaneous measurement of the three isotypes at birth improved the diagnostic yield to 81% relative to the combination of IgA and IgM. Emergence of specific IgE during postnatal treatment for congenital toxoplasmosis is a sign of poor adherence or inadequate dosing.
Toxoplasmosis, a cosmopolitan protozoan disease, is often asymptomatic in humans. Its diagnosis is mainly based on serological tests. Classically, serodiagnosis includes titration of specific immunoglobulin G (IgG) (showing past exposure) and screening for specific IgM, which is suggestive of recent exposure or ongoing active infection (17). However, IgM antibody detection can be due to naturally interfering IgM (15) or to the persistence of IgM for a long time after primary infection. Conversely, the IgM assay can be negative in patients with secondary reactivation or congenital toxoplasmosis (3, 6). Although anti-Toxoplasma IgA antibodies are also informative (i.e., no natural IgA), they can persist for >6 months after infection, making it difficult to determine the precise date of infection in pregnant women (8, 9). There is therefore growing interest in the use of IgE in this setting (1, 10, 14, 18, 22). Given the major role of Toxoplasma gondii P30 membrane protein in early antibody synthesis (4), we have used an enzyme-linked immunosorbent assay (ELISA) based on a monoclonal anti-P30 antibody to screen for specific IgE.
The aim of this study was to determine the kinetics of anti-Toxoplasma IgE in ELISA and the clinical value of the IgE assay in active, reactivated, and congenital toxoplasmosis.
MATERIALS AND METHODS
Patients and sera.
Two thousand thirty-six samples from 792 adults and infants were tested. The samples were subdivided as follows.
(i) Adults (308 patients; 836 sera).
Group A1 consisted of 104 women who contracted toxoplasmosis just before (9 cases) or during (63 infections in the first trimester, 22 in the second trimester, and 10 in the third trimester) pregnancy. Toxoplasma infection was recognized either by symptoms (adenopathies, 15 cases [4 with fever]; isolated fever, 5 cases; fatigue, 4 cases) confirmed to be related to toxoplasmosis by immunological investigations or by serological tests alone in the absence of any symptoms (French law prescribes that nonimmunized pregnant women be tested monthly). In this group, 19 women (patients 1 to 3 infected in the first trimester, patients 4 to 12 infected in the second trimester, and patients 13 to 19 infected in the third trimester) transmitted the infection to their fetuses (subgroup A1+; 60 sera). The offspring of the remaining 85 women (patients 20 to 104) were uninfected (subgroup A1−; 357 sera). Group A2 consisted of eight men (28 sera) and nine women (34 sera) with no known immunodeficiency (patients 105 to 121) who had symptomatic primary toxoplasmic infection. Group A3 consisted of four women (patients 122 to 125; 15 sera) with serological evidence of toxoplasmic reactivation. Group A4 consisted of 49 pregnant women (patients 126 to 174; 141 sera) who had acquired immunity before conception. Group A5 consisted of 121 nonimmune subjects (negative controls; patients 175 to 295; 142 sera). Group A6 consisted of 13 immunodepressed kidney graft recipients (patients 296 to 308; 59 sera), comprising 6 men (12 sera) and 7 women (47 sera).
(ii) Infants (442 infants; 1,053 sera).
Infants born to mothers who seroconverted during pregnancy were divided into two groups. Group I+ consisted of 68 infants with congenital toxoplasmosis (patients 309 to 376; 385 sera), 42 of whom were <3 months old and 26 of whom were between 3 months and at least 2 years old. The diagnosis of congenital toxoplasmosis was established by antenatal investigation of amniotic fluid or by demonstration of toxoplasmic lesions and/or by persistence of anti-Toxoplasma antibodies after 1 year of age. Group I− consisted of 374 infants (patients 377 to 750; 668 sera), clinically safe and <2 years old, who were declared free of congenital toxoplasmosis when they lost anti-Toxoplasma antibodies in <1 year of life in the absence of antitoxoplasmic treatment.
(iii) Cord blood samples (n = 147).
Group C+ consisted of 15 cord blood samples obtained at the birth of infants with congenital toxoplasmosis. Maternal infection occurred in the second (5 cases) or third (10 cases) trimester. No other samples were obtained from the infant in one of these cases (patient 751, whose congenital toxoplasmosis had been diagnosed by antenatal investigation). Group C− consisted of 132 cord blood samples obtained at the birth of infants who were free of congenital toxoplasmosis. Maternal infection occurred in the first (69 cases), second (46 cases), or third (17 cases) trimester. No other samples were obtained from the infants in 21 of these cases (patients 752 to 772, whose later follow-up depended on other centers).
Immunoenzymatic technique: double sandwich ELISA.
The method used to measure specific anti-Toxoplasma IgE was developed in our laboratory from a previously described IgM-IgA ELISA technique (6). Briefly, microplate wells (96-well plates; Nunc 469914F16 Maxisorp) were coated with 200 μl of anti-ɛ monoclonal antibody solution (10 μg/ml) (ANA B16; 24138; Argène-Biosoft, Varilhes, France,) for 16 h at room temperature (18 to 25°C). The plates were then washed (in phosphate-buffered saline [PBS]-10% Tween 20; 822184050020; Merck) and saturated with 300 μl of 0.1% Tween 20/well in 0.1 M Tris buffer (T1503; Sigma). The plates were washed after 1 h at room temperature, and then a postsaturation solution containing 100 g of saccharose (7653; Merck)/liter in 0.1 M Tris buffer was added (250 μl per well). After incubation for 1 h at room temperature, the postsaturation solution was removed and the plates were dried for 1.5 h at 37°C. They were then placed in plastic bags containing a desiccator or were vacuum packed (Turbovac SB415; PSV, Genainville, France). They were either used immediately or kept at 4°C for up to 6 months.
The test sera and negative and positive controls were diluted 1/25 in PBS buffer and distributed (200 μl) in duplicate wells. After 2 h in a 25°C incubator (Dynatech MR 7000), the plates were washed in PBS-Tween 20. The conjugate, consisting of anti-T. gondii P30 monoclonal antibody labeled with peroxidase (anti-T. gondii 30-kDa GII9; 11-132; Argène-Biosoft) and soluble antigen (obtained from peritoneal exudates of mice infected 96 h previously with the RH strain of T. gondii), was automatically distributed (MRD; Dynatech) in each well (200 μl per well). After 1 h at 25°C, the plates were washed, and 200 μl of substrate per well (orthophenylenediamine [P8412; Sigma]) was automatically added. After a final incubation step of 15 min at 25°C, 100 μl of arrest solution (1 N HCl [9970; Merck]) was added. The optical density (OD) at 490 to 630 nm was read directly with a spectrophotometer (Dynatech). Based on the experience of ELISA IgA detection previously described (6), an IgE index was calculated for each test sample as follows: sample OD/0.4 (mean OD of the positive control − mean OD of the negative control). In total, each sample run took <4 h.
Detection of specific IgG, IgM, and IgA.
IgG antibodies were titrated using a high-sensitivity direct-agglutination (HSDA) method (16). The positivity cutoff was 10 HSDA U/ml.
IgM and IgA antibodies were detected with an immunocapture (IC) method based on revelation with a suspension of T. gondii (ICT-M and ICT-A) (6). The results were expressed as agglutination scores, ranging from 0 to 12. The positivity cutoff in ICT-M was 1 for newborns and 9 for adults; values between 6 and 8.5 were considered indeterminate because of possible interference by natural IgM (15). The positivity cutoffs in ICT-A were 1 for newborns and 2 for adults. The results of both assays were read automatically (2).
CIP-ELIFA.
The comparative immunological profile-enzyme-linked immunofiltration assay (CIP-ELIFA) technique uses microporous cellulose acetate membranes (13). Briefly, the antigen and three serum samples are deposited side by side and subjected to rapid immunoelectrodiffusion. Precipitant arcs are detected and characterized by immunofiltration with enzyme-conjugated anti-human IgG, IgM, IgA, or IgE antibodies. The detection of IgG neoantibodies is as reliable as detection of IgM or IgA antibodies for neonatal diagnosis of congenital infection (12).
RESULTS
Reproducibility and repeatability: IgE index positivity cutoff.
To determine the reproducibility of the IgE ELISA method, 50 sera (30 positive and 20 negative) were tested on several consecutive days. Similar, accurate (positive-negative) results were obtained for each sample on the different days. The mean values of negative and positive controls were 0.065 (standard deviation, 0.008) and 1.850 (standard deviation, 0.201), respectively. Within-run repeatability was satisfactory (80 and 95%, respectively, for controls with IgE indices of 2 and 1), permitting comparison of IgE indices between stored sera from a given subject and between different types of samples (cord blood, day zero neonatal serum, and day zero postdelivery maternal sera) processed in the same run. On the basis of the control group values, IgE indices of 0.5 or more were considered positive, with a “gray zone” between 0.3 and 0.5.
Toxoplasmic seroconversion during pregnancy (group A1).
Table 1 shows mean IgG, IgM, IgA, and IgE values according to the estimated date of infection. During maternal primary infection, IgE emerged at the same time as IgM and IgA, peaking 3 months after the estimated date of infection. The peak was brief, lasting <1 month, and was always followed by rapid diminishing of IgE.
TABLE 1.
Toxoplasmic seroconversion during pregnancya
| Time after infection | Titerb
|
No. of sera | |||
|---|---|---|---|---|---|
| IgG Abc (HSDA/U/ml) | IgM Ab | IgA Ab | IgE Ab (index) | ||
| 15 days | 16 ± 33 | 11.1 ± 1.6 | 4.8 ± 3.9 | 0.39 ± 0.58 | 61 |
| 1 mo | 339 ± 571 | 11.6 ± 0.7 | 7.5 ± 3.5 | 0.85 ± 0.95 | 68 |
| 2 mo | 790 ± 829 | 11.5 ± 0.8 | 8.0 ± 3.4 | 1.26 ± 0.95 | 70 |
| 3 mo | 1,165 ± 970 | 11.3 ± 0.9 | 8.0 ± 3.6 | 1.37 ± 0.97 | 48 |
| 4 mo | 1,100 ± 1,240 | 11.1 ± 1 | 6.9 ± 3.8 | 1.17 ± 0.87 | 43 |
| 5 mo | 1,300 ± 2,054 | 11.2 ± 1 | 6.7 ± 3.9 | 1.1 ± 1.32 | 33 |
| 6 mo | 1,106 ± 2,304 | 10.1 ± 2.2 | 6.8 ± 3.3 | 0.65 ± 0.47 | 11 |
| 7 mo | 630 ± 934 | 10.9 ± 1.5 | 6.7 ± 3.5 | 0.5 ± 0.45 | 12 |
| 8 mo | 525 ± 536 | 10.7 ± 1.9 | 5.4 ± 3.5 | 0.37 ± 0.22 | 21 |
| 9 mo | 740 ± 922 | 10.9 ± 1.1 | 5.5 ± 3.5 | 0.39 ± 0.17 | 27 |
| 12 mo | 465 ± 831 | 10.1 ± 2.9 | 5.2 ± 4 | 0.25 ± 0.19 | 13 |
| 15 mo | 94 ± 123 | 10.5 ± 1.9 | 5.4 ± 2.3 | 0.29 ± 0.12 | 10 |
IgG (HSDA), IgM and IgA (ICT), and IgE (ELISA) levels in 104 pregnant women with toxoplasmic seroconversion (group A1; 417 sera) were calculated; results were grouped according to the estimated date of infection.
Values are means ± standard deviations. IgM and IgA Ab results are agglutination scores (maximum score, 12).
Ab, antibody.
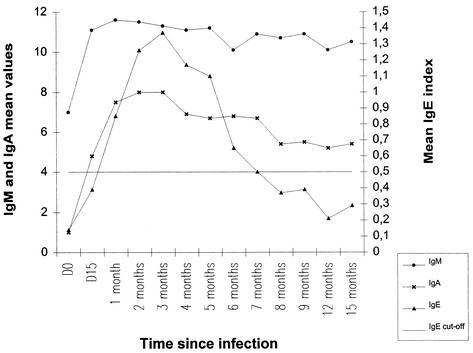
Figure 1 shows IgG, IgM, IgA, and IgE antibody values according to the estimated date of infection in pregnant women. The IgE index increased later in 5 untreated women than in 57 spiramycin-treated women.
FIG. 1.
Kinetics of IgM and IgA (ICT; respective positivity cutoffs, 9 and 2) and IgE (ELISA) in 104 women infected during pregnancy (group A1).
Symptomatic primary infection outside of pregnancy (group A2).
The IgE index increased early, becoming positive 15 days after the estimated date of infection and peaking between 2 and 3 months. All the patients in this group had clinical signs (adenopathies, meningitis, pneumonia, splenomegaly, or disseminated infection) and were treated. Seroconversion was always accompanied by the presence of IgA and IgE. Three of these patients (patients 105, 106, and 110) had particularly high IgE indices (>4); the index fell below the cutoff only after 12 to 18 months, while IgM and IgA persisted at that time.
Serological toxoplasmic reactivation (group A3).
Toxoplasmic reactivation in four women was accompanied by an increase in the IgG titer and emergence of IgA. In two cases, specific IgE appeared transiently, concomitantly with the increase in IgG. IgM values were negative or indeterminate in all these patients.
Immunity acquired before pregnancy (group A4).
Fifteen of the 49 women who were infected before conceiving were sampled twice. The results confirmed stable, long-standing immunity (IgG positive and stable; IgM and IgA negative). Specific IgE was absent in all these cases (IgE index < 0.2). The other women (n = 34) had at least three samples to confirm that the seroconversion occurred prior to conception. In these cases, IgM and/or IgA persisted despite stable or diminishing IgG levels. The IgE index was negative in 25 patients and positive in the other 9 women, in whom IgM and IgA were also detected: in 7 of these 9 cases, infection was estimated to have occurred <2 months before conception.
Negative controls (group A5).
The mean IgE index was 0.08, with values above 0.20 and a standard deviation of 0.03.
Kidney graft recipients (group A6).
Six men (12 sera) and four women (16 sera) had long-standing immunity, with mean IgG, IgM, IgA, and IgE antibody titers of 960 HSDA U/ml, 4.5/12, 4.5/12, and 0.15, respectively. Serological reactivation occurred during posttransplant follow-up in three other women (patients 304, 305, and 308; 31 sera), in whom the emergence of IgE antibody and the increase in the IgE index coincided with the rise in IgG.
Infants with congenital toxoplasmosis (group I+).
For the 42 infants <3 months of age and congenitally infected, maternal seroconversion occurred during the third, second, and first trimesters in 18, 10, and 2 cases, respectively, while the date of maternal seroconversion was not known in the other 12 cases. Twenty-five had IgE indices of ≥0.5 during the first weeks of life. Eleven of these 25 infants had neonatal IgE indices at least equal to the maternal IgE index at delivery. Three (patients 322, 325, and 329) of the five infants with IgE indices above 2 had clinical signs of toxoplasmosis (chorioretinitis, retinal pigmentation, or intracranial calcifications). Twenty-four of these 25 infants had positive IgG titers, but IgM and IgA were strictly negative in two cases. In the last child (patient 376), in whom IgG was not detected at birth (maternal seroconversion and fetal infection occurred at the end of pregnancy), IgM, IgA, and IgE were present at birth, while IgG emerged later.
During their follow-up, 26 other infants had an immunological rebound on treatment withdrawal that generally was programmed between 1 and 2 years. Eight of these 26 rebounds were not accompanied by a significant increase in IgE, while 1 was accompanied by a threefold increase in the IgE index, which nevertheless remained below the positivity cutoff. The IgE index increased from negative to at least 0.5 in 17 cases. IgM and/or IgA were positive in only 15 cases. A significant rise in IgE occurred at the same time as the increase in IgG in 16 cases and later in 2 cases. After the serological rebound, specific IgE levels fell earlier than IgG levels in four infants, simultaneously in five infants, and later in five infants. No samples were obtained after the posttreatment rebound in four cases.
Infants free of congenital toxoplasmosis (group I−).
The mean IgE index at birth was below the positivity cutoff, but individual values showed a very wide range (0.01 to 3.78). The IgE index never exceeded 0.5 after 2 months of life. Thirty infants free of congenital toxoplasmosis had positive IgE indices at birth. Maternal seroconversion occurred close to conception in 10 cases and in the first, second, and third trimesters in 4, 2, and 1 cases, respectively. The date of maternal seroconversion was unknown in 13 cases. Twenty-two of the 344 infants in this group who had negative IgE indices at birth had specific IgM and/or IgA of maternal origin.
For diagnosis of congenital infection, the sensitivities of IgM, IgA, and IgE were, 64.3, 76.2, and 59.7%, respectively; the sensitivity of a combination of the three isotypes (IgM + IgA + IgE) was 81%. The specificities were 96.8% for IgM, 88% for IgA, and 91.9% for IgE. Table 2 summarizes the data for infants.
TABLE 2.
Presence of IgM, IgA, and IgE in blood of infants < 3 months old with (group I+) and without (group I−) congenital toxoplasmosis
| Ig (assay) | Presencea | No. in group I + (n = 42) | Mean valuec | No. in group I − (n = 374) | Mean valuec | Total no. | Sensitivity (%) | Specificity (%) |
|---|---|---|---|---|---|---|---|---|
| IgM (ICT) | − | 15 | 6.3 | 362 | 0.1 | 377 | 64.3 | 96.8 |
| + | 27 | 12 | 37 | |||||
| IgA (ICT) | − | 10 | 6.4 | 329 | 0.2 | 339 | 76.2 | 88 |
| + | 32 | 45 | 77 | |||||
| IgE (ELISA) | − | 17 | 0.85b | 344 | 0.22b | 361 | 59.5 | 91.9 |
| + | 25 | 30 | 55 |
−, absent; +, present.
Index.
Maximum possible value, 12.
Cord blood at birth (group C).
Table 3 compares the mean values of the IgE index and other Ig titers in the cord blood of infants with (group C+) or without (group C−) congenital toxoplasmosis and shows IgM, IgA, and IgE sensitivity and specificity rates for the cord blood.
TABLE 3.
Presence of IgM, IgA, and IgE in cord blood at birth in infants with (group C+) and without (group C−) congenital toxoplasmosis
| Ig (assay) | Presencea | No. in group C+ (n = 15) | Mean value | No. in group C− (n = 132) | Mean value | Total no. | Sensitivity (%) | Specificity (%) |
|---|---|---|---|---|---|---|---|---|
| IgM (ICT) | − | 7 | 6.2c | 116 | 0.7c | 123 | 53.3 | 87.4 |
| + | 8 | 16 | 24 | |||||
| IgA (ICT) | − | 3 | 6.1c | 102 | 0.8c | 105 | 80 | 77.3 |
| + | 12 | 30 | 42 | |||||
| IgE (ELISA) | − | 8 | 0.61b | 112 | 0.35b | 120 | 46.6 | 84.8 |
| + | 7 | 20 | 27 |
−, absent; +, present.
Index.
Maximum possible value, 12.
DISCUSSION
The aim of this study was to determine the value of IgE as a complementary specific marker of Toxoplasma infection, measured using a double sandwich ELISA method based on anti-P30 monoclonal antibody. In previous studies, specific IgE detection was based on the use of a suspension of T. gondii (1, 10, 14, 18, 22) and was highly dependent on the conditions of antigen preparation (time of tachyzoite collection after intraperitoneal inoculation, trypsin and formaldehyde treatment, etc.). The present ELISA technique is more reliable, as shown by its good repeatability and reproducibility. It is also more rapid (4 versus 24 h) and easier to interpret and can be automated.
The specificity of this technique was validated on samples from seronegative patients (mean IgE index, 0.08; standard deviation, 0.03), confirming the absence of cross-reacting natural IgE (10, 14, 18, 22). The sensitivity of IgE detection for seroconversion was 85.7% in our study of 121 patients, a figure very similar to that obtained by Villena et al. (86.6%) in 52 patients (18). Wong et al. obtained a sensitivity of 100%, but in a series of only eight patients (22). It should be noted that 12 of our patients whose IgE indices remained below the positivity cutoff (0.5) nonetheless had a threefold increase in the index during follow-up. IgE was not detected in another 17 patients, possibly because treatment was started very rapidly or because the samples failed to coincide with the transient emergence of this isotype. Indeed, closely spaced samples show a peak at 3 months that lasts ∼1 month, whereas IgM and, to a lesser degree, IgA show a fairly lengthy plateau. Close serological monitoring of pregnant women at risk might enable this IgE peak to be identified, which would be invaluable for dating the infection and estimating the risk for the fetus. It is noteworthy in this respect that IgE remains detectable for longer with this ELISA method than with the previously described nonenzymatic technique (1, 10, 14, 18). Finally, the IgE index showed strong interindividual variability in the different patient subgroups.
The IgE index was higher during symptomatic acquired toxoplasmosis (group A2) and peaked very early (1 month). IgE was detected in all these patients, who had adenopathies, fever, or fatigue, and also lymphocytic meningitis in two cases (patients 105 and 106) and splenomegaly in one case (patient 113). Ashburn et al., Villena et al., and Wong et al. (1, 18, 22) also found very high IgE titers in a group of patients with toxoplasmic adenopathies. These concordant results confirm the value of toxoplasmic IgE serology in etiologic investigation of lymphadenopathies. One patient with severe manifestations (patient 106) had a major antibody response, with an IgG titer of 100,000 HSDA U/ml; 8 months after seroconversion, the IgE index was still above 4, despite very early specific treatment. The manifestations and history of this patient resembled those of another patient infected by a previously undescribed toxoplasmic strain in French Guyana (M. L. Darde, I. Villena, J. M. Pinon, and I. Beguinot, Letter, J. Clin. Microbiol. 36:324, 1998). Villena et al. (18) reported IgE persistence for >6 months in patients with cervical adenopathies. During toxoplasmic reactivation in immunodepressed adults (three kidney graft recipients in group A6) and in four immunocompetent women (group A3), the emergence and increase in IgE coincided with those of IgG, and IgE disappeared more rapidly in five of these seven patients. Detection of IgE, therefore, seems to correlate with toxoplasmic reactivation, as previously reported by Gross et al. (10).
In women who gave birth, regardless of whether their infants had congenital toxoplasmosis, the mean kinetic pattern of specific IgE was very similar to those of women in groups A1 and A2 combined (seroconversion during and outside of pregnancy). IgE detection by ELISA during pregnancy, therefore, is not predictive of congenital transmission, confirming a previous study (18). Likewise, our results suggest that IgE detection in cord blood at birth is not a reliable predictor of congenital infection.
In infants with congenital toxoplasmosis, the mean IgE index was above the positivity cutoff at birth, falling below this threshold value after ∼2 months. In contrast, the mean IgE index was always negative in infants who were free of congenital toxoplasmosis. In infants with congenital toxoplasmosis, specific IgE positivity was less frequent at birth than IgM and IgA positivity (respective sensitivities, 59.5, 64.3, and 76.2%). Specific IgE was the sole positive marker at birth in two infants with congenital toxoplasmosis; one had a positive antenatal diagnosis, while in the other child the diagnosis was only confirmed at age 1 month by CIP-ELIFA detection of neoantibodies. Thus, IgE can be valuable, in combination with IgM-IgA CIP-ELIFA, for neonatal diagnosis of some cases of congenital toxoplasmosis. Interestingly, IgE was found at birth in infants with congenital toxoplasmosis whose mothers had been infected during the first trimester of pregnancy, a situation in which maternal transmission to the fetus is thought to occur early. Given its generally short-lived nature, the presence of IgE at birth points to recent fetal synthesis resulting from late maternal transmission, or placental passage (during delivery) of long-lived maternal IgE (7, 11). Maternofetal treatment had no clear influence on neonatal IgE detection. Naessens et al. came to the same conclusion regarding IgM and IgA in a multicenter study (11). The diagnostic value of IgE detection at birth is slightly better than that of IgA but lower than that of IgM (respective specificities, 91.9, 88, and 96.8%). In the neonatal period, the IgE index was positive in 30 infants who were free of congenital toxoplasmosis. The index fell below the positivity cutoff by day 10 in all these infants but one (patient 384), in whom it remained positive until 2 months of age; it is noteworthy that this child's mother had a particularly high IgE index (>4). The presence of anti-Toxoplasma IgE in these uninfected infants may correspond to maternal antibodies which, as documented for IgA (6) and IgM (12), may cross the damaged placental barrier; these specific maternal IgE antibodies are readily detectable when the relative nonspecific IgE concentration is very low in newborns. As with IgM and IgA, the presence of IgE at birth must therefore be confirmed on a sample obtained on day 10.
Infants with congenital toxoplasmosis and a positive neonatal IgE index must receive very close clinical monitoring. Wong et al. (22) and Pinon et al. (12) detected IgE in 54 and 46%, respectively, of infants with toxoplasmic chorioretinitis. In some of these cases, the IgE index was positive 11, 12, and even 14 months after birth in infants with poor adherence to treatment. IgE assay could therefore help with treatment monitoring: emergence of specific IgE would indicate drug assay to avoid the risks linked to poor postnatal treatment adherence or inadequate dosing (5, 19). After treatment cessation, 69% of serological rebounds were accompanied by a significant increase in IgE, concomitantly with IgG and sometimes without IgM or IgA. As in acquired toxoplasmosis, IgE appears to be a better immunological marker of rebound than IgM and IgA. Routine screening for serological rebound could thus be restricted to IgE assay and to IgG assay by CIP-ELIFA.
Conclusion.
The ELISA method used here has several technical advantages over immunocapture with a tachyzoite suspension. The results of this study confirm the clinical relevance of the IgE assay. The absence of natural IgE, together with the early emergence of specific IgE during seroconversion, its brief peak between 2 and 3 months after infection, and its shorter kinetics relative to IgM and IgA make specific IgE antibodies a useful complementary tool for fine dating of seroconversion. The persistence of specific IgE several months after seroconversion is suggestive of active toxoplasmosis and should be taken into account in the risk assessment both during pregnancy and prior to conception (20, 21). Specific IgE is almost always present in symptomatic acquired toxoplasmosis and can thus contribute to the etiologic diagnosis of lymphadenopathies.
IgE assay can also contribute to neonatal diagnosis of congenital toxoplasmosis, although the possibility of sample contamination by maternal antibodies means that a positive result must be confirmed on day 10 of life, as recommended for IgM and IgA. The emergence of IgE antibodies in a child on treatment is a marker of poor adherence or inadequate dosing.
Acknowledgments
This work was supported by the Programme Hospitalier de Recherche Clinique (1995 to 2001), Ministère de la Santé, Paris, France.
We thank D. Young for translating the French manuscript.
REFERENCES
- 1.Ashburn, D., A. W. Joss, T. H. Pennington, and D. O. Ho-Yen. 1995. Specificity and usefulness of an IgE immunosorbent agglutination assay for toxoplasmosis. J. Clin. Pathol. 48:64-69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Aubert, D., F. Foudrinier, M. L. Kaltenbach, D. Guyot-Walser, C. Marx-Chemla, R. Geers, H. Lepan, and J. M. Pinon. 1995. Automated reading and processing of quantitative IgG, IgM, IgA and IgE isotypic agglutination results in microplates. Development and application in parasitology-mycology. J. Immunol. Methods 186:323-328. [DOI] [PubMed] [Google Scholar]
- 3.Couvreur, J. 1999. Problems of congenital toxoplasmosis. Evolution over four decades. Presse Med. 28:753-757. [PubMed] [Google Scholar]
- 4.Decoster, A., F. Darcy, A. Caron, and A. Capron. 1988. IgA antibodies against P30 as markers of congenital and acute toxoplasmosis. Lancet ii:1104-1107. [DOI] [PubMed]
- 5.Fortier, B., C. Coignard-Chatain, A. Dao, V. Rouland, A. S. Valat, D. Vinatier, and T. Lebrun. 1997. Study of developing clinical outbreak and serological rebounds in children with congenital toxoplasmosis and follow-up during the first 2 years of life. Arch. Pediatr. 4:940-946. [DOI] [PubMed] [Google Scholar]
- 6.Foudrinier, F., C. Chemla, D. Aubert, A. Bonhomme, and J. M. Pinon. 1995. Value of specific immunoglobulin A detection by two immunocapture assays in the diagnosis of toxoplasmosis. Eur. J. Microbiol. Infect. Dis. 14:585-590. [DOI] [PubMed] [Google Scholar]
- 7.Foulon, W., J. M. Pinon, B. Stray-Pedersen, A. Pollak, M. Lappalainen, A. Decoster, I. Villena, P. A. Jenum, M. Hayde, and A. Naessens. 1999. Prenatal diagnosis of congenital toxoplasmosis: a multicenter evaluation of different diagnostic parameters. Am. J. Obstet. Gynecol. 181:843-847. [DOI] [PubMed] [Google Scholar]
- 8.Francis, J. M., and D. H. Joynson. 1993. Duration of specific immunoglobulin A antibody following acute toxoplasmosis as determined by enzyme immunoassay and immunosorbent agglutination assay. Eur. J. Microbiol. Infect. Dis. 12:556-559. [DOI] [PubMed] [Google Scholar]
- 9.Gorgievski-Hrisoho, M., D. Germann, and L. Matter. 1996. Diagnostic implications of kinetics of immunoglobulin M and A antibody responses to Toxoplasma gondii. J. Clin. Microbiol. 34:1506-1511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gross, U., O. Keksel, and M. L. Dardé. 1997. Value of detecting immunoglobulin E antibodies for the serologic diagnosis of Toxoplasma gondii infection. Clin. Diagn. Lab. Immunol. 4:247-251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Naessens, A., P. A. Jenum, A. Pollak, A. Decoster, M. Lappalainen, I. Villena, M. Lebech, B. Stray-Pedersen, M. Hayde, J. M. Pinon, and W. Foulon. 1999. Diagnosis of congenital toxoplasmosis in the neonatal period: a multicenter evaluation. J. Pediatr. 135:714-719. [DOI] [PubMed] [Google Scholar]
- 12.Pinon, J. M., H. Dumon, C. Chemla, J. Franck, E. Petersen, M. Lebech, J. Zufferey, M. H. Bessieres, P. Marty, R. Holliman, J. Johnson, V. Luyasu, B. Lecolier, E. Guy, D. H. M. Joynson, A. Decoster, G. Enders, H. Pelloux, and E. Candolfi. 2001. Strategy for diagnosis of congenital toxoplasmosis: evaluation of methods comparing mothers and newborns and standard methods for postnatal detection of immunoglobulin G, M, and A antibodies. J. Clin. Microbiol. 39:2267-2271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Pinon, J. M., H. Thoannes, and N. Gruson. 1985. An enzyme-linked-immuno-filtration-assay used to compare infant and maternal antibody profiles in toxoplasmosis. J. Immunol. Methods 77:15-23. [DOI] [PubMed] [Google Scholar]
- 14.Pinon, J. M., D. Toubas, C. Marx, G. Mougeot, A. Bonnin, A. Bonhomme, M. Villaume, F. Foudrinier, and H. Lepan. 1990. Detection of specific immunoglobulin E in patients with toxoplasmosis. J. Clin. Microbiol. 28:1739-1743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Potasman, I., F. G. Araujo, and J. S. Remington. 1986. Toxoplasma antigens recognized by naturally occurring human antibodies. J. Clin. Microbiol. 24:1050-1054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Puygauthier-Toubas, D., D. Jolly, O. Bajolet, T. Moreaux, C. Marx-Chemla, A. Bonhomme, F. Blanchard, and J. M. Pinon. 1990. Comparative study of anti-toxoplasma IgG isotypes titrated by high sensitivity direct agglutination and indirect immunofluorescence: consequence of the choice of methods on the expression of results in international units. Ann. Biol. Clin. 48:737-741. [PubMed] [Google Scholar]
- 17.Suzuki, L. A., R. J. Rocha, and C. L. Rossi. 2001. Evaluation of serological markers for the immunodiagnosis of acute acquired toxoplasmosis. J. Med. Microbiol. 50:62-70. [DOI] [PubMed] [Google Scholar]
- 18.Villena, I., D. Aubert, V. Brodard, C. Quéreux, B. Leroux, D. Dupuy, G. Remy, F. Foudrinier, C. Chemla, J. E. Gomez-Marin, and J. M. Pinon. 1999. Detection of specific IgE during maternal, fetal, and congenital toxoplasmosis. J. Clin. Microbiol. 37:3487-3490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Villena, I., D. Aubert, B. Leroux, D. Dupouy, M. Talmud, C. Chemla, T. Trenque, G. Schmit, C. Quereux, M. Guenounou, M. Pluot, A. Bonhomme, and J. M. Pinon. 1998. Pyrimethamine-sulfadoxine treatment of congenital toxoplasmosis: follow-up of 78 cases between 1980 and 1997. Scand. J. Infect. Dis. 30:295-300. [DOI] [PubMed] [Google Scholar]
- 20.Villena, I., C. Chemla, C. Quereux, D. Dupouy, B. Leroux, F. Foudrinier, and J. M. Pinon. 1998. Prenatal diagnosis of congenital toxoplasmosis transmitted by an immunocompetent woman infected before conception. Prenat. Diagn. 18:1079-1081. [PubMed] [Google Scholar]
- 21.Vogel, N., M. Kirisits, E. Michael, H. Bach, M. Hostetter, K. Boyer, R. Simpson, E. Holfels, J. Hopkins, D. Mack, M. B. Mets, C. N. Swisher, D. Patel, N. Roizen, L. Stein, M. Stein, S. Withers, E. Mui, C. Egwuagu, J. Remington, R. Dorfman, and R. McLeod. 1996. Congenital toxoplasmosis transmitted from an immunologically competent mother infected before conception. Clin. Infect. Dis. 23:1055-1066. [DOI] [PubMed] [Google Scholar]
- 22.Wong, S. Y., P. Hadju, R. Ramirez, P. Thulliez, R. MacLeod, and J. S. Remington. 1993. Role of specific immunoglobulin E in diagnosis of acute Toxoplasma infection and toxoplasmosis. J. Clin. Microbiol. 31:2952-2959. [DOI] [PMC free article] [PubMed]