Abstract
Inflammatory mediators play a crucial role in the pathophysiology of several neurodegenerative diseases including acquired immune deficiency syndrome dementia complex. In the present study we identified a link between CXCL10 overexpression in the brain and human immunodeficiency virus dementia and demonstrated the presence of the chemokine CXCL10 and its receptor, CXCR3, in the neurons in the brains of macaques with simian human immunodeficiency virus encephalitis. Using human fetal brain cultures, we showed that treatment of these cells with either SHIV89.6P or viral gp120 resulted in induction of CXCL10 in neurons. Cultured neurons treated with the chemokine developed increased membrane permeability followed by apoptosis via activation of caspase-3. We confirmed the relevance of these findings in sections of human and macaque brains with encephalopathy demonstrating that neurons expressing CXCL10 also expressed caspase-3.
It is estimated that almost 25% of untreated human immunodeficiency virus (HIV)-infected individuals and ∼7% of HIV-infected patients treated with highly active anti-retroviral therapy develop HIV-associated dementia (HAD),1–4 a neurodegenerative syndrome that is clinically characterized by progressive cognitive, motor, and behavioral abnormalities.5,6 Pathological manifestation of the syndrome, HIV-encephalitis (HIV-E), is accompanied by prominent microglial activation, perivascular accumulations of mononuclear cells, formation of microglial nodules, presence of virus-infected multinucleated giant cells among the accumulations of macrophages, and neuronal damage and loss.7–9 The primary cell types infected by HIV-1 in the brain are macrophages/microglia, and to a lesser extent, astrocytes, but not neurons.10 One broad explanation frequently advocated explaining the loss of neurons in this disease is that cellular and/or viral proteins released from the infected cells have a direct toxic effect on the neurons.11–18
Because all parenchymal brain cells are known to express chemokine receptors,19 and because expression of chemokines becomes dysregulated and frequently overexpressed during central nervous system (CNS) inflammation, it is possible that overexpressed chemokines in the HIV-infected brain may orchestrate the degenerative neuronal changes.20 In earlier studies aimed at exploring factors contributing to encephalitis caused by simian human immunodeficiency virus (SHIV) in the rhesus macaque model of HIV encephalopathy, we performed chemokine microarray analysis on the brains of infected macaques with and without SHIV-E. Among the various dysregulated genes identified on the array, a dramatic up-regulation (∼20-fold) of CXCL10 (formerly known as IP-10, interferon-γ-inducible protein) was observed in the brains of macaques with SHIV-E.21
CXCL10 is a secreted polypeptide of 10 kd that was first identified as an early response gene induced after interferon-γ treatment in a variety of cells, and was thus named interferon-inducible peptide, IP-10.22,23 In addition to interferon-γ, HIV envelope glycoprotein gp120 has also been shown to induce expression of CXCL10 in brains of mice.24 CXCL10 has been detected in the cerebrospinal fluid of individuals with HIV-1 infection25,26 and in the brains of individuals with HAD.27 Kolb and co-workers25 reported that CXCL10 is present in the cerebrospinal fluid of all HIV-1-infected patients but is absent in uninfected control individuals. Significantly, these authors also reported that CXCL10 levels were closely associated with the progression of HIV-1-related CNS infection and neuropyschiatric impairment.25 CXCL10 and its receptor CXCR3, were also shown to be present in SIV/SHIV-encephalitis.21,28,29
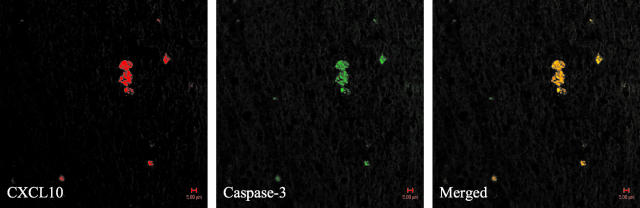
In the present study, we used the SHIV/rhesus macaque model of HIV-E to investigate whether there was a link between CXCL10 overexpression and neuronal degeneration. Using confocal microscopy on immunohistochemically stained sections of macaque brains with SHIV-E, we report localization of CXCL10 in neurons. Moreover, we found that overexpression of CXCL10 co-localized with the active form of caspase-3, the common effector caspase of the apoptosis cascade. Further, using human fetal brain cultures, we show that both SHIV89.6P and viral gp120 induced expression of the chemokine in neurons and that exogenous CXCL10 led to activation of caspase-3 and neuronal apoptosis in these mixed cultures. Relevance of these findings to the human disease was substantiated with the demonstration that CXCL10 was overexpressed in neurons in the brains of individuals with HIV-E. These results suggest a novel role for this chemokine in neuronal dysfunction, with a possible link to HIV dementia.
Materials and Methods
Animals
Five rhesus macaque monkeys previously used to define cytokine/chemokine gene expression profiles in the brain were used in this study. The five animals were infected with SHIV89.6P and all developed acquired immune deficiency syndrome (AIDS)-defining illnesses. All five had also developed virus infection in the brain but only three of these animals developed SHIV-E as demonstrated by histopathology of nine different regions of the brain.21 Details of viral inoculation, disease course, processing of tissue samples, and histological analysis of the tissues have been described earlier.21 Prominent neuropathological changes were present in basal ganglia, motor cortex, and brain stem regions in the encephalitic animals.
Antibodies
R-Phycoerythrin-conjugated/unconjugated mouse anti-human CXCL10 monoclonal antibodies and mouse anti-human CXCR3 antibody were purchased from BD PharMingen (San Diego, CA). Rabbit anti-human active casapase-3 polyclonal antibody and mouse anti-human CXCL10 monoclonal antibody were purchased from R&D Systems (Minneapolis, MN). Mouse anti-neuronal nuclei (NeuN) monoclonal antibody was purchased from Chemicon (Temecula, CA). Rabbit anti-microtubule-associated protein 2 (MAP-2) and neurofilament, two neuronal markers, were purchased from Sigma-Aldrich (St. Louis, MO) and rabbit anti-glial fibrillary acidic protein (GFAP) antibody, an astrocyte marker, was purchased from DAKO (Glostrup, Denmark). Alexa Fluor 488/594 goat anti-rabbit/mouse IgGs (Molecular Probes, Eugene, OR) were used as the secondary antibodies.
Immunohistochemical/Immunocytochemical Analyses
Immunohistochemical analysis was performed on paraffin-fixed sections of brain as previously described.21 Briefly, paraffin sections of brain tissue were dewaxed, rehydrated in graded ethanol solutions, and then irradiated at 750 W in a microwave oven in 0.01 mol/L sodium citrate buffer, pH 6.0, for 1.5 minutes. After blockage with 1% of milk in phosphate-buffered saline, the sections were stained with primary/secondary antibodies. For double-immunofluorescence staining, sections were first treated with the primary antibody, followed by treatment with Alexa Fluor 594/488-conjugated secondary antibody. The sections were then stained with another primary antibody (different species from the first primary antibody), followed by treating with Alexa Fluor 488/594-conjugated secondary antibody. After the final washing, the slides were mounted in SlowFade anti-fade reagent with 4,6-diamidino-2-phenylindole (DAPI) (Molecular Probes, Eugene, OR) and images were captured by confocal microscope.
Western Blotting
For Western blotting, proteins from brain homogenates were separated by sodium dodecyl sulfate-polyacrylamide gel electrophoresis (18% gels) under reducing conditions in the presence of 10 mmol/L dithiothreitol, and electrotransferred to nitrocellulose membranes that were blocked, and incubated with 2 μg/ml of anti-CXCL10 monoclonal antibodies from two different sources. Alkaline phosphatase conjugated to goat-anti-mouse IgG was used as a secondary antibody. CXCL10 signal was detected by chemiluminescence (CDP-star; Tropix, Bedford, MA).
Cell Cultures
Fetal Brain Cultures
Brain specimens were obtained from human fetuses of 12 to 14 weeks gestational age with consent from women undergoing elective termination of pregnancy and approval by the Johns Hopkins University Institutional Review Board. After dissection, tissue was mechanically disrupted by aspiration through a 19-gauge needle, rinsed in Eagle’s minimal essential medium (MEM), and cultured in MEM containing 10% fetal bovine serum, l-glutamine (2 mmol/L), and gentamicin (5 μg/ml) and 1% of N-2 supplement.30 These cultures were comprised mainly of neurons (70%) and astrocytes (30%).30
NT-2 Cell Cultures
Undifferentiated human teratocarcinoma cells NTera 2/c1.D1 (NT−) were maintained in Opti-MEM supplemented with 5% fetal bovine serum and penicillin (100 U/ml) and streptomycin (100 U/ml) (all from Life Technologies, Grand Island, NY) and were differentiated with retinoic acid as described previously.31 Briefly, undifferentiated NT2 cells were treated with 10 μmol/L retinoic acid (Sigma-Aldrich, St. Louis, MO) for a period of 5 to 6 weeks and harvested by selective trypsinization. This neuron-enriched culture was replated three times in medium containing mitotic inhibitors (10 μmol/L 5-fluoro-2′-deoxyuridine, 10 μmol/L uridine, 1 μmol/L cytosine β-d-arabinofuranoside) to prevent the undifferentiated cells from overgrowing the postmitotic neurons. Cell suspensions rich in neurons were then seeded in glass chamber slides and flasks and used in various assays. NT-2 neurons are greater than 95% pure.
Induction of CXCL10 with SHIV89.6P and gp120 of Macrophage-Tropic HIV
Fetal brain cultures were inoculated with SHIV89.6P for 1 to 2 hours, after which, the inoculum was removed in three washes with RPMI 1640. The cultures were then replenished with fresh medium. After 18 hours of incubation, the supernatant was collected for analysis of CXCL10 expression using the CXCL10 enzyme-linked immunosorbent assay (ELISA) kit. Confocal microscopy using antibodies specific for neurofilament and CXCL10 was used to determine whether neurons in the inoculated cultures were the producers of the chemokine. Fetal brain cultures were also treated with varying concentrations (10 to 500 ng/ml) of gp120 derived from macrophage-tropic HIV-Bal for 48 hours and supernatant fluids were collected to determine the levels of CXCL10 protein by ELISA. The ELISA kit was purchased from R&D Systems (Minneapolis, MN). The detection limit was 5 pg/ml.
CXCL10 Assay of Degenerative Changes in Neurons
Cell Viability
The Cell Titer 96 Aqueous One Solution Assay (Promega, Madison, WI) was performed using the manufacturer’s recommendation to measure viability of the neuronal cells.
Changes in Membrane Permeability
Fetal brain cultures were seeded at 40% confluence in six-well plates and after attachment, the cells were incubated with different concentrations of CXCL10 (10 to 100 ng/ml). Individual cultures were harvested at different time points after treatment, and stained with propidium iodide solution (1 mg/ml) for 30 minutes, then analyzed by fluorescence-activated cell sorting. The results were expressed as average intensity of propidium iodide staining as previously described.32
ApoAlert Caspase Profiling Assay
Fetal neuronal cultures were seeded in 96-well plates and cultured in Opti-MEM medium with 100 U/ml penicillin, 100 U/ml streptomycin, and 10% fetal bovine serum (Life Technologies, Inc., Grand Island, NY). After attachment, the cells were incubated with 50 ng/ml of CXCL10 (BD PharMingen, San Diego, CA). Individual cultures were collected, lysed, centrifuged (14,000 rpm, 5 minutes), and the supernatant collected. One hundred μl of the lysates were transferred into each well of the ApoAlert Caspase Profiling Assay plate (BD Biosciences Clontech, Palo Alto, CA) and then incubated at 37°C for 2 hours. A CytoFluor fluorescence plate reader set to 380 nm (excitation) and 460 nm (emission) was used for fluorescence measurements.
Terminal dUTP Nick-End Labeling (TUNEL) ELISA Assay
Cells were also harvested to assess degenerative changes as indicated by the extent of high-molecular weight DNA strand breaks. This was performed by the Cell Death Detection ELISA kit (Boehringer Mannheim, Indianapolis, IN) according to the manufacturer’s instructions. To confirm the activation of caspase by CXCL10, 3 hours before the addition of CXCL10, a pan-caspase inhibitor [50 μmol/L N-benzyloxycarbonyl-Val-Ala-Asp-fluorometry ketone (zVAD-fmk)] or a caspase-3-specific inhibitor [50 μmol/L z-Asp-Glu-Val-Asp-fluoromethy ketone (DEVD-fmk)] was added. Briefly, CXCL10-treated cells were harvested and transferred to the streptavidin-coated microplates, followed by incubation with anti-histone-biotin and anti-DNA-POD complex. During the incubation period, the anti-histone antibody binds to the histone component of the nucleosomes and simultaneously captures the immunocomplex to the streptavidin-coated MP via its biotinylation. Additionally, the anti-DNA-POD antibody reacts with the DNA component of the nucleosomes. After removing the unbound antibodies, we quantified the labeled nucleosomes photometrically.
Human Tissue Samples
Paraffin-embedded brain sections from basal ganglia of two adult patients with HIV encephalitis, two with HIV infection without encephalitis were stained as described. Postmortem intervals varied between 5 and 21 hours. All human tissue samples were obtained from the National Neuro-AIDS tissue consortium (Galveston, TX).
Statistical Analysis
Statistical analysis was performed using one-way analysis of variance. Results were judged statistically significant if p < 0.05 by analysis of variance.
Results
Localization of CXCL10 in Neurons in Brains of Macaques with SHIV-E
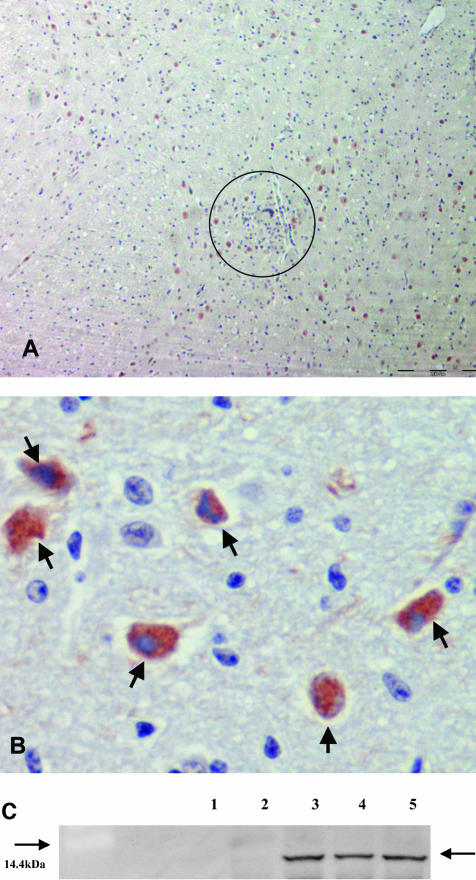
In our previous studies, we had examined brains from five SHIV89.6P-infected macaques that succumbed to AIDS. Three of the five animals had developed CNS lesions and had lentiviral encephalitis associated with opportunistic infections. The two other animals died with AIDS but had no CNS lesions.21,33 Microarray analysis for cytokine and chemokine genes in the brains from the two groups of macaques demonstrated a marked up-regulation of CXCL10 RNA (almost a 20-fold increase) in the brains of macaques with SHIV-E compared to brains of infected macaques without encephalitis.21 In assays described here, we used sections of encephalitic brain for immunohistochemical analyses to determine the expression pattern of CXCL10. As shown in Figure 1A, CXCL10 antigen was observed in large cells outside of and in close proximity to microglial nodules, but not in the macrophages populating the nodules. Microglial nodules in SHIV-E animals were found mainly in the basal ganglia. These lesions were also seen sporadically in different cortical areas of the brain and were located mainly at the junctions of gray and white matter. Close examination of these cells showed that the CXCL10 protein was localized mainly in the cytoplasm of the cells (Figure 1B). These findings were further confirmed by Western blot analysis revealing an up-regulation of CXCL10 protein in the brains of macaques with SHIV-E as compared to brains of SHIV-infected animals without encephalitis that lacked the protein (Figure 1C).
Figure 1.
A and B: Demonstration of CXCL10 antigen in basal ganglia region of SHIV-encephalitic brain by immunohistochemistry. Microglial nodule in A is highlighted within the circle. Arrows in B indicate CXCL10-positive cells. C: Western blot analysis, showing expression of CXCL10 in brains of macaques with (lanes 3 to 5) and without (lanes 1 and 2) encephalitis. Arrow on the right indicates the CXCL10 protein. Number on the left indicates the 14.4-kd protein in the marker. Original magnifications: ×100 (A); ×200 (B).
Consistent with our previous reverse transcriptase-polymerase chain reaction analysis,21 CXCL10 staining was absent in the brain sections of macaques without encephalitis. Constitutive expression of CXCR3, the receptor for CXCL10 in the neurons was observed in the brains of macaques with SHIV-E (data not shown), confirming similar findings in human brains.30,34
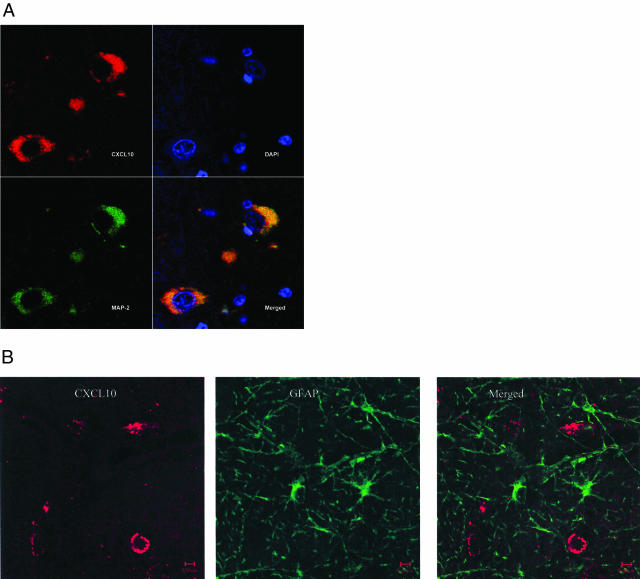
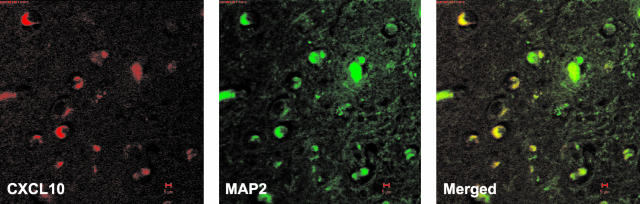
To determine whether CXCL10-expressing cells in the encephalitic brains were neurons or astrocytes, we performed double-label confocal microscopy using antibodies specific for CXCL10 and cell-specific markers [neuronal marker, MAP-2 (microtubule-associated protein) or astrocyte-specific marker, GFAP]. These studies showed that the cells in which CXCL10 was identified were the cells that also stained with MAP-2 antibodies (Figure 2A). In contrast, none of the CXCL10-stained cells were positive for GFAP (Figure 2B). These studies suggested that neurons (almost 35%) were the main cells expressing CXCL10 in SHIV-E.
Figure 2.
Cellular localization of CXCL10 in the brains of SHIV89.6P-infected macaque with encephalitis. A: Basal ganglia regions of the brain from SHIV-E macaques were double immunostained with anti-MAP-2 (green) and anti-CXCL10 (red) antibodies. DAPI (blue) was also applied to stain the nuclei (top right). Confocal microscopy analysis showed that CXCL10 co-localized with MAP-2 in the SHIV-E brain sections (bottom right). B: Basal ganglia regions of the SHIV-E macaques were double immunostained with anti-GFAP (green) antibody and anti-CXCL10 (red). Confocal microscopy analysis showed lack of CXCL10 and GFAP co-localization (merged image).
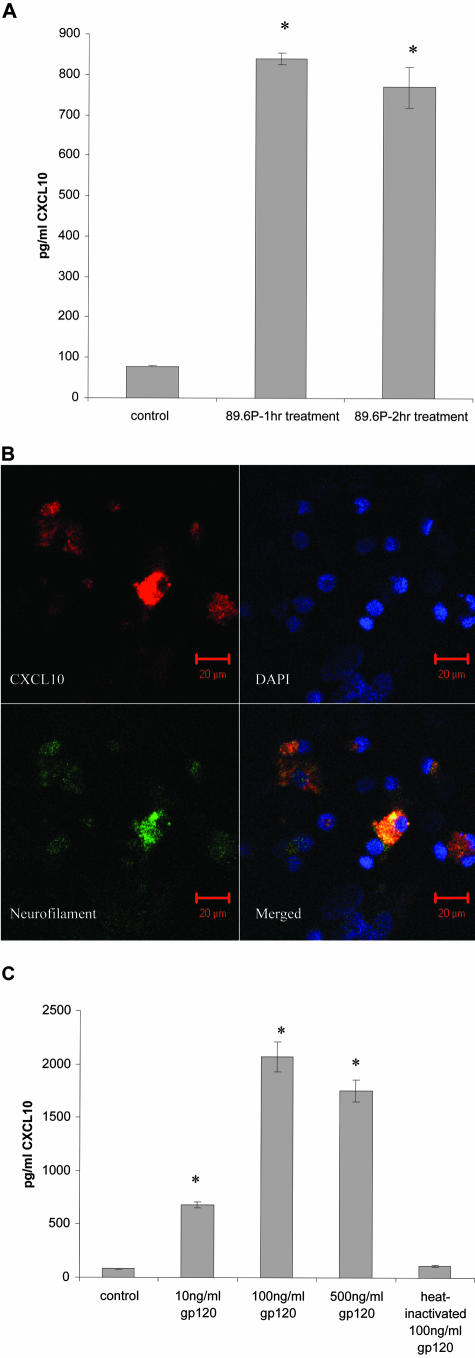
Induction of CXCL10 by SHIV89.6P and Viral gp120 in Fetal Brain Cultures
To explain the uniquely high concentration of CXCL10 in neurons in SHIV-E, we inquired whether treatment of fetal neuronal cultures with SHIV 89.6P could induce expression of the chemokine in neurons. We demonstrated the up-regulation in expression of CXCL10 on SHIV89.6P treatment in fetal neuronal cultures (Figure 3A). To explore whether neurons in the fetal brain cultures inoculated with stock SHIV89.6P produced CXCL10, we performed confocal microscopy using antibodies specific for neurofilament and CXCL10. This experiment showed that greater than 30% of the neurons in the culture expressed CXCL10 (Figure 3B).
Figure 3.
Fetal neuronal cultures were exposed to SHIV89.6P (A) or varying concentrations of macrophage-tropic gp120BAL (C) and expression of CXCL10 in the culture supernatants was quantitatively determined by ELISA. *, Statistical significance compared to control. B: SHIV89.6P induced CXCL10 expression in neurons in fetal brain cultures. Fetal neuronal cultures treated with the virus stock were immunostained with anti-CXCL10 (red) and anti-neurofilament (green) antibodies. DAPI (blue stain) was also applied to stain the nuclei. CXCL10 was localized in neurons.
Because neurons are uninfectable by the virus, we inquired whether the viral gp120 that is present in the virus stock could have induced expression of CXCL10 protein. Fresh cultures were therefore inoculated with different concentrations of recombinant gp120 derived from macrophage-tropic (BAL) and lymphocyte-tropic (IIIB) HIV. Gp120IIIB failed to induce CXCL10 in the cultures (data not shown). Figure 3C shows a dose curve of CXCL10 induction by gp120BAL. Although gp120 at a concentration of 10 ng/ml induced expression of CXCL10, the maximal effect was observed with 100 ng/ml. Higher concentrations did not show a further increase in CXCL10 expression. Heat-inactivated gp120 failed to induce CXCL10 in these cells.
Exogenous CXCL10-Induced Apoptosis in Fetal Brain Cultures
To verify whether overexpression of CXCL10 could play a role in neuronal dysfunction, we performed studies to assess the effect of exogenous CXCL10 on the alterations in membrane permeability and on the viability of neuronal cells. The present study was performed in fetal brain cultures and in NT-2 neurons. Fetal brain cultures were used because they adequately mimic the in vivo cellular milieu of neurons. However, in this mixed culture almost 30% of the cells are comprised of astrocytes. Therefore, confirmation of our studies was also performed in differentiated NT-2 cells that are more than 95% neuronal in their phenotype. Treatment of fetal brain cultures and NT-2 neurons with increasing amounts of exogenous CXCL10 led to increased membrane permeability as assessed by staining with propidium iodide (Table 1). The changes in membrane permeability were more striking after 6 days of treatment with CXCL10 compared to treatment for 3 days. In addition to causing increased permeability, CXCL10, used at a concentration of 10 ng/ml, also caused cell loss of ∼20 to 40% in the fetal brain cultures (Table 1) and in the NT-2 neurons at 48 hours after treatment (data not shown). Because the effect was basically similar in the two cell types, we presumed that neurons were the primary target of the chemokine in the fetal brain cultures. These findings suggested that induction of apoptosis-related mechanisms might be responsible for these events.
Table 1.
Effect of Exogenous CXCL10 on Membrane Permeability and Cell Viability in Fetal Neuronal Cultures
| 10 ng/ml | 100 ng/ml | |
|---|---|---|
| Membrane permeability after 6 days of exposure to CXCL10* | ++ | ++ |
| Neuronal cell growth inhibition/cell loss† | ++ | +++ |
Fetal neuronal cultures treated with CXCL10 for 3 to 6 days, cells were harvested, stained with PI solution for 30 minutes and analyzed by FACS. membrane permeability: +, 1.5 to 2.9-fold increase of PI staining; ++, 3.0 to 4.9-fold increase of PI staining; +++, 5 to 7.9-fold increase of PI staining.
Cell growth inhibition: +: 10 to 20%; ++: 21 to 40%.
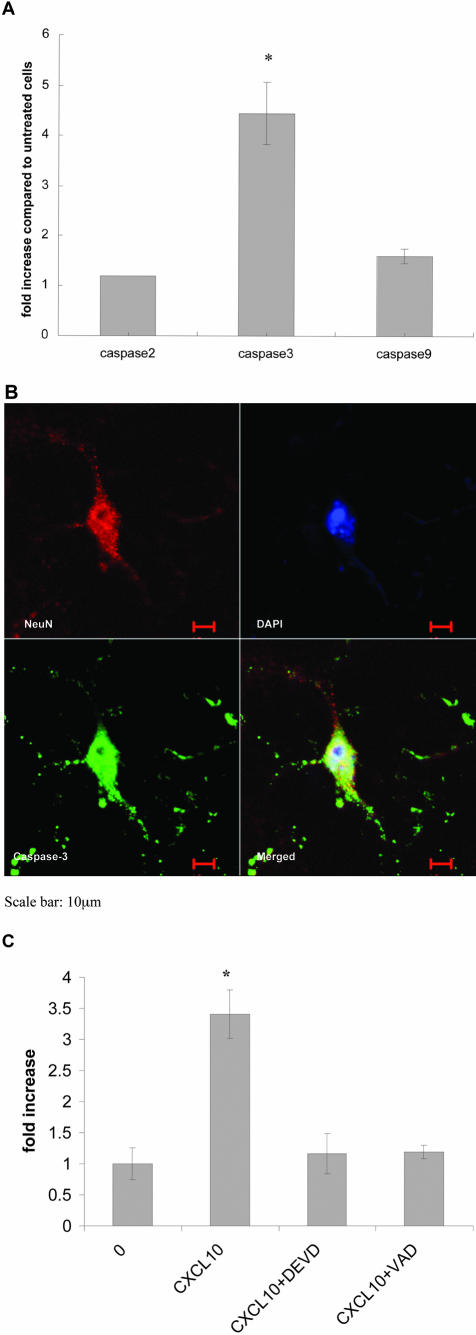
To determine whether CXCL10-induced damage in neuronal cultures was mediated via the apoptotic pathway, we asked whether caspases, a family of proteases that are involved in signal transduction of apoptotic stimuli,35 had become activated. Fetal brain cultures were exposed to CXCL10 (10 to 100 ng/ml) for 16 to 24 hours and the ApoAlert Caspase Profiling Assay was used to measure activation of caspase-2, -3, and -9, simultaneously. As shown in Figure 4A, CXCL10-treated neurons developed a 4- to 4.9-fold increase in caspase-3 activation compared to untreated neurons. Among the various caspases involved in transmitting the apoptotic stimuli, caspase-3 is the major downstream effector of the cascade and is activated in several neurodegenerative disorders.36–38
Figure 4.
A: Activation of caspases in fetal neuronal cultures treated with exogenous CXCL10. Fetal neuronal cultures were treated with CXCL10. Later (18 to 24 hours) the cells were lysed and the supernatant collected. One hundred μl of the lysates were then transferred into each well of the ApoAlert caspase profiling assay plate and incubated at 37°C for 2 hours. A CytoFluor fluorescence plate reader was used for fluorescence measurements. The increase in fluorescence by the various activated caspases is shown as fold increase relative to untreated cells. B: Caspase-3 activation in neurons in fetal neuronal cultures treated with exogenous CXCL10. Fetal neuronal cultures treated with exogenous CXCL10 were immunostained with anti-Neu N (red) and anti-caspase-3 (green) antibodies. DAPI (blue stain) was also applied to stain the nuclei. Caspase-3 was observed in the neurons. C: TUNEL ELISA of fetal neuronal cultures treated with exogenous CXCL10. Exposure of fetal brain cells to CXCL10 demonstrated a significant increase in apoptosis as detected by TUNEL ELISA. This increase in apoptosis was prevented by caspase inhibitors, zVAD-fmk or DEVD-fmk. *, Statistical significance compared to untreated cultures.
To determine whether active caspase-3 was present specifically in neurons, after treatment with CXCL10, fetal neuronal cultures were stained with antibodies specific for caspase-3 and the neuron-specific marker NeuN. As shown in Figure 4B, chemokine treatment resulted in a significant increase in caspase-3 staining in neurons 18 hours after exposure to CXCL10. Moreover, the staining pattern manifested both cytoplasmic and nuclear localization of caspase-3 in the neurons (Figure 4B). We found a similar staining pattern in NT-2 cells treated with CXCL10 (data not shown), demonstrating the apoptotic effect of the chemokine was specific for neurons.
To further determine whether CXCL10 could induce neuronal apoptosis, we conducted TUNEL analysis to determine the extent of genomic DNA strand breaks triggered by the chemokine. Fetal neuronal cultures/neuronal NT-2 cells were treated with CXCL10 for 3 to 6 days and then analyzed by the TUNEL assays to detect the presence of fragmented DNA. Consistent with data shown in Figure 4B, increased TUNEL activity in cells treated with the CXCL10 was demonstrated by TUNEL ELISA assays (Figure 4C). Pre-treatment of the cells with a pan-caspase inhibitor, zVAD-fmk or a caspase-3-specific inhibitor DEVD-fmk, followed by exogenous CXCL10 treatment led to a decrease in TUNEL activity (Figure 4C).
In our efforts to extrapolate the findings in cell cultures of CXCL10-mediated induction of caspase-3 to those in the brains of macaques with SHIV-E, we asked whether overexpression of CXCL10 in the neurons correlated with activation of caspase-3 in these cells. Consistent with the in vitro caspase-3 staining in CXCL10-treated fetal neuronal cultures; we found that SHIV-E brain sections positively stained for the active form of caspase-3 (Figure 5). Using confocal microscopy, we showed that caspase-3 co-localized in cells expressing CXCL10 in the brain sections with SHIV-E (Figure 5). The phenotype of these cells resembled neurons. Neurons in brain sections of macaques without SHIV-E did not express CXCL10 or active caspase-3. Further confirmation of neuronal apoptosis in the SHIV-E brain was also demonstrated by TUNEL in situ staining of the macaque brain sections (data not shown).
Figure 5.
Co-localization of CXCL10 and caspase-3 in the brains of SHIV89.6P-infected macaque with encephalitis. Basal ganglia regions of the brain from SHIV-E macaques were double immunostained with anti-CXCL10 (red) and anti-caspase-3 (green) antibodies. Confocal microscopy analysis showed that CXCL10 co-localized with caspase-3 in the SHIV-E brain sections (merged image).
To understand whether there was any relevance of these findings in the human disease, we stained sections of the basal ganglia from brains of patients infected with HIV, with and without the encephalitis. As shown in Figure 6, analogous to the macaque disease, we found co-localization of CXCL10 in the neurons in the brains of patients with HIV-E. CXCL10 expression was significantly up-regulated in patients with encephalitis as compared to HIV-infected individuals without the CNS disease. Brains of uninfected controls did not express this chemokine.
Figure 6.
Localization of CXCL10 in the neurons in the brains of patients with HIV-E. Basal ganglia region of the brain from individuals with HIV-E was double immunostained with anti-CXCL10 (red) and anti-MAP-2 (green) antibodies. Confocal microscopy analysis showed that CXCL10 localized in the neurons in the HIV-E brain sections (merged image).
Discussion
A large number of HIV-1-infected individuals develop varying degrees of neurological deterioration collectively termed as HAD. Neurons are not infected by the virus, therefore the mechanism of neuronal injury in HAD remains speculative. In this study, we demonstrated for the first time that overexpression of a CXC chemokine, CXCL10 in the neurons in the brains of macaques with SHIV-E is a possible cause of neuronal injury in HAD. Earlier reports have shown that CXCL10 is always present in the cerebrospinal fluid of HIV-I-infected patients and is absent in uninfected control individuals.25,26 Increased levels of CXCL10 have also been observed in the brains of HIV-1-infected individuals,25 and in macaques with SIV28 and SHIV-E21 and furthermore, CXCL10 levels were closely associated with the progression of HIV-1-related CNS infection and neuropyschiatric impairment.25 However, the cellular source of this chemokine in HAD still remains unclear. Although constitutive expression of the CXCL10 receptor, CXCR3, has been documented in neurons,34 our studies showed that enhanced expression of the ligand was confined to neurons in both macaques and humans with lentiviral neurological disease, and these were associated with degenerative changes in the neurons.
In our efforts to explore whether expression of CXCL10 and its receptor could play a role in HIV-associated neuronal injury, and the implied dementia, we demonstrated that treatment of fetal neuronal cultures and NT-2 neurons with increasing concentrations of exogenous CXCL10 resulted in increased membrane permeability and increased cell loss, presumably via apoptotic mechanisms. Because apoptosis is mediated by activation of caspases, we inquired whether caspase-3 was activated in neuronal cultures treated with the chemokine. We found that neurons treated with exogenous CXCL10 showed a strong staining for active caspase-3 expression by immunocytochemistry. Furthermore, pre-treatment ofthe cells with a caspase-3-specific inhibitor DEVD-fmk protected the cells from CXCL10-induced apoptosis. These data strongly suggested that CXCL10-mediated apoptosis involved specific activation of caspase-3. Confirmation of these cell culture findings was obtained from studies in the brains of macaques with SHIV-E wherein we demonstrated co-localization of CXCL10 and caspase-3 in the neurons in the CNS. This is the first report showing that capsase-3-positive cells also expressed CXCL10, extending previous reports that HIV-E is associated with an increase in neuronal immunoreactivity for the active form of caspase-3.39,40 Clinical relevance of our findings was further demonstrated by localization of overexpressed CXCL10 in the neurons in brains of individuals with HIV-E. These results suggest a novel role for this chemokine in HIV dementia.
The mechanism of CXCL10 overexpression in neurons still remains to be determined. HIV-E is usually associated with infection with viruses that use the CCR5 co-receptor, although it has been demonstrated recently that viruses that use CXCR4 can also cause the disease.41 SHIV-E has been clearly associated with viruses that use the CXCR4 co-receptor.21,42,43 The common factor shared by these viruses was their tropism for macrophages. Because expression of CXCL10 in neuronal cultures could only be induced with gp120 of macrophage-tropic HIVBAL, and it is known that neurons express both CXCR4 and CCR5 co-receptors,44,45 it is possible that overexpression of CXCL10 in the encephalitic brains was induced by viral gp120, irrespective of the co-receptor usage of the causative virus. The viral glycoprotein released from the infected macrophages in the microglial nodule in the encephalitic animals could thus be the initial trigger that causes enhanced expression of the chemokine in neurons. It remains to be determined whether other viral proteins such as tat or CXCL10 itself could induce the chemokine expression thereby amplifying the response further.
These findings suggest that viral proteins from the infected cells cause neuronal injury not only though direct toxic pathways, but also through indirect pathways by induction of neuronal CXCL10 expression, leading ultimately to neuronal apoptosis. Future studies aimed at the development of therapeutic strategies for AIDS-associated CNS disorders could therefore include CXCR3 antagonists and inhibitors of CXCL10.
Acknowledgments
We thank Mingzhao Huang and Fenglan Jia for technical assistance; and the AIDS Research and Reference Reagent Program, Division of AIDS, National Institute of Allergy and Infectious Diseases, National Institutes of Health, for HIV-1 Bal gp120.
Footnotes
Address reprint requests to Shilpa J. Buch, Ph.D., Department of Microbiology, Immunology and Molecular Genetics, 5000 Wahl Hall East, University of Kansas Medical Center, 3901 Rainbow Blvd., Kansas City, KS 66160. E-mail: sbuch@kumc.edu.
Supported by the National Institutes of Health (grants MH-62969-01, AI-29382, NS-32203, RR-16443, and MH068212).
References
- Sacktor N, Lyles RH, Skolasky R, Kleeberger C, Selnes OA, Miller EN, Becker JT, Cohen B, McArthur JC. HIV-associated neurologic disease incidence changes: Multicenter AIDS Cohort Study, 1990–1998. Neurology. 2001;56:257–260. doi: 10.1212/wnl.56.2.257. [DOI] [PubMed] [Google Scholar]
- Budka H. Neuropathology of human immunodeficiency virus infection. Brain Pathol. 1991;1:163–175. doi: 10.1111/j.1750-3639.1991.tb00656.x. [DOI] [PubMed] [Google Scholar]
- McArthur JC, Hoover DR, Bacellar H, Miller EN, Cohen BA, Becker JT, Graham NM, McArthur JH, Selnes OA, Jacobson LP. Dementia in AIDS patients: incidence and risk factors. Multicenter AIDS Cohort Study. Neurology. 1993;43:2245–2252. doi: 10.1212/wnl.43.11.2245. [DOI] [PubMed] [Google Scholar]
- Spencer DC, Price RW. Human immunodeficiency virus and the central nervous system. Annu Rev Microbiol. 1992;46:655–693. doi: 10.1146/annurev.mi.46.100192.003255. [DOI] [PubMed] [Google Scholar]
- Price RW, Sidtis JJ, Brew BJ. AIDS dementia complex and HIV-1 infection: a view from the clinic. Brain Pathol. 1991;1:155–162. doi: 10.1111/j.1750-3639.1991.tb00655.x. [DOI] [PubMed] [Google Scholar]
- Lipton SA, Gendelman HE. Seminars in medicine of the Beth Israel Hospital, Boston. Dementia associated with the acquired immunodeficiency syndrome. N Engl J Med. 1995;332:934–940. doi: 10.1056/NEJM199504063321407. [DOI] [PubMed] [Google Scholar]
- Bell JE. The neuropathology of adult HIV infection. Rev Neurol (Paris) 1998;154:816–829. [PubMed] [Google Scholar]
- Gendelman HE, Lipton SA, Tardieu M, Bukrinsky MI, Nottet HS. The neuropathogenesis of HIV-1 infection. J Leukoc Biol. 1994;56:389–398. doi: 10.1002/jlb.56.3.389. [DOI] [PubMed] [Google Scholar]
- Nath A. Pathobiology of human immunodeficiency virus dementia. Semin Neurol. 1999;19:113–127. doi: 10.1055/s-2008-1040830. [DOI] [PubMed] [Google Scholar]
- Kaul M, Garden GA, Lipton SA. Pathways to neuronal injury and apoptosis in HIV-associated dementia. Nature. 2001;410:988–994. doi: 10.1038/35073667. [DOI] [PubMed] [Google Scholar]
- Brenneman DE, Westbrook GL, Fitzgerald SP, Ennist DL, Elkins KL, Ruff MR, Pert CB. Neuronal cell killing by the envelope protein of HIV and its prevention by vasoactive intestinal peptide. Nature. 1988;335:639–642. doi: 10.1038/335639a0. [DOI] [PubMed] [Google Scholar]
- Dreyer EB, Kaiser PK, Offermann JT, Lipton SA. HIV-1 coat protein neurotoxicity prevented by calcium channel antagonists. Science. 1990;248:364–367. doi: 10.1126/science.2326646. [DOI] [PubMed] [Google Scholar]
- New DR, Ma M, Epstein LG, Nath A, Gelbard HA. Human immunodeficiency virus type 1 Tat protein induces death by apoptosis in primary human neuron cultures. J Neurovirol. 1997;3:168–173. doi: 10.3109/13550289709015806. [DOI] [PubMed] [Google Scholar]
- Adamson DC, Dawson TM, Zink MC, Clements JE, Dawson VL. Neurovirulent simian immunodeficiency virus infection induces neuronal, endothelial, and glial apoptosis. Mol Med. 1996;2:417–428. [PMC free article] [PubMed] [Google Scholar]
- Kruman I, Guo Q, Mattson MP. Calcium and reactive oxygen species mediate staurosporine-induced mitochondrial dysfunction and apoptosis in PC12 cells. J Neurosci Res. 1998;51:293–308. doi: 10.1002/(SICI)1097-4547(19980201)51:3<293::AID-JNR3>3.0.CO;2-B. [DOI] [PubMed] [Google Scholar]
- Hof PR, Lee PY, Yeung G, Wang RF, Podos SM, Morrison JH. Glutamate receptor subunit GluR2 and NMDAR1 immunoreactivity in the retina of macaque monkeys with experimental glaucoma does not identify vulnerable neurons. Exp Neurol. 1998;153:234–241. doi: 10.1006/exnr.1998.6881. [DOI] [PubMed] [Google Scholar]
- Patel CA, Mukhtar M, Pomerantz RJ. Human immunodeficiency virus type 1 Vpr induces apoptosis in human neuronal cells. J Virol. 2000;74:9717–9726. doi: 10.1128/jvi.74.20.9717-9726.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen Z, Huang Y, Zhao X, Skulsky E, Lin D, Ip J, Gettie A, Ho DD. Enhanced infectivity of an R5-tropic simian/human immunodeficiency virus carrying human immunodeficiency virus type 1 subtype C envelope after serial passages in pig-tailed macaques (Macaca nemestrina). J Virol. 2000;74:6501–6510. doi: 10.1128/jvi.74.14.6501-6510.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mennicken F, Maki R, de Souza EB, Quirion R. Chemokines and chemokine receptors in the CNS: a possible role in neuroinflammation and patterning. Trends Pharmacol Sci. 1999;20:73–78. doi: 10.1016/s0165-6147(99)01308-5. [DOI] [PubMed] [Google Scholar]
- Asensio VC, Campbell IL. Chemokines in the CNS: plurifunctional mediators in diverse states. Trends Neurosci. 1999;22:504–512. doi: 10.1016/s0166-2236(99)01453-8. [DOI] [PubMed] [Google Scholar]
- Sui Y, Potula R, Pinson D, Adany I, Li Z, Buch E, Segerbrecht J, Villinger F, Narayan O, Buch S. Analysis of cytokine and chemokine genes in the brains of macaques with SHIV-encephalitis. J Med Primatol. 2003;32:229–239. doi: 10.1034/j.1600-0684.2003.00030.x. [DOI] [PubMed] [Google Scholar]
- Luster AD, Ravetch JV. Biochemical characterization of a gamma interferon-inducible cytokine (IP-10). J Exp Med. 1987;166:1084–1097. doi: 10.1084/jem.166.4.1084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luster AD, Unkeless JC, Ravetch JV. Gamma-interferon transcriptionally regulates an early-response gene containing homology to platelet proteins. Nature. 1985;315:672–676. doi: 10.1038/315672a0. [DOI] [PubMed] [Google Scholar]
- Asensio VC, Maier J, Milner R, Boztug K, Kincaid C, Moulard M, Phillipson C, Lindsley K, Krucker T, Fox HS, Campbell IL. Interferon-independent, human immunodeficiency virus type 1 gp120-mediated induction of CXCL10/IP-10 gene expression by astrocytes in vivo and in vitro. J Virol. 2001;75:7067–7077. doi: 10.1128/JVI.75.15.7067-7077.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kolb SA, Sporer B, Lahrtz F, Koedel U, Pfister HW, Fontana A. Identification of a T cell chemotactic factor in the cerebrospinal fluid of HIV-1-infected individuals as interferon-gamma inducible protein 10. J Neuroimmunol. 1999;93:172–181. doi: 10.1016/s0165-5728(98)00223-9. [DOI] [PubMed] [Google Scholar]
- Lahrtz F, Piali L, Nadal D, Pfister HW, Spanaus KS, Baggiolini M, Fontana A. Chemotactic activity on mononuclear cells in the cerebrospinal fluid of patients with viral meningitis is mediated by interferon-gamma inducible protein-10 and monocyte chemotactic protein-1. Eur J Immunol. 1997;27:2484–2489. doi: 10.1002/eji.1830271004. [DOI] [PubMed] [Google Scholar]
- Sanders VJ, Pittman CA, White MG, Wang G, Wiley CA, Achim CL. Chemokines and receptors in HIV encephalitis. AIDS. 1998;12:1021–1026. [PubMed] [Google Scholar]
- Sasseville VG, Smith MM, Mackay CR, Pauley DR, Mansfield KG, Ringler DJ, Lackner AA. Chemokine expression in simian immunodeficiency virus-induced AIDS encephalitis. Am J Pathol. 1996;149:1459–1467. [PMC free article] [PubMed] [Google Scholar]
- Westmoreland SV, Rottman JB, Williams KC, Lackner AA, Sasseville VG. Chemokine receptor expression on resident and inflammatory cells in the brain of macaques with simian immunodeficiency virus encephalitis. Am J Pathol. 1998;152:659–665. [PMC free article] [PubMed] [Google Scholar]
- Coughlan CM, McManus CM, Sharron M, Gao Z, Murphy D, Jaffer S, Choe W, Chen W, Hesselgesser J, Gaylord H, Kalyuzhny A, Lee VM, Wolf B, Doms RW, Kolson DL. Expression of multiple functional chemokine receptors and monocyte chemoattractant protein-1 in human neurons. Neuroscience. 2000;97:591–600. doi: 10.1016/s0306-4522(00)00024-5. [DOI] [PubMed] [Google Scholar]
- Llanes C, Collman RG, Hrin R, Kolson DL. Acetylcholinesterase expression in NTera 2 human neuronal cells: a model for developmental expression in the nervous system. J Neurosci Res. 1995;42:791–802. doi: 10.1002/jnr.490420608. [DOI] [PubMed] [Google Scholar]
- Ensoli F, Fiorelli V, DeCristofaro M, Santini MD, Novi A, Vannelli B, Thiele CJ, Luzi G, Aiuti F. Inflammatory cytokines and HIV-1-associated neurodegeneration: oncostatin-M produced by mononuclear cells from HIV-1-infected individuals induces apoptosis of primary neurons. J Immunol. 1999;162:6268–6277. [PubMed] [Google Scholar]
- Hicks A, Potula R, Sui YJ, Villinger F, Pinson D, Adany I, Li Z, Long C, Cheney P, Marcario J, Novembre F, Mueller N, Kumar A, Major E, Narayan O, Buch S. Neuropathogenesis of lentiviral infection in macaques: roles of CXCR4 and CCR5 viruses and interleukin-4 in enhancing monocyte chemoattractant protein-1 production in macrophages. Am J Pathol. 2002;161:813–822. doi: 10.1016/S0002-9440(10)64241-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xia MQ, Bacskai BJ, Knowles RB, Qin SX, Hyman BT. Expression of the chemokine receptor CXCR3 on neurons and the elevated expression of its ligand IP-10 in reactive astrocytes: in vitro ERK1/2 activation and role in Alzheimer’s disease. J Neuroimmunol. 2000;108:227–235. doi: 10.1016/s0165-5728(00)00285-x. [DOI] [PubMed] [Google Scholar]
- Stennicke HR, Salvesen GS. Caspase assays. Methods Enzymol. 2000;322:91–100. doi: 10.1016/s0076-6879(00)22010-7. [DOI] [PubMed] [Google Scholar]
- Namura S, Zhu J, Fink K, Endres M, Srinivasan A, Tomaselli KJ, Yuan J, Moskowitz MA. Activation and cleavage of caspase-3 in apoptosis induced by experimental cerebral ischemia. J Neurosci. 1998;18:3659–3668. doi: 10.1523/JNEUROSCI.18-10-03659.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hartmann A, Hunot S, Michel PP, Muriel MP, Vyas S, Faucheux BA, Mouatt-Prigent A, Turmel H, Srinivasan A, Ruberg M, Evan GI, Agid Y, Hirsch EC. Caspase-3: a vulnerability factor and final effector in apoptotic death of dopaminergic neurons in Parkinson’s disease. Proc Natl Acad Sci USA. 2000;97:2875–2880. doi: 10.1073/pnas.040556597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Su JH, Nichol KE, Sitch T, Sheu P, Chubb C, Miller BL, Tomaselli KJ, Kim RC, Cotman CW. DNA damage and activated caspase-3 expression in neurons and astrocytes: evidence for apoptosis in frontotemporal dementia. Exp Neurol. 2000;163:9–19. doi: 10.1006/exnr.2000.7340. [DOI] [PubMed] [Google Scholar]
- James HJ, Sharer LR, Zhang Q, Wang HG, Epstein LG, Reed JC, Gelbard HA. Expression of caspase-3 in brains from paediatric patients with HIV-1 encephalitis. Neuropathol Appl Neurobiol. 1999;25:380–386. doi: 10.1046/j.1365-2990.1999.00195.x. [DOI] [PubMed] [Google Scholar]
- Garden GA, Budd SL, Tsai E, Hanson L, Kaul M, D’Emilia DM, Friedlander RM, Yuan J, Masliah E, Lipton SA. Caspase cascades in human immunodeficiency virus-associated neurodegeneration. J Neurosci. 2002;22:4015–4024. doi: 10.1523/JNEUROSCI.22-10-04015.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yi YJ, Chen W, Frank I, Cutilli J, Singh A, Starr-Spires L, Sulcove J, Kolson DL, Collman RG. An unusual syncytia-inducing human immunodeficiency virus type 1 primary isolate from the central nervous system that is restricted to CXCR4, replicates efficiently in macrophages, and induces neuronal apoptosis. J Neurovirol. 2003;9:432–441. doi: 10.1080/13550280390218706. [DOI] [PubMed] [Google Scholar]
- Liu ZQ, Muhkerjee S, Sahni M, McCormick-Davis C, Leung K, Li Z, Gattone VH, Tian C, Doms RW, Hoffman TL, Raghavan R, Narayan O, Stephens EB. Derivation and biological characterization of a molecular clone of SHIV(KU-2) that causes AIDS, neurological disease, and renal disease in rhesus macaques. Virology. 1999;260:295–307. doi: 10.1006/viro.1999.9812. [DOI] [PubMed] [Google Scholar]
- Gorry PR, Bristol G, Zack JA, Ritola K, Swanstrom R, Birch CJ, Bell JE, Bannert N, Crawford K, Wang H, Schols D, De Clercq E, Kunstman K, Wolinsky SM, Gabuzda D. Macrophage tropism of human immunodeficiency virus type 1 isolates from brain and lymphoid tissues predicts neurotropism independent of coreceptor specificity. J Virol. 2001;75:10073–10089. doi: 10.1128/JVI.75.21.10073-10089.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oh SB, Endoh T, Simen AA, Ren D, Miller RJ. Regulation of calcium currents by chemokines and their receptors. J Neuroimmunol. 2002;123:66–75. doi: 10.1016/s0165-5728(01)00485-4. [DOI] [PubMed] [Google Scholar]
- Klein RS, Williams KC, Alvarez-Hernandez X, Westmoreland S, Force T, Lackner AA, Luster AD. Chemokine receptor expression and signaling in macaque and human fetal neurons and astrocytes: implications for the neuropathogenesis of AIDS. J Immunol. 1999;163:1636–1646. [PubMed] [Google Scholar]