Abstract
Dendritic cells are professional antigen-presenting cells able to initiate innate and adaptive immune responses against invading pathogens. In response to external stimuli dendritic cells undergo a complete genetic reprogramming that allows them to become, soon after activation, natural killer cell activators and subsequently T cell stimulators. The recent observation that dendritic cells produce interleukin 2 following microbial stimulation opens new possibilities for understanding the efficiency of dendritic cells in regulating immune system functions. This review discusses how dendritic cells control natural killer, T- and B-cell responses and the relevance of interleukin 2 in these processes.
Keywords: adaptive immune response/dendritic cells/innate immune response/interleukin 2/regulatory T cells
Introduction
The immune system of vertebrate animals has evolved to respond to different types of perturbations (invading pathogens, stress signals), limiting self-tissue damage. The decision to activate an immune response is made by antigen-presenting cells (APCs) that are quiescent until they encounter a foreign microorganism or inflammatory stimulus. Early activated APCs trigger innate immune responses that represent the first line of reaction against invading pathogens to limit the infections. At later times, activated APCs acquire the ability to prime antigen-specific immune responses that clear the infections and give rise to memory. During the immune response self-tissue damage is limited and tolerance to self is maintained through life.
Among the cells that constitute the immune system, dendritic cells (DCs) play a central role. They are extremely versatile APCs involved in the initiation of both innate and adaptive immunity (Banchereau et al., 2000) and also in the differentiation of regulatory T cells (Steinman and Nussenzweig, 2002) required for the maintenance of self-tolerance.
How DCs can mediate these diverse and almost contradictory functions has recently been investigated. The plasticity of these cells allows them to undergo a complete genetic reprogramming in response to external microbial stimuli, such as inflammatory cytokines, microorganisms or microbial products like lipopolysaccharide (LPS), lipoteichoic acid (LTA), bacterial DNA and double-stranded viral RNA (Granucci et al., 2001b; Huang et al., 2001). Resting immature DCs are highly phagocytic and continuously internalize soluble and particulate antigens that are processed and presented, although inefficiently, to T cells. The interaction of immature DCs with T cells induces an abortive T-cell activation with the induction of T-cell anergy (Hawiger et al., 2001; Sotomayor et al., 2001) or the differentiation of regulatory T cells (Jonuleit et al., 2001). In contrast, microbial stimuli that are recognized through a complex DC innate receptor repertoire induce DC maturation that is completed after 24 h (Granucci et al., 2001b; Huang et al., 2001). Mature DCs express high levels of stable peptide–MHC complexes and costimulatory molecules at the cell surface and efficiently prime naive T cells. The extent and the type of innate and adaptive responses induced by DCs are related to the type of signal they have received (Huang et al., 2001). Indeed, DCs are able to distinguish different pathogens through the expression of pattern-recognition receptors (PRRs) that interact with specific microorganism molecular structures called microbe-associated molecular patterns (PAMPs). These constitutive and conserved microbial structures are absent in host mammalian cells and represent the signature of microorganisms (Medzhitov, 2001). Well-defined PRRs are Toll-like receptors (TLRs). The stimulation of different TLRs at the DC surface results in the activation of different signaling pathways and the induction of diverse maturation processes that influence the outcome of adaptive immunity (Huang et al., 2001).
DC maturation process
Immature DCs reside in peripheral tissue, particularly in skin and mucosae that are sites of interface with the external environment, where they continuously monitor invading microorganisms. The development of culture systems that allow the maintenance and expansion of immature human and mouse DCs (Sallusto and Lanzavecchia, 1994; Winzler et al., 1997) and mimic in vitro the process of DC maturation has enabled large quantities of immature and maturing DCs to be obtained at distinct stages of activation upon encounter with different stimuli. Thus, the process of DC maturation has been described in the mouse and human systems (Granucci et al., 2001b; Huang et al., 2001). Immature DCs are highly phagocytic cells but are quite inefficient in antigen processing and T-cell priming activities. Stimuli that induce DC maturation increase the efficiency of antigen processing for both class I and class II pathways and the half-life of peptide–MHC complexes at the cell surface that otherwise are rapidly internalized and recycled. Thus, large numbers of long-lived peptide-loaded MHC class I and class II molecules persist at the cell surface and render DCs capable of stimulating T cells even after several days (Cella et al., 1997; Pierre et al., 1997; Rescigno et al., 1998).
Kinetic studies of DC maturation have been performed using microarray technology (Granucci et al., 2001a,b). After DC treatment with bacteria or LPS, genes involved in the MHC class I processing pathway were upregulated with precise kinetics. Transcript levels of the PA28 proteasome activator increased 6 h after encounter with LPS, while the transporter of antigen presentation 1 (TAP-1) mRNA upregulation was measurable at later times. These observations were in perfect agreement with the kinetics of new MHC class I molecule biosynthesis, which was described as peaking 18 h after bacterial or LPS stimulation (Rescigno et al., 1998). In contrast, MHC class II genes were already downregulated in both the mouse and human systems 4 h after bacterial and LPS treatment, respectively (Granucci et al., 2001a,b), consistent with the observation that the upregulation of MHC class II protein synthesis is very rapid, peaking as soon as 1 h after DC activation (Rescigno et al., 1998). Finally, in accordance with the described increased stability of peptide–MHC class II complexes at the cell surface of activated DCs, H-2M molecules, which regulate MHC class II loading with antigenic peptides, were downregulated as soon as 6 h after LPS stimulation.
During maturation, DCs lose their phagocytic capacities. This phenomenon, regulated by the actin cytoskeleton, has been associated with the downregulation of the activated form of the small GTPase Cdc42 (Garrett et al., 2000). This GTPase is also implicated, together with Rho and Rac, in determining cytoskeletal architecture in immature human monocyte derived DC. Cdc42, Rho and Rac are involved in the formation of filopodia and podosomes, which are highly specialized adhesion structures important for cell motility, typical of immature DCs and absent in mature DCs (Burns et al., 2001). Moreover, in the mouse system the Vav proteins, which induce typical Rac-1- and RhoG-like cytoskeletal changes including cell spreading, membrane ruffling and the formation of lamellipodia (Borisy and Svitkina, 2000), as well as many genes that modulate the dynamic properties of actin filaments, like fascin and gelsolin, were regulated at the transcription level during maturation (Granucci et al., 2001a).
It is known that activation with bacteria induces DC maturation and survival. Genes that were upregulated early after bacterial encounter which might be involved in DC survival include mouse inhibitor of apoptosis protein 1 (MIAP1), MIAP2, Bcl-x and TNF receptor associated factor 1 (TRAF1) and TRAF2. Conversely, Bcl-2 mRNA was already downregulated 4 h after bacterial stimulation, indicating that it is not involved in maintaining mature DC survival.
During the process of maturation, DCs go through intermediate maturational stages in which they express, with strictly defined kinetics, cytokines and cell surface molecules critical for the initiation and the control of innate and then adaptive immune responses (Langenkamp et al., 2000; Granucci et al., 2001a). In particular, inflammatory products, such as tumor necrosis factor-α (TNF-α), macrophage inflammatory protein-1α (MIP-1α), MIP-1β and MIP-2, are strongly upregulated soon after bacterial interaction with a progressive downregulation, suggesting that the inflammatory activity of DCs mostly takes place early after activation before they have left the inflammatory site. Controlled expression during maturation has also been described for interleukin (IL) 12, which is produced transiently by monocyte-derived DCs following LPS stimulation. After the peak of IL-12 production DCs become refractory to further stimulation. The time-dependent cytokine expression has been associated with different DC functions at different transitional stages after activation. Thus, early activated IL-12-producing DCs would be able to prime T helper cell type 1 (Th1) responses, whereas at later times the same cells would preferentially prime Th2 and non-polarized T cells (Langenkamp et al., 2000).
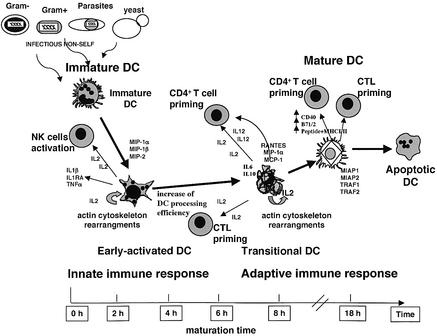
DCs and interleukin 2
Using microarray technology, we have recently found that DCs are able to produce IL-2 upon bacterial encounter (Granucci et al., 2001a). Like the other inflammatory cytokines, IL-2 is expressed with strictly defined kinetics between 2 and 8 h after bacterial uptake. IL-2 is a cytokine which is able to sustain the growth of T, B and natural killer (NK) cells and, during the late phases of antigen-specific T-cell response, it contributes to the maintenance of T-cell homeostasis by promoting activation-induced cell death (AICD) of effector T lymphocytes (Van Parijs et al., 1999). Given the important regulatory role exerted by IL-2 in the immune system, IL-2-deficient mice show a generalized immune system deregulation (Schimpl et al., 2002). The observation that DCs, as well as T cells, can produce IL-2 (Figure 1) opens new possibilities for understanding the mechanisms by which DCs control innate and adaptive immunity (Lebecque, 2001). Only microbial stimuli, and not inflammatory cytokines, are able to induce IL-2 secretion by DCs (Granucci et al., 2003), indicating that DCs can distinguish between the actual presence of an infection and a cytokine-mediated inflammatory process.
Fig. 1. Schematic representation of the DC maturation process. Following a microbial encounter, immature DCs undergo actin cytoskelton rearrangements (which induce downregulation of the phagocytic activity) and increase the efficiency of antigen processing and presentation to prime T cells. Moreover, activated DCs express, with strictly defined kinetics, cytokines and chemokines for activation and control of innate and acquired immune responses. Among the cytokines produced by early activated DCs, IL-2 plays a key role. At early time points, it helps to activate NK cells (IL-2 pathway, see Figure 2). At later time points, when DCs have not yet reached the final stage of maturation and still express low levels of costimulatory molecules and peptide–MHC complexes at the cell surface, DC-derived IL-2 cooperates in the activation of T-cell responses (late adaptive response). The possibility that IL-2 can also act on DC in an autocrine fashion cannot be excluded.
DCs and natural killer cells
NK cells are specialized cells of the innate immune system that exert their functions against pathogen-infected or tumor cells. NK cell activity is primed during the early phases of an immune response, a few hours after infection. A predominant role of DCs in NK cell activation has been described in mouse and human (Moretta, 2002). Both immature and mature human monocyte derived DCs and mouse bone marrow derived DCs have been shown to be able to prime NK cell cytolytic activity (Ferlazzo et al., 2002; Gerosa et al., 2002; Piccioli et al., 2002). This process requires cell-to-cell contact and is independent of IL-12 and IL-2 (Gerosa et al., 2002). DC–NK cell cross-talk is bidirectional since IL-2 activated NK cells induce immature DC activation in terms of upregulation of costimulatory and MHC molecules and production of inflammatory cytokines. Like DC-mediated NK cell activation, NK-mediated DC activation also requires cell-to-cell contact and mediators produced by NK cells and DCs, such as TNF-α (Gerosa et al., 2002). Immature DCs can prime NK cell activity provided that they are cultured in the presence of IL-4, but not if propagated with GM-CSF only (Fernandez et al., 1999). Potential sources of IL-4 in vivo during the early innate phase of the immune response are NKT cells, basophils and mast cells, which have recently been shown to play a critical role in innate immunity to bacterial infections (Galli et al., 1999; Wedemeyer et al., 2000; Henz et al., 2001). Moreover, basophils and mast cells also produce large amounts of TNF-α after bacterial and parasite interaction. TNF-α is an additional cytokine able to confer on DCs the ability to activate NK cells (Fernandez et al., 1999).
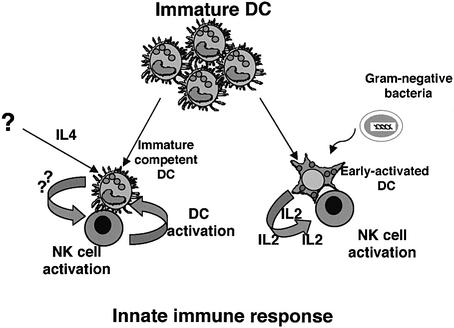
In addition to these new mechanisms for NK cell priming, a classical method of activating NK cells in vitro is culture in the presence of IL-2. However, IL-2-mediated NK cell activation has never been considered to be possible during immunocompetent responses in vivo because it was commonly believed that IL-2 was exclusively produced by T cells during the late phase of the immune response when the peak of interferon-γ (IFN-γ) production by activated NK cells, which occurs during the innate response, was exhausted (Biron et al., 1999). However, as it is now clear that DCs are able to make IL-2 early after infection, at least in the mouse, a possible prediction is that DC-derived IL-2 could be involved in NK cell activation (Moretta, 2002). Bacterially activated DCs are strong inducers of NK cell priming (Ferlazzo et al., 2003), and preliminary data from our laboratory (unpublished observations) suggest that the efficiency of NK cell activation mediated by bacterially activated DCs strongly depends on IL-2 in vitro and in vivo rather than on cell-to-cell contact. Thus, we propose that two possible pathways of NK cell priming by DC may exist, one dependent on IL-4 and the other dependent on microbial stimuli and IL-2. Hence an appropriate cytokine milieu can render DC competent for NK cell activation independently of the presence of microbial stimuli and IL-2; alternatively, following microbial encounter, DCs acquire the ability to activate NK cells with an IL-2-dependent process (Figure 2).
Fig. 2. Two possible pathways for DC-mediated NK cell activation. In the IL-4 pathway, immature DCs become competent NK cell activators in the presence of IL-4. This process is bidirectional and requires cell-to-cell contact and soluble factors. In the IL-2 pathway, early microbial activated DCs, which are IL-2 producers, acquire the ability to stimulate NK cells. This process depends on IL-2 and membrane proteins.
DCs and B cells
DCs have the capacity to regulate B-cell responses directly (Banchereau et al., 2000). As shown in vivo in rats, DCs can capture antigens, maintain them unprocessed and transfer them to naive B cells to initiate antigen-specific responses (Wykes et al., 1998). Upon exposure to IFN-γ, CD40 ligand, LPS or IFN-α, marginal zone DCs upregulate members of the TNF family, B lymphocyte stimulator protein (BlyS) and proliferation-inducing ligand (APRIL). In the presence of IL-4, IL-10 or transforming growth factor-β (TGF-β), BlyS- and APRIL-expressing activated DCs induce class switch recombination to Cγ, Cα and Cε in a CD40-independent manner (Litinskiy et al., 2002). Secretion of immunoglobulin by BlyS- and APRIL-stimulated B cells also requires activation of the surface B-cell receptor. Synergism of BlyS and APRIL with particular cytokines, such as IL-15, is requested for the activation of transcription factors, including NF-κB, that lead to efficient proliferation and antibody production. IL-15 has many overlapping activities with IL-2: it signals through the β and γ subunits of the IL-2 receptor and, exactly like IL-2, costimulates antibody production in CD40-activated B cells (Armitage et al., 1995). IL-2 is also an efficient B-cell growth factor and, given the fact that it is produced by mouse DCs following activation with stimuli, such as CD40L and LPS, that also upregulate the expression of BlyS and APRIL, the possibility that DC-derived IL-2 plays a role in activating B-cell responses cannot be excluded.
DC and T cells
Activated antigen-loaded DCs migrate to the T-cell zone of secondary lymphoid organs to prime T-cell responses. Naive T-cell priming requires sustained T-cell receptor (TCR) stimulation that is achieved by the formation of an ‘immunological synapse’ (Grakoui et al., 1999), a specialized molecular organization that takes place at the contact region between DCs and T cells. The synapse is a concentric structure with a central supramolecular activation cluster (cSMAC) enriched in TCR, CD2 and CD28, which interact with peptide–MHC complexes, CD58 or CD48 and CD80 or CD86, respectively, surrounded by a peripheral ring (pSMAC) enriched in lymphocyte function associated antigen (LFA-1). The formation of supramolecular aggregates allows the costimulation of and the sustained low-affinity interaction between TCR and specific peptide–MHC complexes. The high efficiency of DCs as APCs has not been attributed to one particular DC-specific, surface or secreted molecule, but to the high level of expression of cell membrane costimulatory proteins, the efficient antigen processing machinery and the secretion of cytokines, properties acquired by DCs during the maturation process (Steinman, 2000). The requirement of DC for T-cell activation has been demonstrated in vivo for CD8+ T lymphocytes. Indeed, mice temporarily deprived of CD11c+ DC are impaired in the ability to mount specific CD8+ T-cell responses to infection with the intracellular bacterium Listeria monocytogenes and the parasite Plasmodium yoelii or following antigen immunization (Jung et al., 2002). Moreover, the relevance of DC maturation for CD8+ T-cell activation has also been assessed in vivo. It has been shown that DCs matured in the presence of LPS or activated through the CD40–CD40L interaction can prime CD8+ T cells independently of the concomitant presence of CD4+ helper T cells (Ridge et al., 1998; Schuurhuis et al., 2000). These two stimuli induce IL-2 production by DCs (Granucci et al., 2003), and so this cytokine could represent an additional relevant molecule conferring on DC the unique CD8+ T-cell priming capacity. In agreement with this assumption, early bacterial activated IL-2-deficient DCs were severely impaired in the ability to induce allogeneic CD8+ and CD4+ T-cell proliferation compared with wild-type DCs (Granucci et al., 2001a). The role of DC-derived IL-2 in T-cell priming is also supported by the fact that immunosuppressive viruses, such as murine cytomegalovirus (MCMV), once established as persistent infections, block IL-2 production by DCs and affect their capacity to activate T cells (Andrews et al., 2001).
DC-derived IL-2 may be also required for induction of T-cell proliferation when the general avidity of the system (frequency of responder antigen-specific T cells, affinity for MHC–peptide complexes and frequency of particular MHC–peptide complexes at the cell surface) is low as can frequently occur in vivo during immune responses to microorganisms.
DCs and regulatory T cells
Regulatory T (T-reg) cells are immune system com ponents involved in maintaining tolerance to self-antigens by inhibiting responses mediated by effector CD4+ and CD8+ T cells (Sakaguchi, 2000). Some T-reg cell populations [those expressing CD4 and IL-2 receptor α chain (CD25)], originate in the thymus, while other T-reg subtypes (those identified as IL-10 producers) differentiate in the periphery (Roncarolo and Levings, 2000). The role of DCs in the peripheral differentiation of T-reg cells has recently been investigated. In particular, it has been observed that repetitive stimulation of naive T cells with allogeneic immature DCs results in the generation of IL-10-producing anergic T cells able to suppress effector T-cell functions (Jonuleit et al., 2000). Similar results were also obtained in vivo in humans; injection of immature DCs pulsed with the influenza peptide induced the differentiation of peptide-specific IL-10-producing T cells and the disappearance of influenza-specific effector CD8+ T cells. In contrast, a single injection of peptide-pulsed mature DCs led to the rapid expansion of specific T lymphocytes (Dhodapkar et al., 2001). Moreover, there are certain types of stimuli, such as TNF-α, that bring DCs to a stage of semi-maturation which seems to be involved in the peripheral differentiation of T-reg cells. Repetitive injections of bone-marrow-derived TNF-α-differentiated DCs prevent experimental autoimmune encephalomyelitis (EAE) by inducing IL-10-producing T-reg cells (Menges et al., 2002). Thus it is likely that T cell encounters with antigen-presenting immature or semi-mature DCs may induce peripheral differentiation of T-reg lymphocytes to maintain peripheral tolerance.
Do DCs play any role in regulating CD4+CD25+ T-reg cell functions? The importance of IL-2 for T-reg cell activity has recently been reported (Furtado et al., 2002). In this experiment, IL-2- or CD25-deficient T cells were transferred in mice that harbor a monoclonal myelin basic protein (MBP)-specific αβ T-cell repertoire and spontaneously develop EAE (Lafaille et al., 1994). Only IL-2-deficient T cells protected from the disease while CD25-negative lymphocytes did not, indicating that IL-2 is not required for the generation of T-reg cells in the thymus but is necessary for T-reg cells in the periphery to exert their functions. Although Th1 lymphocytes are a potential source of IL-2 for T-reg cells, an alternative possibility could be that early activated DCs provide IL-2 to T-reg cells, thus contributing to the maintenance of peripheral tolerance.
Conclusions
DCs exert a fundamental role in regulating adaptive and innate immune responses to microorganisms. The recent finding that DCs can produce IL-2 following microbial encounter opens new possibilities for understanding the efficiency of DC in activating NK, T and B cells to fight infections and, probably, in maintaining peripheral T-cell tolerance via regulation of T-reg cell functions.
Acknowledgments
Acknowledgements
This work was supported by grants from the Italian Association against Cancer (AIRC), 5th EC Programs (DC strategies and TAGAPO) and Ministero dell’Istruzione dell’Università e della Ricerca (MIUR).
References
- Andrews D.M. Andoniou,C.E., Granucci,F., Ricciardi-Castagnoli,P. and Degli-Esposti,M.A. (2001) Infection of dendritic cells by murine cytomegalovirus induces functional paralysis. Nat. Immunol., 2, 1077–1084. [DOI] [PubMed] [Google Scholar]
- Armitage R.J., Macduff,B.M., Eisenman,J., Paxton,R. and Grabstein,K.H. (1995) IL-15 has stimulatory activity for the induction of B cell proliferation and differentiation. J. Immunol., 154, 483–490. [PubMed] [Google Scholar]
- Banchereau J., Briere,F., Caux,C., Davoust,J., Lebecque,S., Liu,Y.J., Pulendran,B. and Palucka,K. (2000) Immunobiology of dendritic cells. Annu. Rev. Immunol., 18, 767–811. [DOI] [PubMed] [Google Scholar]
- Biron C.A., Nguyen,K.B., Pien,G.C., Cousens,L.P. and Salazar-Mather,T.P. (1999) Natural killer cells in antiviral defense: function and regulation by innate cytokines. Annu. Rev. Immunol., 17, 189–220. [DOI] [PubMed] [Google Scholar]
- Borisy G.G. and Svitkina,T.M. (2000) Actin machinery: pushing the envelope. Curr. Opin. Cell Biol., 12, 104–112. [DOI] [PubMed] [Google Scholar]
- Burns S., Thrasher,A.J., Blundell,M.P., Machesky,L. and Jones,G.E. (2001) Configuration of human dendritic cell cytoskeleton by Rho GTPases, the WAS protein and differentiation. Blood, 98, 1142–1149. [DOI] [PubMed] [Google Scholar]
- Cella M., Engering,A., Pinet,V., Pieters,J. and Lanzavecchia,A. (1997) Inflammatory stimuli induce accumulation of MHC class II complexes on dendritic cells. Nature, 388, 782–787. [DOI] [PubMed] [Google Scholar]
- Dhodapkar M.V., Steinman,R.M., Krasovsky,J., Munz,C. and Bhardwaj,N. (2001) Antigen-specific inhibition of effector T cell function in humans after injection of immature dendritic cells. J. Exp. Med., 193, 233–238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ferlazzo G., Tsang,M.L., Moretta,L., Melioli,G., Steinman,R.M. and Munz,C. (2002) Human dendritic cells activate resting natural killer (NK) cells and are recognized via the NKp30 receptor by activated NK cells. J. Exp. Med., 195, 343–351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ferlazzo G., Morandi,B., D’Agostino,A., Meazza,R., Melioli,G., Moretta,A. and Moretta,L. (2003) The interaction between NK cells and dendritic cells in bacterial infections results in rapid induction of NK cell activation and in the lysis of uninfected dendritic cells. Eur. J. Immunol., 33, 306–313. [DOI] [PubMed] [Google Scholar]
- Fernandez N.C. et al. (1999) Dendritic cells directly trigger NK cell functions: cross-talk relevant in innate anti-tumor immune responses in vivo. Nat. Med., 5, 405–411. [DOI] [PubMed] [Google Scholar]
- Furtado G.C., Curotto de Lafaille,M.A., Kutchukhidze,N. and Lafaille,J.J. (2002) Interleukin 2 signaling is required for CD4+ regulatory T cell function. J. Exp. Med., 196, 851–857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Galli S.J., Maurer,M. and Lantz,C.S. (1999) Mast cells as sentinels of innate immunity. Curr. Opin. Immunol. 11, 53–59. [DOI] [PubMed] [Google Scholar]
- Garrett W.S., Chen,L.M., Kroschewski,R., Ebersold,M., Turley,S., Trombetta,S., Galan,J.E. and Mellman,I. (2000) Developmental control of endocytosis in dendritic cells by Cdc42. Cell, 102, 325–334. [DOI] [PubMed] [Google Scholar]
- Gerosa F., Baldani-Guerra,B., Nisii,C., Marchesini,V., Carra,G. and Trinchieri,G. (2002) Reciprocal activating interaction between natural killer cells and dendritic cells. J. Exp. Med., 195, 327–333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grakoui A., Bromley,S.K., Sumen,C., Davis,M.M., Shaw,A.S., Allen,P.M. and Dustin,M.L. (1999) The immunological synapse: a molecular machine controlling T cell activation. Science, 28, 221–227. [DOI] [PubMed] [Google Scholar]
- Granucci F., Vizzardelli,C., Pavelka,N., Feau,S., Persico,M., Virzi,E., Rescigno,M., Moro,G. and Ricciardi-Castagnoli,P. (2001a) Inducible IL-2 production by dendritic cells revealed by global gene expression analysis. Nat. Immunol., 2, 882–888. [DOI] [PubMed] [Google Scholar]
- Granucci F., Vizzardelli,C., Virzi,E., Rescigno,M. and Ricciardi-Castagnoli P. (2001b) Transcriptional reprogramming of dendritic cells by differentiation stimuli. Eur. J. Immunol., 31, 2539–2546. [DOI] [PubMed] [Google Scholar]
- Granucci F., Feau,S., Angeli,V., Trottein,F. and Ricciardi-Castagnoli,P. (2003) Early IL-2 production by mouse dendritic cells is the result of microbial-induced priming. J. Immunol., 170, 5110–5117. [DOI] [PubMed] [Google Scholar]
- Hawiger D., Inaba,K., Dorsett,Y., Guo,M., Mahnke,K., Rivera,M., Ravetch,J.V., Steinman,R.M. and Nussenzweig,M.C. (2001) Dendritic cells induce peripheral T cell unresponsiveness under steady state conditions in vivo. J. Exp. Med., 194, 769–779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Henz B.M., Maurer,M., Lippert,U., Worm,M. and Babina,M. (2001) Mast cells as initiators of immunity and host defense. Exp. Dermatol., 10, 1–10. [DOI] [PubMed] [Google Scholar]
- Huang Q., Liu,D., Majewski,P., Schulte,L.C., Korn,J.M., Young,R.A., Lander,E.S. and Hacohen,N. (2001) The plasticity of dendritic cell responses to pathogens and their components. Science, 294, 870–875. [DOI] [PubMed] [Google Scholar]
- Jonuleit H., Schmitt,E., Schuler,G., Knop,J. and Enk,A.H. (2000) Induction of interleukin 10-producing, nonproliferating CD4+ T cells with regulatory properties by repetitive stimulation with allogeneic immature human dendritic cells. J. Exp. Med., 192, 1213–1222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jonuleit H., Schmitt,E., Steinbrink,K. and Enk,A.H. (2001) Dendritic cells as a tool to induce anergic and regulatory T cells. Trends Immunol., 22, 394–400. [DOI] [PubMed] [Google Scholar]
- Jung S. et al. (2002) In vivo depletion of CD11c+ dendritic cells abrogates priming of CD8+ T cells by exogenous cell-associated antigens. Immunity, 17, 211–220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lafaille J.J., Nagashima,K., Katsuki,M. and Tonegawa,S. (1994) High incidence of spontaneous autoimmune encephalomyelitis in immunodeficient anti-myelin basic protein T cell receptor transgenic mice. Cell, 78, 399–408. [DOI] [PubMed] [Google Scholar]
- Langenkamp A., Messi,M., Lanzavecchia,A. and Sallusto,F. (2000) Kinetics of dendritic cell activation: impact on priming of TH1, TH2 and nonpolarized T cells. Nat. Immunol., 1, 311–316. [DOI] [PubMed] [Google Scholar]
- Lebecque S. (2001) A new job for dendritic cells. Nat. Immunol., 2, 830–831. [DOI] [PubMed] [Google Scholar]
- Litinskiy M.B., Nardelli,B., Hilbert,D.M., He,B., Schaffer,A., Casali,P. and Cerutti,A. (2002) DCs induce CD40-independent immunoglobulin class switching through BLyS and APRIL. Nat. Immunol., 3, 822–829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Medzhitov R. (2001) Toll-like receptors and innate immunity. Nat. Rev. Immunol., 1, 135–145. [DOI] [PubMed] [Google Scholar]
- Menges M., Rossner,S., Voigtlander,C., Schindler,H., Kukutsch,N.A., Bogdan,C., Erb,K., Schuler,G. and Lutz,M.B. (2002) Repetitive injections of dendritic cells matured with tumor necrosis factor alpha induce antigen-specific protection of mice from autoimmunity. J. Exp. Med., 195, 15–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moretta A. (2002) Natural killer cells and dendritic cells: rendezvous in abused tissues. Nat. Rev. Immunol., 2, 957–965. [DOI] [PubMed] [Google Scholar]
- Piccioli D., Sbrana,S., Melandri,E. and Valiante,N.M. (2002) Contact-dependent stimulation and inhibition of dendritic cells by natural killer cells. J. Exp. Med., 195, 335–341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pierre P., Turley,S.J., Gatti,E., Hull,M., Meltzer,J., Mirza,A., Inaba,K., Steinman,R.M. and Mellman,I. (1997) Developmental regulation of MHC class II transport in mouse dendritic cells. Nature, 388, 787–792. [DOI] [PubMed] [Google Scholar]
- Rescigno M., Citterio,S., Thery,C., Rittig,M., Medaglini,D., Pozzi,G., Amigorena,S. and Ricciardi-Castagnoli,P. (1998) Bacteria-induced neo-biosynthesis, stabilization and surface expression of functional class I molecules in mouse dendritic cells. Proc. Natl Acad. Sci. USA, 95, 5229–5234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ridge J.P., Di Rosa,F. and Matzinger,P. (1998) A conditioned dendritic cell can be a temporal bridge between a CD4+ T-helper and a T-killer cell. Nature, 393, 474–478. [DOI] [PubMed] [Google Scholar]
- Roncarolo M.G., and Levings,M.K. (2000) The role of different subsets of T regulatory cells in controlling autoimmunity. Curr. Opin. Immunol., 12, 676–683. [DOI] [PubMed] [Google Scholar]
- Sakaguchi S. (2000) Regulatory T cells: key controllers of immunologic self-tolerance. Cell, 101, 455–458. [DOI] [PubMed] [Google Scholar]
- Sallusto F. and Lanzavecchia,A. (1994) Efficient presentation of soluble antigen by cultured human dendritic cells is maintained by granulocyte/macrophage colony-stimulating factor plus interleukin 4 and downregulated by tumor necrosis factor alpha. J. Exp. Med., 179, 1109–1118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schimpl A., Berberich,I., Kneitz,B., Kramer,S., Santner-Nanan,B., Wagner,S., Wolf,M. and Hunig,T. (2002) IL-2 and autoimmune disease. Cytokine Growth Factor Rev., 13, 369–378. [DOI] [PubMed] [Google Scholar]
- Schuurhuis D.H. et al. (2000) Immature dendritic cells acquire CD8+ cytotoxic T lymphocyte priming capacity upon activation by T helper cell-independent or -dependent stimuli. J. Exp. Med., 192, 145–150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sotomayor E.M., Borrello,I.M., Rattis,F., Cuenca,A.G., Abrams,J., Staveley-O’Carroll,K. and Levitsky,H.I. (2001) Cross-presentation of tumor antigens by bone marrow-derived antigen-presenting cells is the dominant mechanism in the induction of T-cell tolerance during B-cell lymphoma progression. Blood, 98, 1070–1077. [DOI] [PubMed] [Google Scholar]
- Steinman R.M. (2000) DC-SIGN: a guide to some mysteries of dendritic cells. Cell, 100, 491–494. [DOI] [PubMed] [Google Scholar]
- Steinman R.M. and Nussenzweig,M.C. (2002) Avoiding horror autotoxicus: the importance of dendritic cells in peripheral T cell tolerance. Proc. Natl Acad. Sci. USA, 99, 351–358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- VanParijs L., Refaeli,Y., Lord,J.D., Nelson,B.H., Abbas,A.K. and Baltimore,D. (1999) Uncoupling IL-2 signals that regulate T cell proliferation, survival and Fas-mediated activation-induced cell death. Immunity, 11, 281–288. [DOI] [PubMed] [Google Scholar]
- Wedemeyer J., Tsai,M. and Galli.S,J. (2000) Roles of mast cells and basophils in innate and acquired immunity. Curr. Opin. Immunol., 12, 624–631. [DOI] [PubMed] [Google Scholar]
- Winzler C., Rovere,P., Rescigno,M., Granucci,F., Penna,G., Adorini,L., Zimmermann,V.S., Davoust,J. and Ricciardi-Castagnoli,P. (1997) Maturation stages of mouse dendritic cells in growth factor-dependent long-term cultures. J. Exp. Med., 185, 317–328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wykes M., Pombo,A., Jenkins,C. and MacPherson,G.G. (1998) Dendritic cells interact directly with naive B lymphocytes to transfer antigen and initiate class switching in a primary T-dependent response. J. Immunol., 161, 1313–1319. [PubMed] [Google Scholar]