Abstract
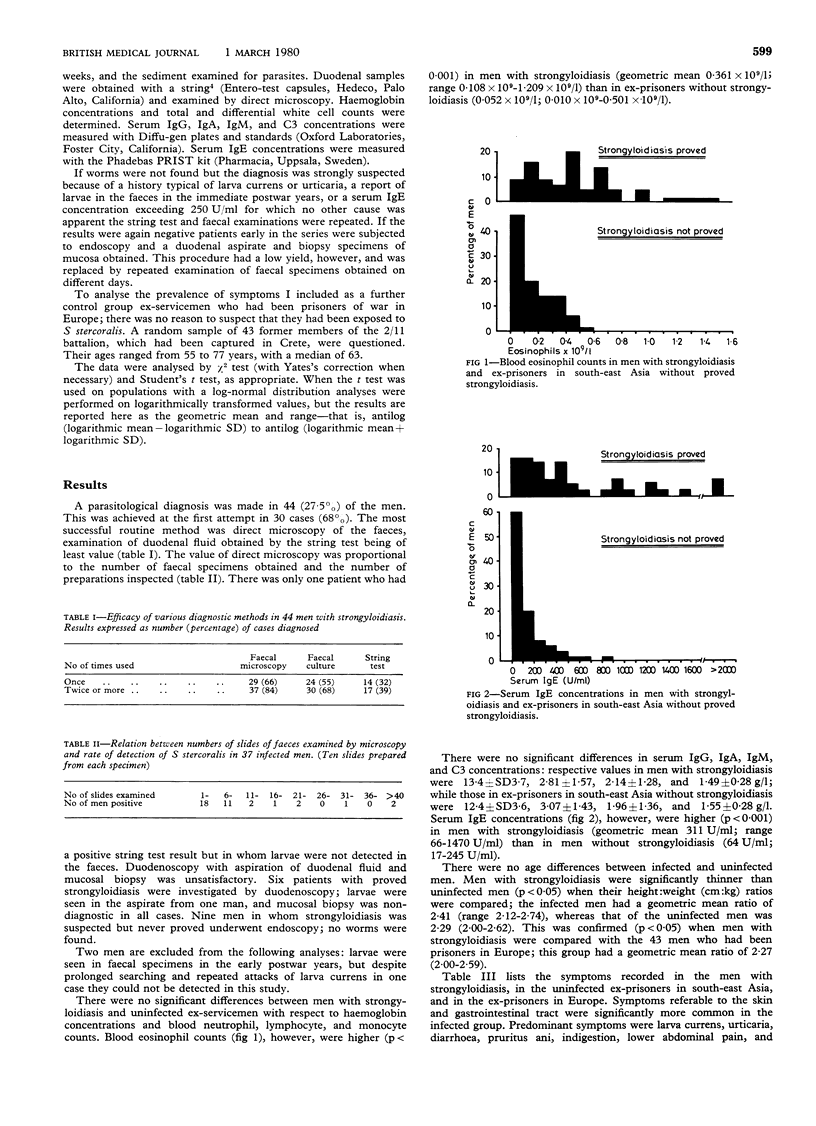
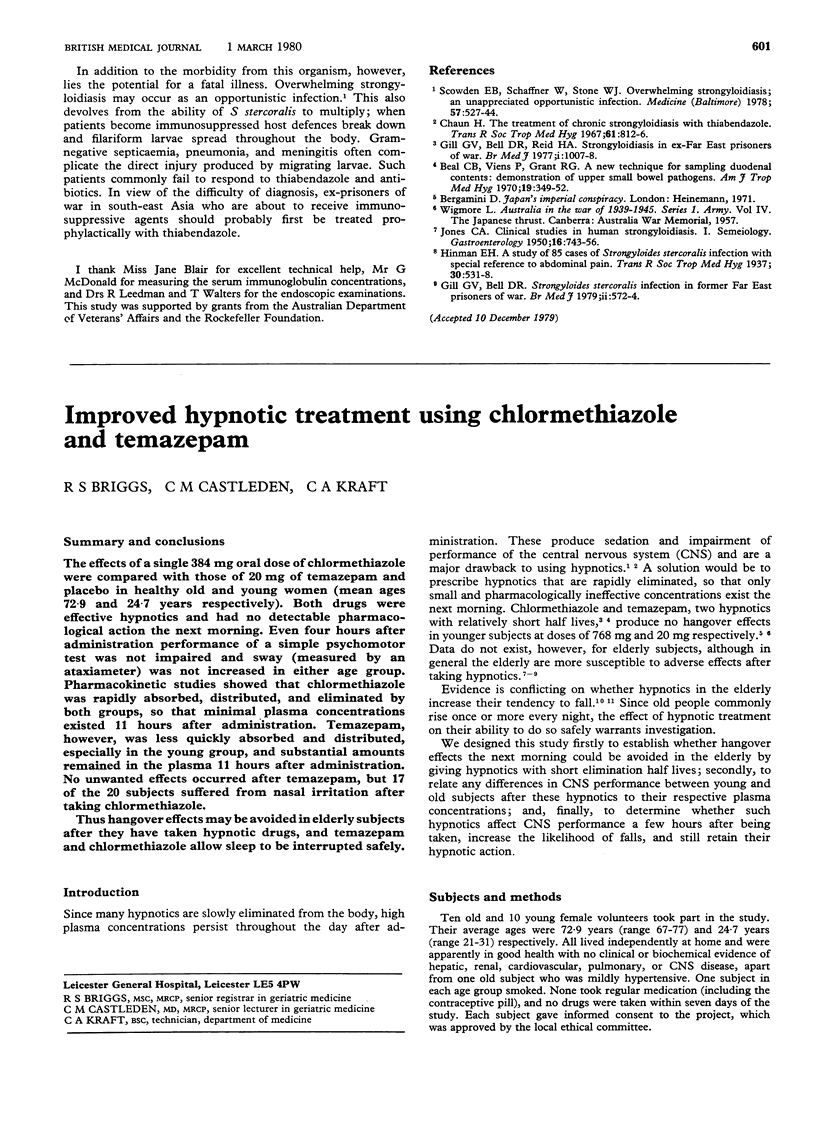
One hundred and sixty ex-servicemen who had been prisoners of war in south-east Asia during 1942-5 were investigated for infection with Strongyloides stercoralis. Larvae were found in 44 (27·5%) of the men, who had therefore been infected for 34-37 years. Direct microscopy of the faeces was the most successful diagnostic method, giving a positive result in 37 cases (84%); multiple examinations were often necessary. Faecal culture was positive in 30 cases (68%), but examination of duodenal fluid obtained with the string test gave a positive result in only 17 (39%). The mean blood eosinophil count and mean serum IgE concentration were higher in the infected men, though normal values were often found in individual cases. Clinical manifestations of isolated strongyloides infection were analysed by comparing the infected men with control groups of ex-prisoners in south-east Asia without proved strongyloidiasis and ex-prisoners in Europe. Twenty-nine infected men (66%) complained of non-specific urticaria, and 13 (30%) had pathognomonic larva currens. Gastrointestinal symptoms significantly more common in the infected group were diarrhoea, indigestion, lower abdominal pain, pruritus ani, and weight loss (p <0·05-p <0·0005).
The study group was thought to be reasonably representative of Allied ex-servicemen imprisoned in south-east Asia during the second world war. Probably there are many thousands of infected persons in several countries. The worm has an unusual ability to multiply, and larvae may spread throughout the body in immunosuppressed subjects.
Full text
PDF

Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Beal C. B., Viens P., Grant R. G., Hughes J. M. A new technique for sampling duodenal contents: demonstration of upper small-bowel pathogens. Am J Trop Med Hyg. 1970 Mar;19(2):349–352. doi: 10.4269/ajtmh.1970.19.349. [DOI] [PubMed] [Google Scholar]
- Chaun H. The treatment of chronic strongyloidiasis with thiabendazole. Trans R Soc Trop Med Hyg. 1967;61(6):812–816. doi: 10.1016/0035-9203(67)90040-5. [DOI] [PubMed] [Google Scholar]
- Gill G. V., Bell D. R., Reid H. A. Strongyloidiasis in ex-Far East prisoners of war. Br Med J. 1977 Apr 16;1(6067):1007–1007. doi: 10.1136/bmj.1.6067.1007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gill G. V., Bell D. R. Strongyloides stercoralis infection in former Far East prisoners of war. Br Med J. 1979 Sep 8;2(6190):572–574. doi: 10.1136/bmj.2.6190.572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- JONES C. A. Clinical studies in human strongyloidiasis. I Semeiology. Gastroenterology. 1950 Dec;16(4):743–756. [PubMed] [Google Scholar]
- Scowden E. B., Schaffner W., Stone W. J. Overwhelming strongyloidiasis: an unappreciated opportunistic infection. Medicine (Baltimore) 1978 Nov;57(6):527–544. [PubMed] [Google Scholar]


