Abstract
1. Exposure to glass of whole blood from anaesthetized foetal lambs (at 0·6-0·95 of term) causes the rapid development of a potent pulmonary vasodilator agent.
2. The formation of the vasodilator agent on exposure to glass, its disappearance with time, and the inhibition of its production by soya bean trypsin inhibitor, suggest that it is bradykinin.
3. Small doses of bradykinin (∼ 1 ng/kg) cause pulmonary vasodilatation on close arterial injection. Neither this, nor the vasodilatation caused by glass-exposed whole blood, are affected by agents which block the vasodilator actions of acetylcholine, isoprenaline or histamine.
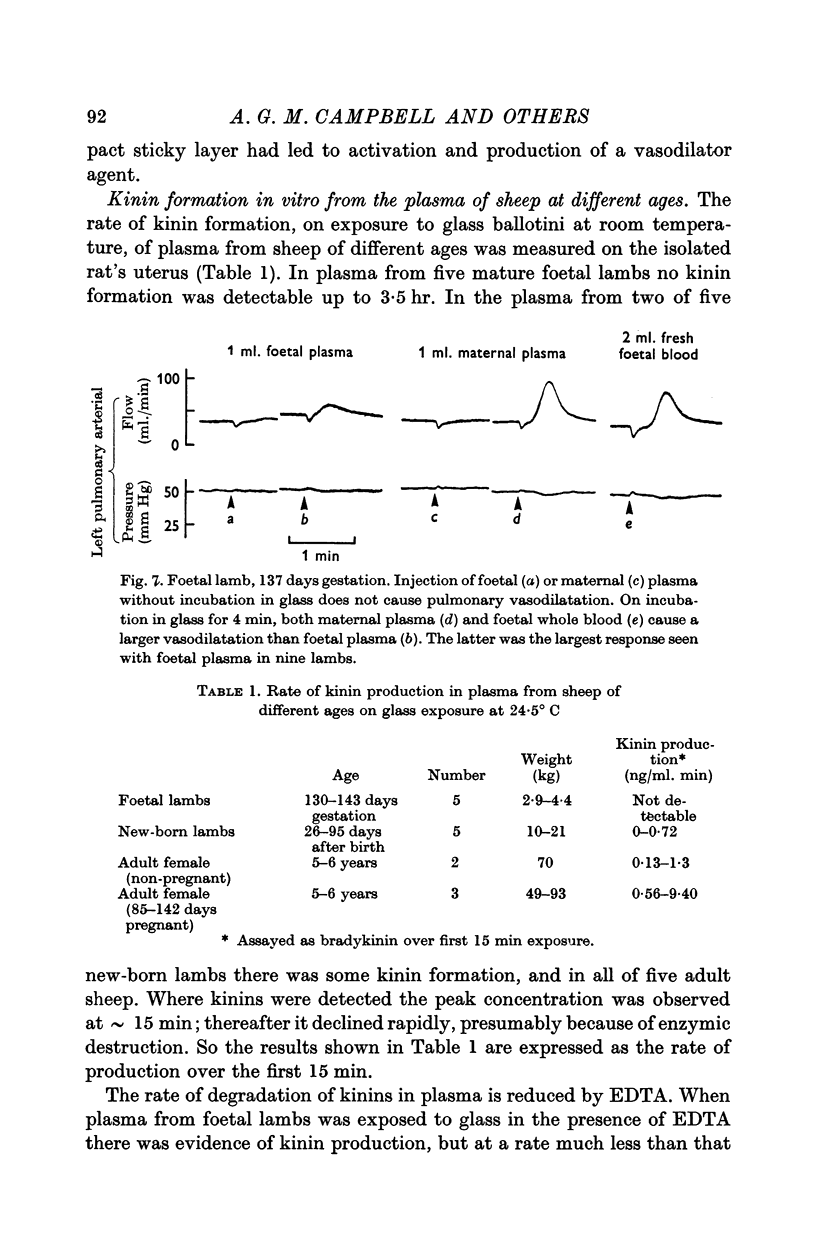
4. Exposure of foetal plasma and/or red cells to glass rarely caused the development of a pulmonary vasodilator agent. Maternal plasma was always active. Injection of the buffy coat from foetal blood caused pulmonary vasodilatation.
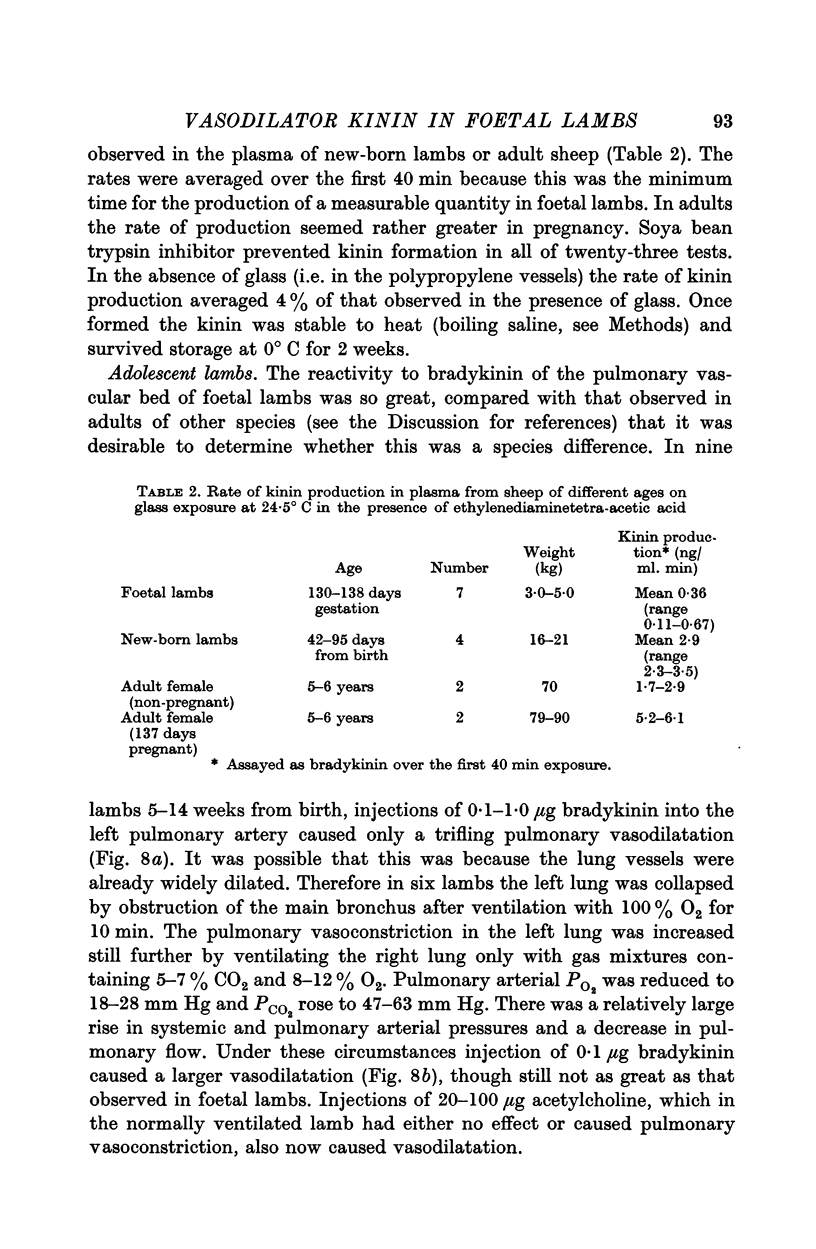
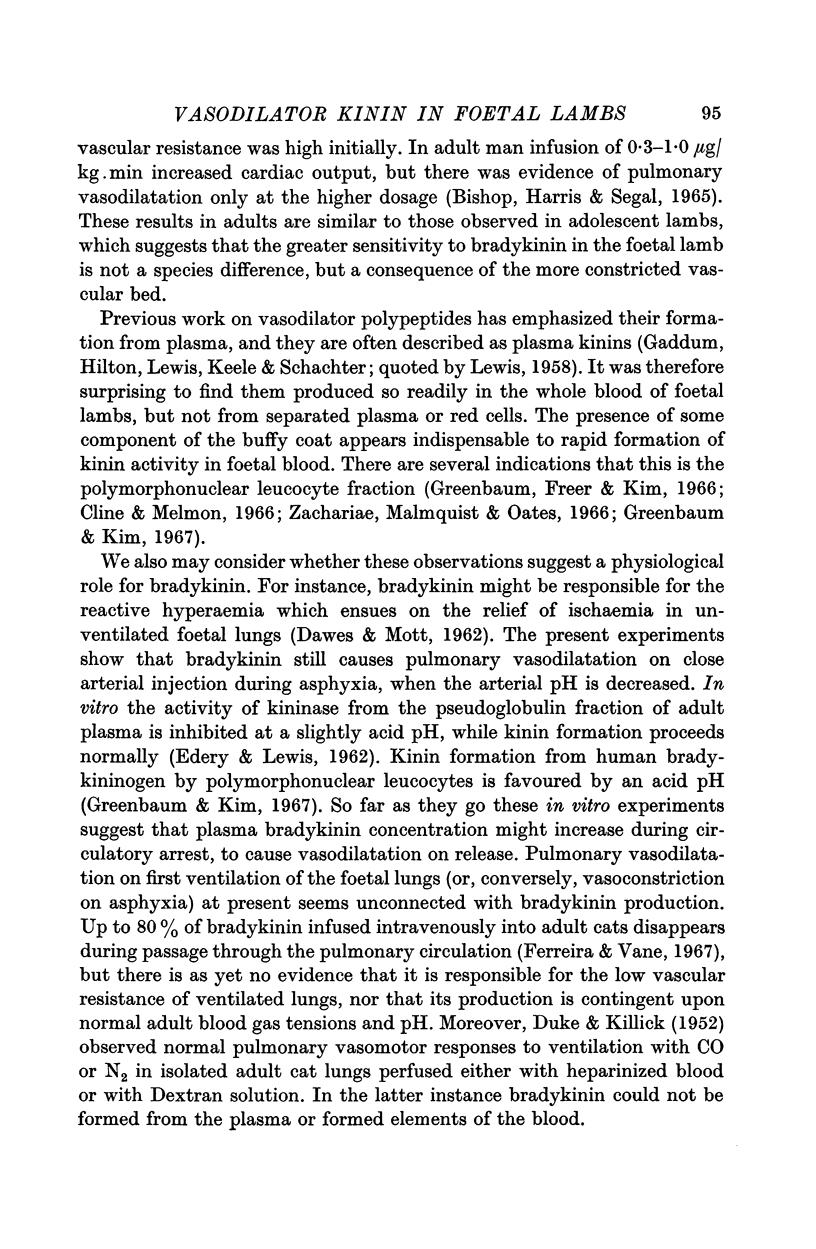
5. The capacity of plasma from sheep at different ages to produce kinin(s) was examined by assay on the isolated rat's uterus. In the foetus activity was very low; it increased with age.
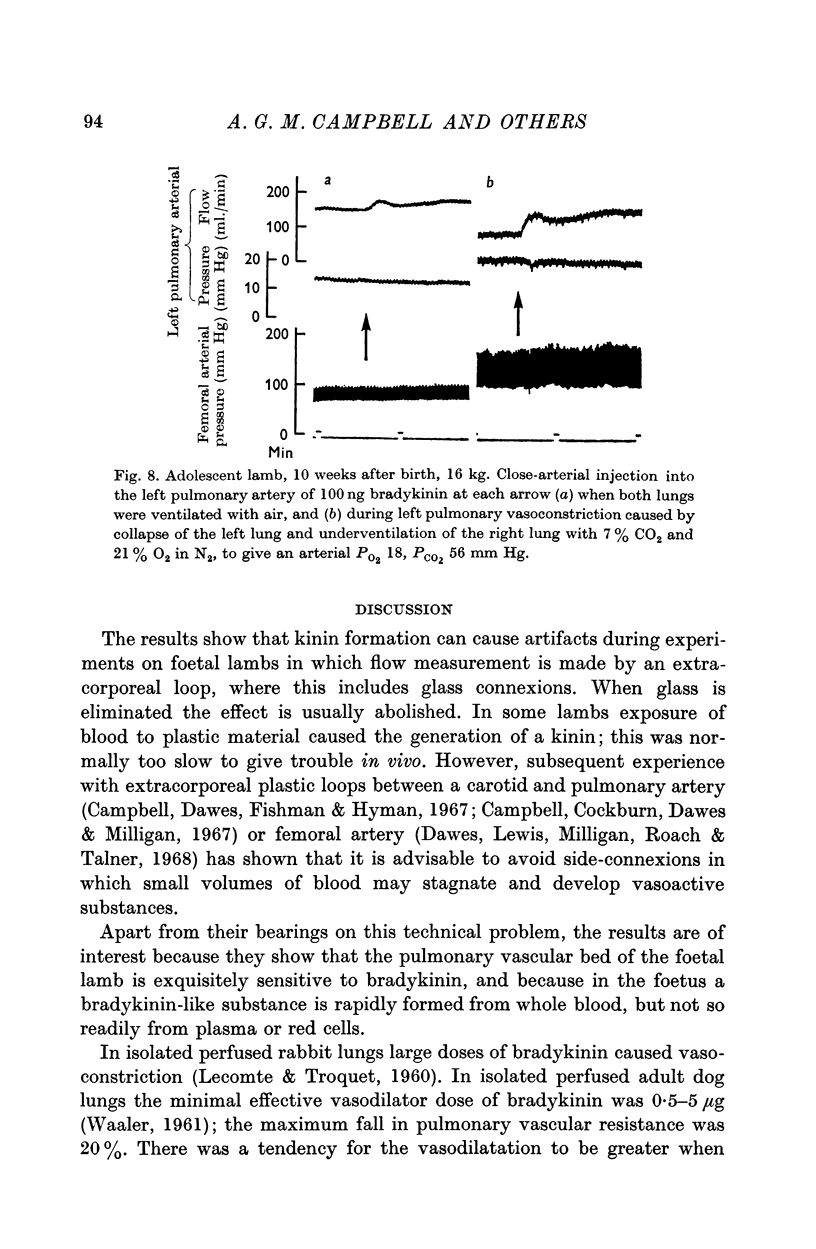
6. In adolescent lambs 5-14 weeks after birth injection of ∼ 10 ng/kg bradykinin into the pulmonary artery caused only a trifling vasodilatation; this was greater when pulmonary vasoconstriction was induced by lung collapse, hypoxaemia and hypercapnia.
7. The possible physiological consequences of these findings are discussed.
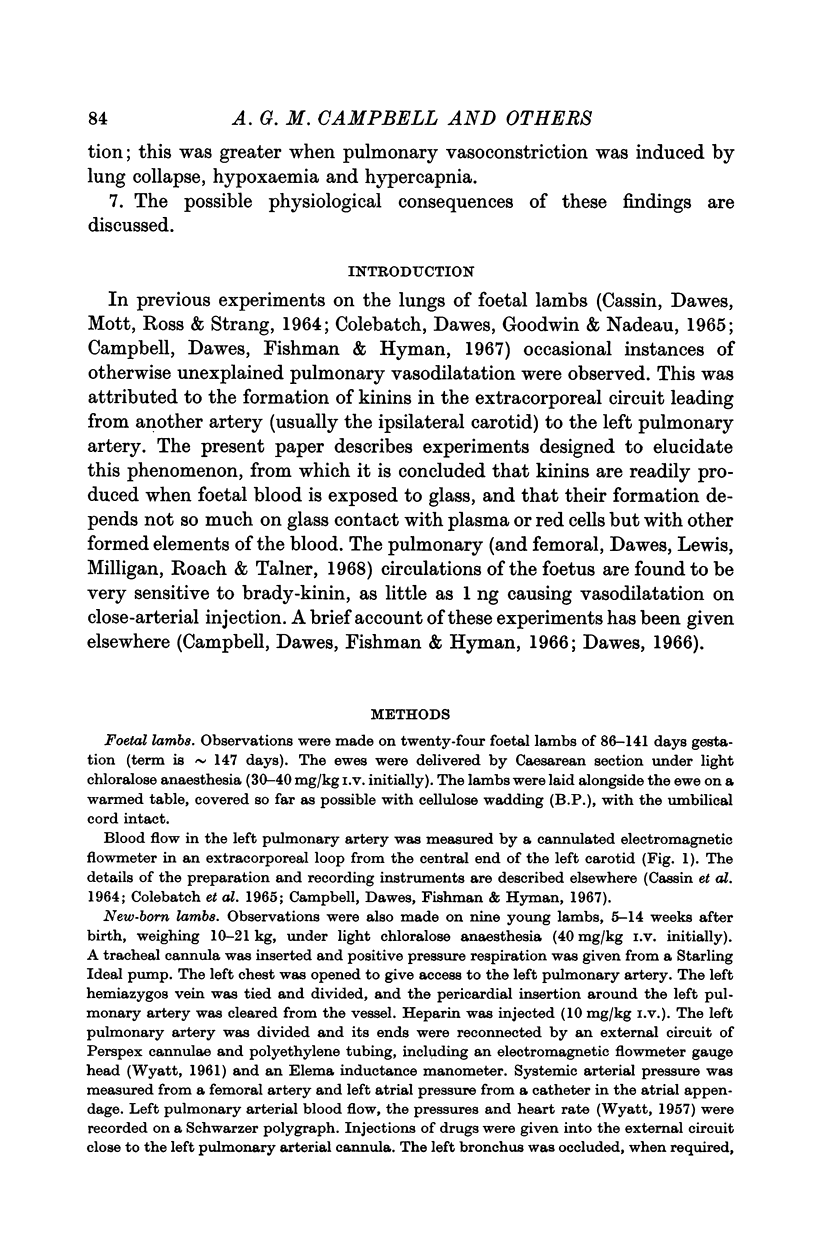
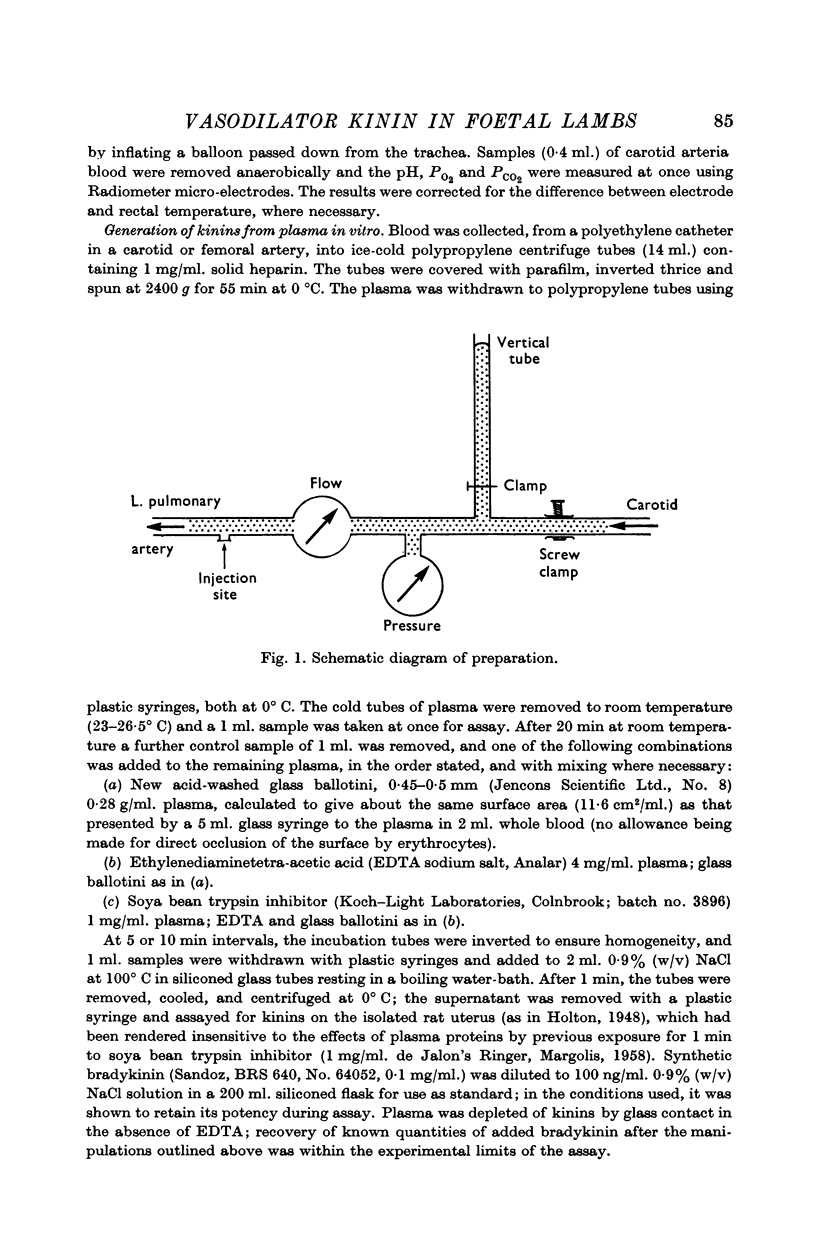
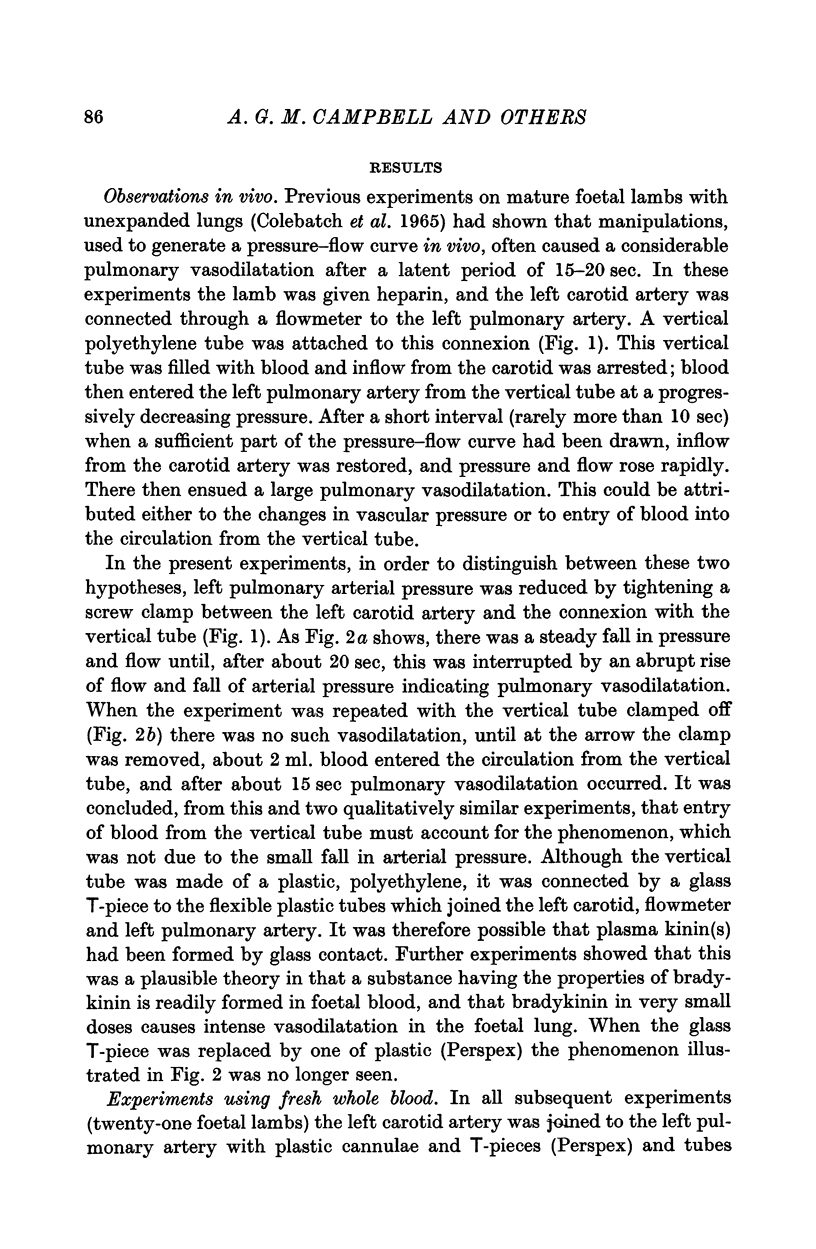
Full text
PDF
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Bishop J. M., Harris P., Segel N. The circulatory effects of bradykinin in normal subjects and patients with chronic bronchitis. Br J Pharmacol Chemother. 1965 Oct;25(2):456–469. doi: 10.1111/j.1476-5381.1965.tb02064.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- CASSIN S., DAWES G. S., MOTT J. C., ROSS B. B., STRANG L. B. THE VASCULAR RESISTANCE OF THE FOETAL AND NEWLY VENTILATED LUNG OF THE LAMB. J Physiol. 1964 May;171:61–79. doi: 10.1113/jphysiol.1964.sp007361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Campbell A. G., Cockburn F., Dawes G. S., Milligan J. E. Pulmonary vasoconstriction in asphyxia during cross-circulation between twin foetal lambs. J Physiol. 1967 Sep;192(1):111–121. doi: 10.1113/jphysiol.1967.sp008291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Campbell A. G., Dawes G. S., Fishman A. P., Hyman A. I. Pulmonary vasoconstriction and changes in heart rate during asphyxia in immature foetal lambs. J Physiol. 1967 Sep;192(1):93–110. doi: 10.1113/jphysiol.1967.sp008290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cline M. J., Melmon K. L. Plasma kinins and cortisol: a possible explanation of the anti-inflammatory action of cortisol. Science. 1966 Sep 2;153(3740):1135–1138. doi: 10.1126/science.153.3740.1135. [DOI] [PubMed] [Google Scholar]
- Colebatch H. J., Dawes G. S., Goodwin J. W., Nadeau R. A. The nervous control of the circulation in the foetal and newly expanded lungs of the lamb. J Physiol. 1965 Jun;178(3):544–562. doi: 10.1113/jphysiol.1965.sp007641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DAWES G. S., MOTT J. C. The vascular tone of the foetal lung. J Physiol. 1962 Dec;164:465–477. doi: 10.1113/jphysiol.1962.sp007032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DUKE H. N., KILLICK E. M. Pulmonary vasomotor responses of isolated perfused cat lungs to anoxia. J Physiol. 1952 Jul;117(3):303–316. doi: 10.1113/jphysiol.1952.sp004750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dawes G. S., Lewis B. V., Milligan J. E., Roach M. R., Talner N. S. Vasomotor responses in the hind limbs of foetal and new-born lambs to asphyxia and aortic chemoreceptor stimulation. J Physiol. 1968 Mar;195(1):55–81. doi: 10.1113/jphysiol.1968.sp008446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ferreira S. H., Vane J. R. The disappearance of bradykinin and eledoisin in the circulation and vascular beds of the cat. Br J Pharmacol Chemother. 1967 Jun;30(2):417–424. doi: 10.1111/j.1476-5381.1967.tb02148.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greenbaum L. M., Kim K. S. The kinin-forming and kininase activities of rabbit polymorphonuclear leucocytes. Br J Pharmacol Chemother. 1967 Feb;29(2):238–247. doi: 10.1111/j.1476-5381.1967.tb01956.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- LECOMTE J., TROQUET J. [Antagonism between bradykinin and phenylbutazone in the rabbit]. C R Seances Soc Biol Fil. 1960;154:1115–1117. [PubMed] [Google Scholar]
- LEWIS G. P. Formation of plasma kinins by plasmin. J Physiol. 1958 Feb 17;140(2):285–300. doi: 10.1113/jphysiol.1958.sp005934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MARGOLIS J. Activation of plasma by contact with glass: evidence for a common reaction which releases plasma kinin and initiates coagulation. J Physiol. 1958 Nov 10;144(1):1–22. doi: 10.1113/jphysiol.1958.sp006082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MARGOLIS J. The mode of action of Hageman factor in the release of plasma kinin. J Physiol. 1960 May;151:238–252. doi: 10.1113/jphysiol.1960.sp006434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- WAALER B. A. The effect of bradykinin in an isolated perfused dog lung preparation. J Physiol. 1961 Aug;157:475–483. doi: 10.1113/jphysiol.1961.sp006737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zachariae H., Malmquist J., Oates J. A. Kininase in human polymorphonuclear leukocytes. Life Sci. 1966 Dec;5(24):2347–2355. doi: 10.1016/0024-3205(66)90072-5. [DOI] [PubMed] [Google Scholar]


