Abstract
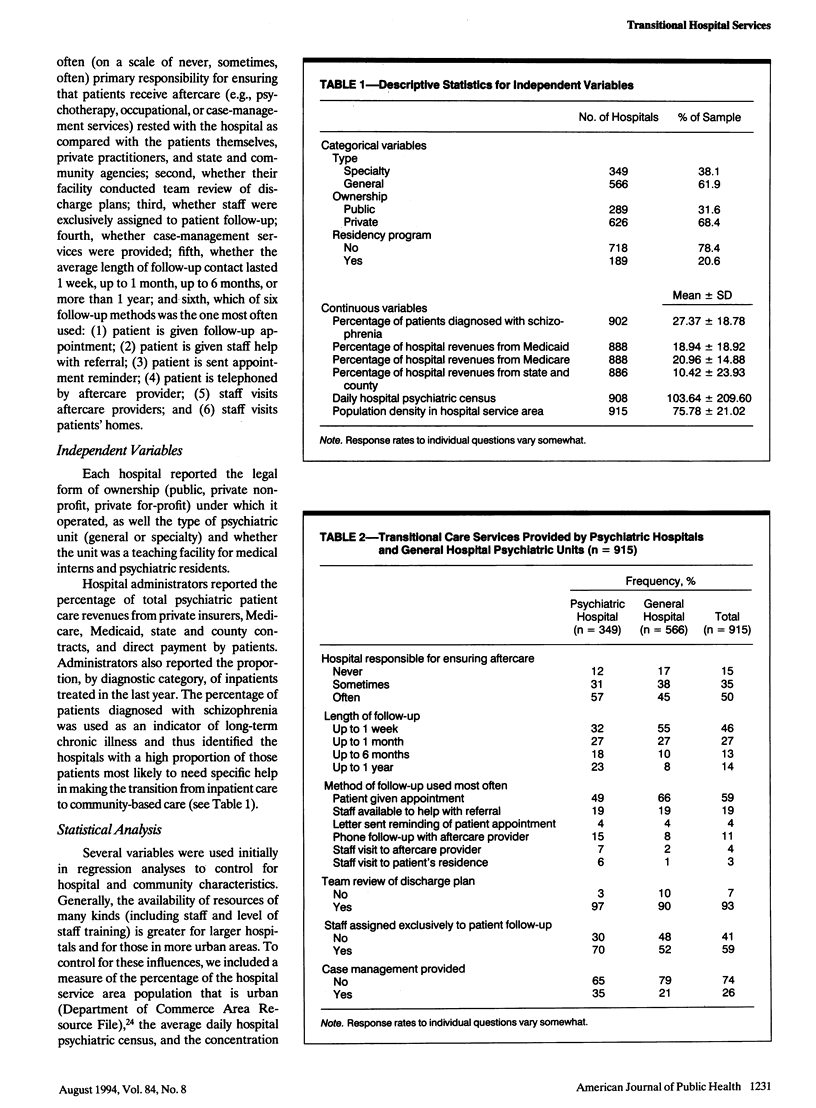
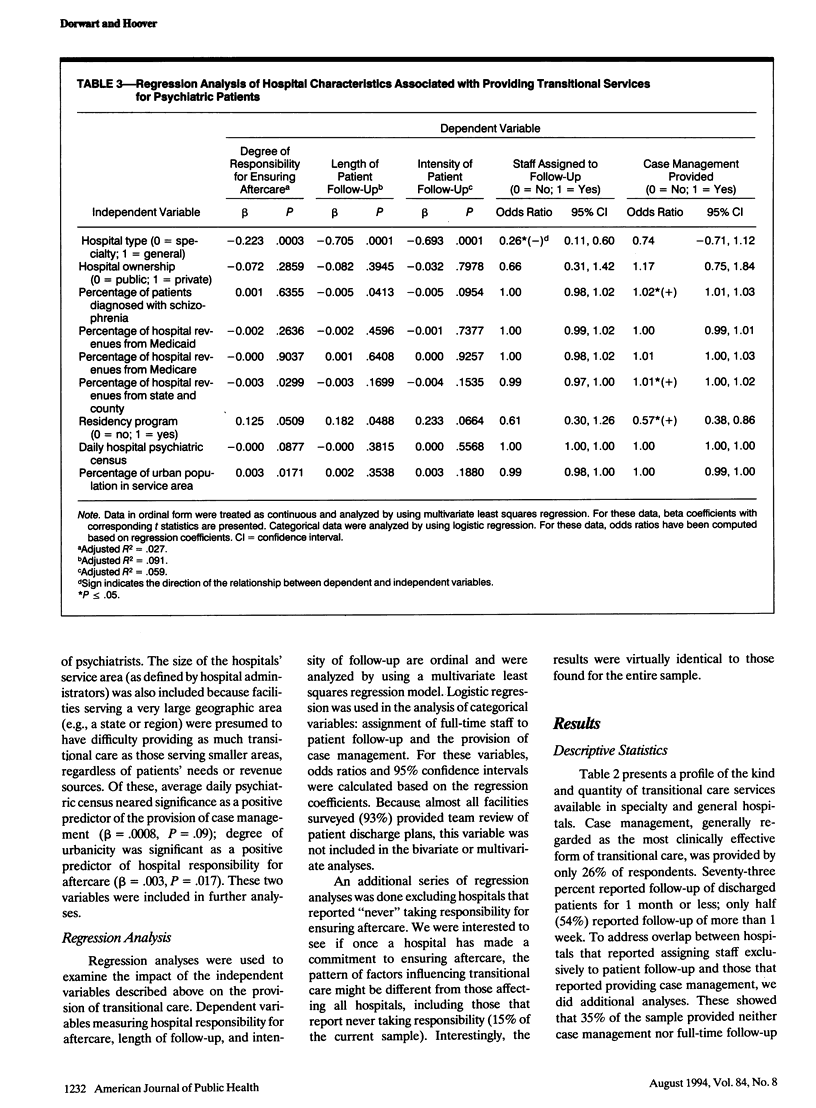
OBJECTIVES. Shifts in care for the seriously mentally ill from inpatient to community-based treatment have highlighted the importance of transitional care. Our objectives were to document the kinds and quantity of transitional services provided by psychiatric hospitals nationally and to assess the impact of hospital type (psychiatric vs general), ownership (public vs private), case mix, and revenue source on provision of these services. METHODS. A national sample of nonfederal inpatient mental health facilities (n = 915) was surveyed in 1988, and data were analyzed by using multiple regression. RESULTS. Half (46%) of the facilities surveyed provided patient follow-up of 1 week or less, and almost all (93%) conducted team review of discharge plans, but 74% provided no case management services. Hospital type was the most consistent predictor of transitional care, with psychiatric hospitals providing more of these services than general hospitals. Severity of illness, level of nonfederal funding, urbanicity, and teaching hospital affiliation were positively associated with provision of case management. CONCLUSIONS. Transitional care services for mentally ill patients leaving the hospital were found to be uneven and often inadequate. Reasons for broad variation in services are discussed.
Full text
PDF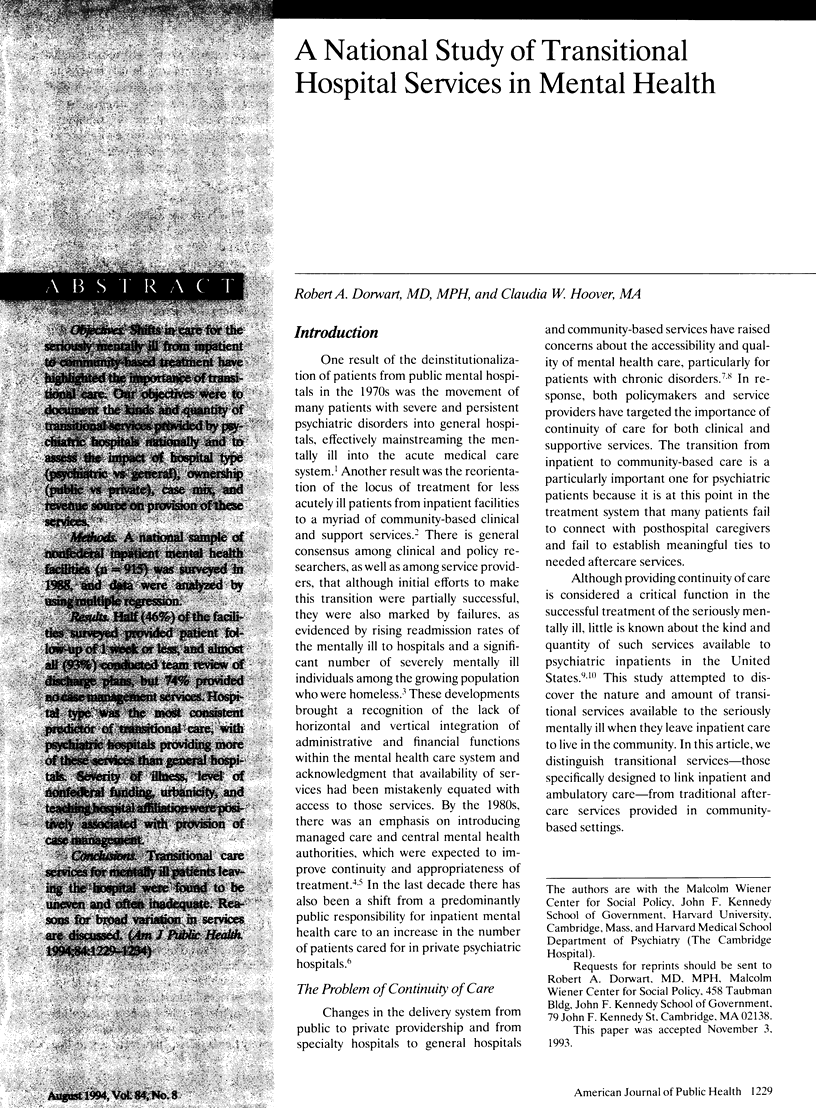


Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Bachrach L. L. Continuity of care and approaches to case management for long-term mentally ill patients. Hosp Community Psychiatry. 1993 May;44(5):465–468. doi: 10.1176/ps.44.5.465. [DOI] [PubMed] [Google Scholar]
- Bachrach L. L. The challenge of service planning for chronic mental patients. Community Ment Health J. 1986 Fall;22(3):170–174. doi: 10.1007/BF00756979. [DOI] [PubMed] [Google Scholar]
- Clark R. E., Fox T. S. A framework for evaluating the economic impact of case management. Hosp Community Psychiatry. 1993 May;44(5):469–473. doi: 10.1176/ps.44.5.469. [DOI] [PubMed] [Google Scholar]
- Dorwart R. A. Managed mental health care: myths and realities in the 1990s. Hosp Community Psychiatry. 1990 Oct;41(10):1087–1091. doi: 10.1176/ps.41.10.1087. [DOI] [PubMed] [Google Scholar]
- Dorwart R. A., Schlesinger M., Davidson H., Epstein S., Hoover C. A national study of psychiatric hospital care. Am J Psychiatry. 1991 Feb;148(2):204–210. doi: 10.1176/ajp.148.2.204. [DOI] [PubMed] [Google Scholar]
- Dorwart R. A., Schlesinger M. Privatization of psychiatric services. Am J Psychiatry. 1988 May;145(5):543–553. doi: 10.1176/ajp.145.5.543. [DOI] [PubMed] [Google Scholar]
- Fisher W. H., Dorwart R. A., Schlesinger M., Davidson H. Contracting between public agencies and private psychiatric inpatient facilities. Med Care. 1991 Aug;29(8):766–774. doi: 10.1097/00005650-199108000-00009. [DOI] [PubMed] [Google Scholar]
- Fisher W. H., Geller J. L., Altaffer F., Bennett M. B. The relationship between community resources and state hospital recidivism. Am J Psychiatry. 1992 Mar;149(3):385–390. doi: 10.1176/ajp.149.3.385. [DOI] [PubMed] [Google Scholar]
- Herman N. J., Smith C. M. Mental hospital depopulation in Canada: patient perspectives. Can J Psychiatry. 1989 Jun;34(5):386–391. doi: 10.1177/070674378903400505. [DOI] [PubMed] [Google Scholar]
- Mechanic D. Managed care for the seriously mentally ill. Am J Public Health. 1992 Jun;82(6):788–789. doi: 10.2105/ajph.82.6.788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meyerson A. T., Herman G. S. What's new in aftercare? A review of recent literature. Hosp Community Psychiatry. 1983 Apr;34(4):333–342. doi: 10.1176/ps.34.4.333. [DOI] [PubMed] [Google Scholar]
- Rosenfield S., Caton C., Nachumi G., Robbins E. Closing the gaps: the effectiveness of linking programs connecting chronic mental patients from the hospital to the community. J Appl Behav Sci. 1986;22(4):411–423. doi: 10.1177/002188638602200405. [DOI] [PubMed] [Google Scholar]
- Shore M. F., Cohen M. D. The Robert Wood Johnson Foundation Program on Chronic Mental Illness: an overview. Hosp Community Psychiatry. 1990 Nov;41(11):1212–1216. doi: 10.1176/ps.41.11.1212. [DOI] [PubMed] [Google Scholar]
- Siegel C., Alexander M. J., Lin S. Severe alcoholism in the mental health sector: II. Effects of service utilization on readmission. J Stud Alcohol. 1984 Nov;45(6):510–516. doi: 10.15288/jsa.1984.45.510. [DOI] [PubMed] [Google Scholar]
- Solomon P., Gordon B., Davis J. M. Reconceptualizing assumptions about community mental health. Hosp Community Psychiatry. 1986 Jul;37(7):708–712. doi: 10.1176/ps.37.7.708. [DOI] [PubMed] [Google Scholar]
- Surles R. C., Blanch A. K., Shern D. L., Donahue S. A. Case management as a strategy for systems change. Health Aff (Millwood) 1992 Spring;11(1):151–163. doi: 10.1377/hlthaff.11.1.151. [DOI] [PubMed] [Google Scholar]
- Torrey E. F. Continuous treatment teams in the care of the chronic mentally ill. Hosp Community Psychiatry. 1986 Dec;37(12):1243–1247. doi: 10.1176/ps.37.12.1243. [DOI] [PubMed] [Google Scholar]


