Abstract
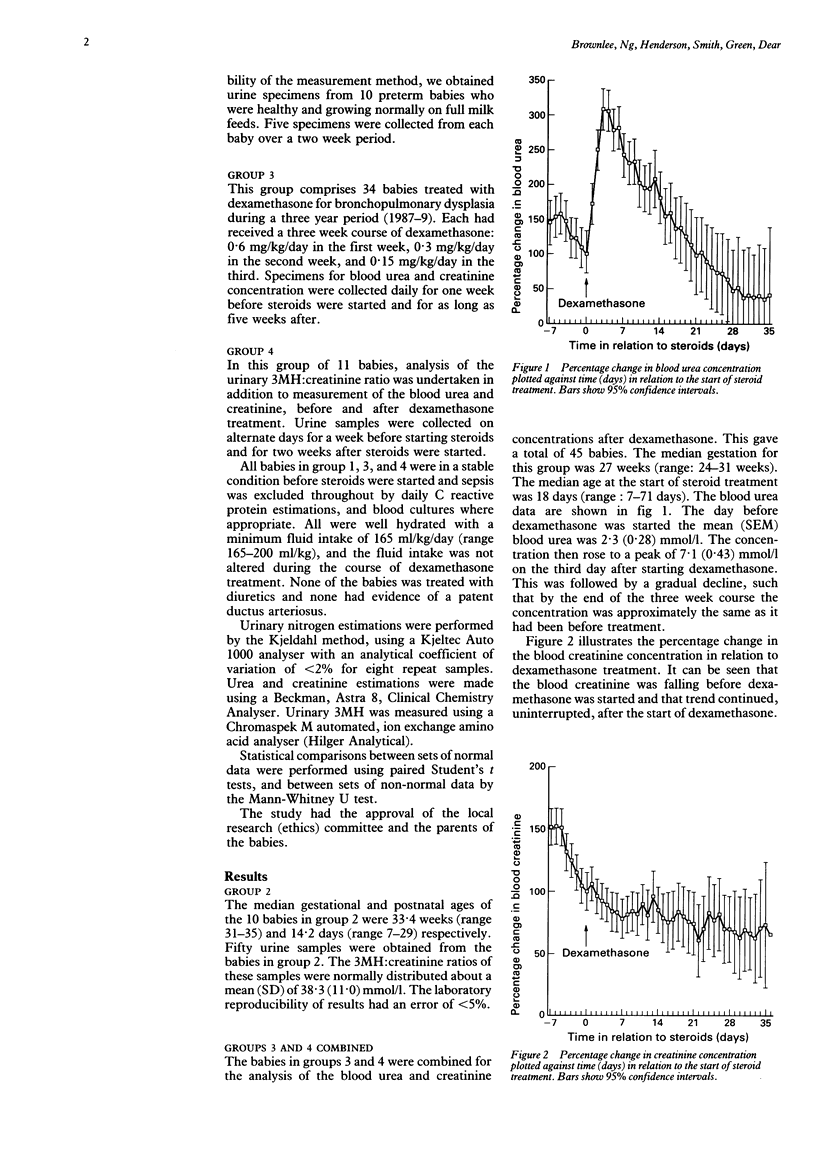
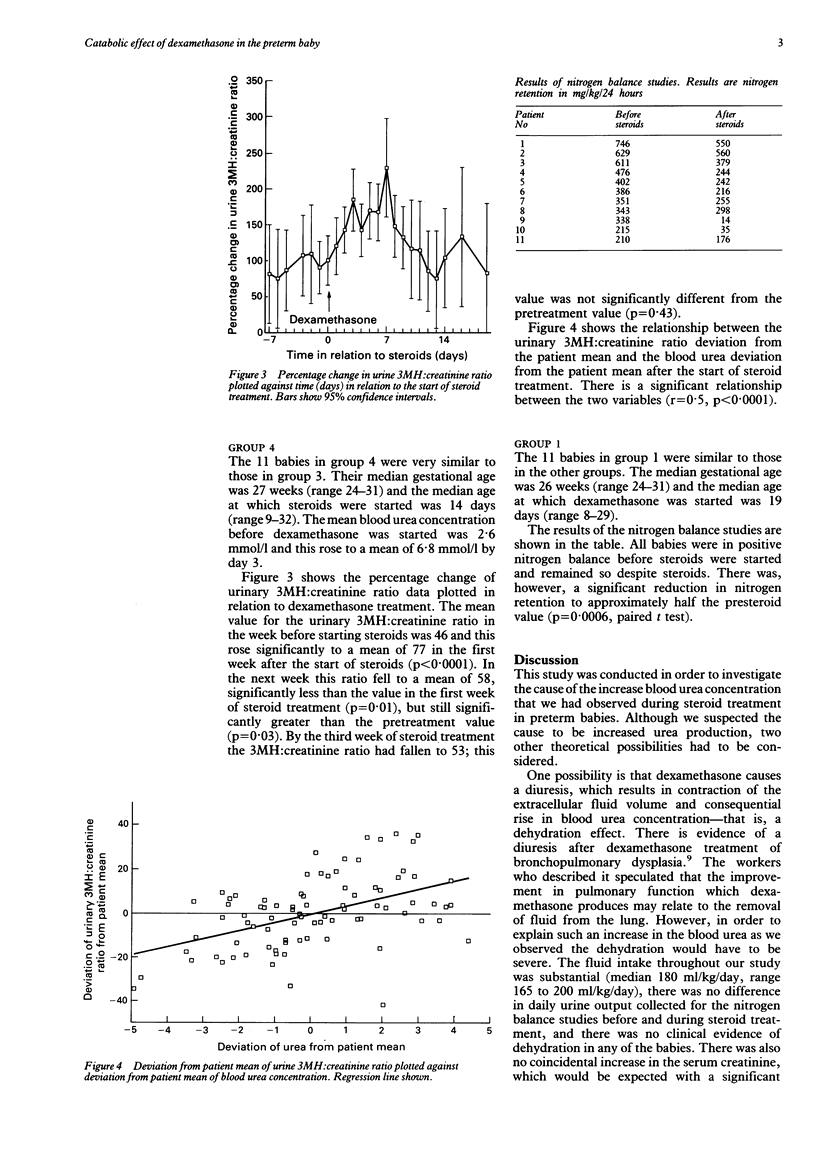
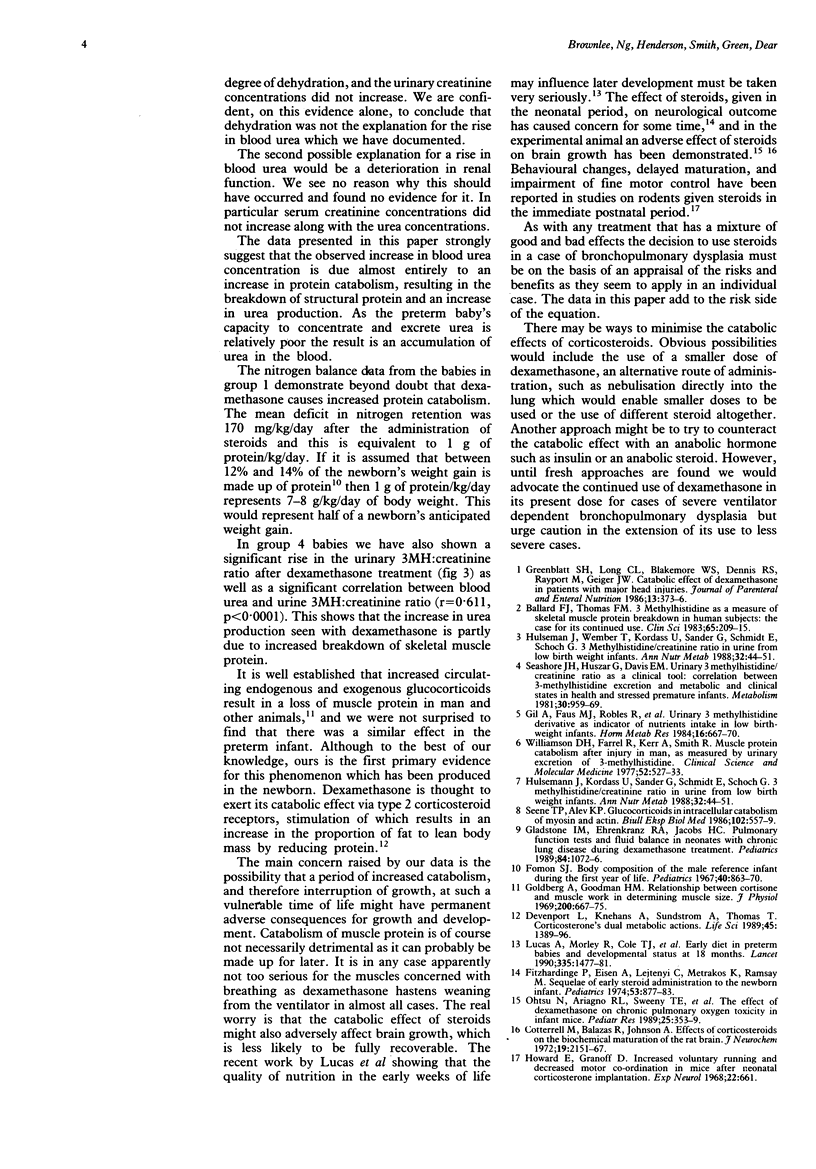
Most babies treated with dexamethasone for bronchopulmonary dysplasia exhibit an appreciable rise in the blood urea concentration, from a mean of 2.3 mmol/l before steroid to a mean of 7.1 mmol/l after. In order to discover whether this was primarily the result of increased protein catabolism, nitrogen balance studies before and after the start of dexamethasone were performed and a mean deficit in nitrogen retention of 158 mg/kg/24 hours was found. Similarly the urinary 3-methylhistidine (3MH):creatinine ratio before and after the commencement of dexamethasone treatment in a group of preterm babies was measured. It was found that there was a substantial increase in 3MH excretion after dexamethasone: from a mean 3MH:creatinine ratio of 46 in the week before steroids to a mean ratio of 77 in the week after. As 3MH emanates almost exclusively from the breakdown of actin in skeletal muscle cell, this finding implies the loss of muscle tissue. It was also found that the babies were in less positive nitrogen balance after dexamethasone, to a degree which is significant relative to their protein reserves. The long term consequences of a period of increased catabolism are not yet known but the authors suggest caution in the use of dexamethasone, at least in babies with milder degrees of bronchopulmonary dysplasia in whom the ratio of benefit to risk may be less favourable.
Full text
PDF
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Ballard F. J., Tomas F. M. 3-Methylhistidine as a measure of skeletal muscle protein breakdown in human subjects: the case for its continued use. Clin Sci (Lond) 1983 Sep;65(3):209–215. doi: 10.1042/cs0650209. [DOI] [PubMed] [Google Scholar]
- Devenport L., Knehans A., Sundstrom A., Thomas T. Corticosterone's dual metabolic actions. Life Sci. 1989;45(15):1389–1396. doi: 10.1016/0024-3205(89)90026-x. [DOI] [PubMed] [Google Scholar]
- Fitzhardinge P. M., Eisen A., Lejtenyi C., Metrakos K., Ramsay M. Sequelae of early steroid administration to the newborn infant. Pediatrics. 1974 Jun;53(6):877–883. [PubMed] [Google Scholar]
- Fomon S. J. Body composition of the male reference infant during the first year of life. Pediatrics. 1967 Nov;40(5):863–870. [PubMed] [Google Scholar]
- Gil A., Faus M. J., Robles R., Pita M. L., Sánchez-Pozo A., Linares M. D., Sánchez-Medina F. Urinary 3-methylhistidine derivative as indicator of nutrients intake in low-birth-weight infants. Horm Metab Res. 1984 Dec;16(12):667–670. doi: 10.1055/s-2007-1014878. [DOI] [PubMed] [Google Scholar]
- Gladstone I. M., Ehrenkranz R. A., Jacobs H. C. Pulmonary function tests and fluid balance in neonates with chronic lung disease during dexamethasone treatment. Pediatrics. 1989 Dec;84(6):1072–1076. [PubMed] [Google Scholar]
- Goldberg A. L., Goodman H. M. Relationship between cortisone and muscle work in determining muscle size. J Physiol. 1969 Feb;200(3):667–675. doi: 10.1113/jphysiol.1969.sp008715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greenblatt S. H., Long C. L., Blakemore W. S., Dennis R. S., Rayport M., Geiger J. W. Catabolic effect of dexamethasone in patients with major head injuries. JPEN J Parenter Enteral Nutr. 1989 Jul-Aug;13(4):373–376. doi: 10.1177/0148607189013004373. [DOI] [PubMed] [Google Scholar]
- Howard E., Granoff D. M. Increased voluntary running and decreased motor coordination in mice after neonatal corticosterone implantation. Exp Neurol. 1968 Dec;22(4):661–673. doi: 10.1016/0014-4886(68)90155-6. [DOI] [PubMed] [Google Scholar]
- Hülsemann J., Kordass U., Sander G., Schmidt E., Schöch G. 3-Methylhistidine/creatinine ratio in urine from low-birth-weight infants. Clinical approach. Ann Nutr Metab. 1988;32(1):44–51. doi: 10.1159/000177391. [DOI] [PubMed] [Google Scholar]
- Hülsemann J., Kordass U., Sander G., Schmidt E., Schöch G. 3-Methylhistidine/creatinine ratio in urine from low-birth-weight infants. Clinical approach. Ann Nutr Metab. 1988;32(1):44–51. doi: 10.1159/000177391. [DOI] [PubMed] [Google Scholar]
- Lucas A., Morley R., Cole T. J., Gore S. M., Lucas P. J., Crowle P., Pearse R., Boon A. J., Powell R. Early diet in preterm babies and developmental status at 18 months. Lancet. 1990 Jun 23;335(8704):1477–1481. doi: 10.1016/0140-6736(90)93026-l. [DOI] [PubMed] [Google Scholar]
- Ohtsu N., Ariagno R. L., Sweeney T. E., Davis L., Moses L., Petriceks R., Daehne I., Bensch K., Northway W. H., Jr The effect of dexamethasone on chronic pulmonary oxygen toxicity in infant mice. Pediatr Res. 1989 Apr;25(4):353–359. doi: 10.1203/00006450-198904000-00008. [DOI] [PubMed] [Google Scholar]
- Seashore J. H., Huszar G., Davis E. M. Urinary 3-methylhistidine/creatinine ratio as a clinical tool: correlation between 3-methylhistidine excretion and metabolic and clinical states in healthy and stressed premature infants. Metabolism. 1981 Oct;30(10):959–969. doi: 10.1016/0026-0495(81)90093-7. [DOI] [PubMed] [Google Scholar]
- Séne T. P., Alev K. P. Gliukortikoidy vo vnutrikletochnom katabolizme miozina i aktina. Biull Eksp Biol Med. 1986 Nov;102(11):557–559. [PubMed] [Google Scholar]
- Williamson D. H., Farrell R., Kerr A., Smith R. Muscle-protein catabolism after injury in man, as measured by urinary excretion of 3-methylhistidine. Clin Sci Mol Med. 1977 May;52(5):527–533. doi: 10.1042/cs0520527. [DOI] [PubMed] [Google Scholar]


