Abstract
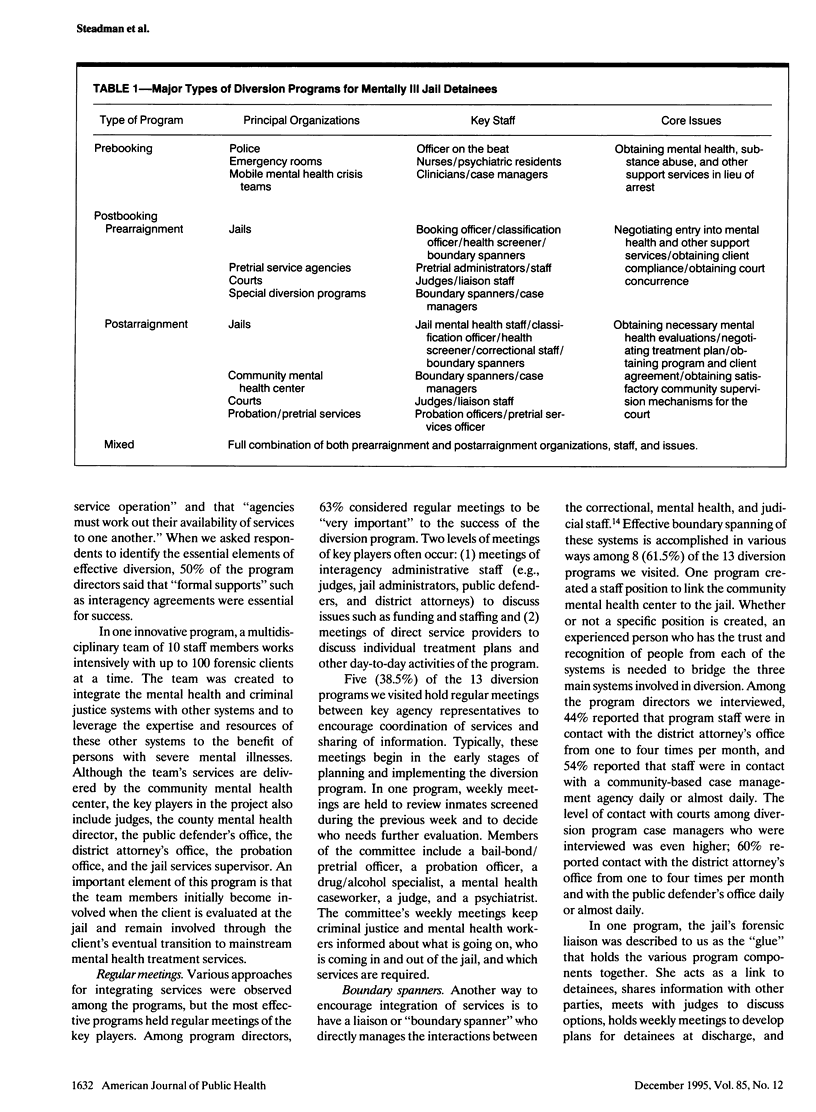
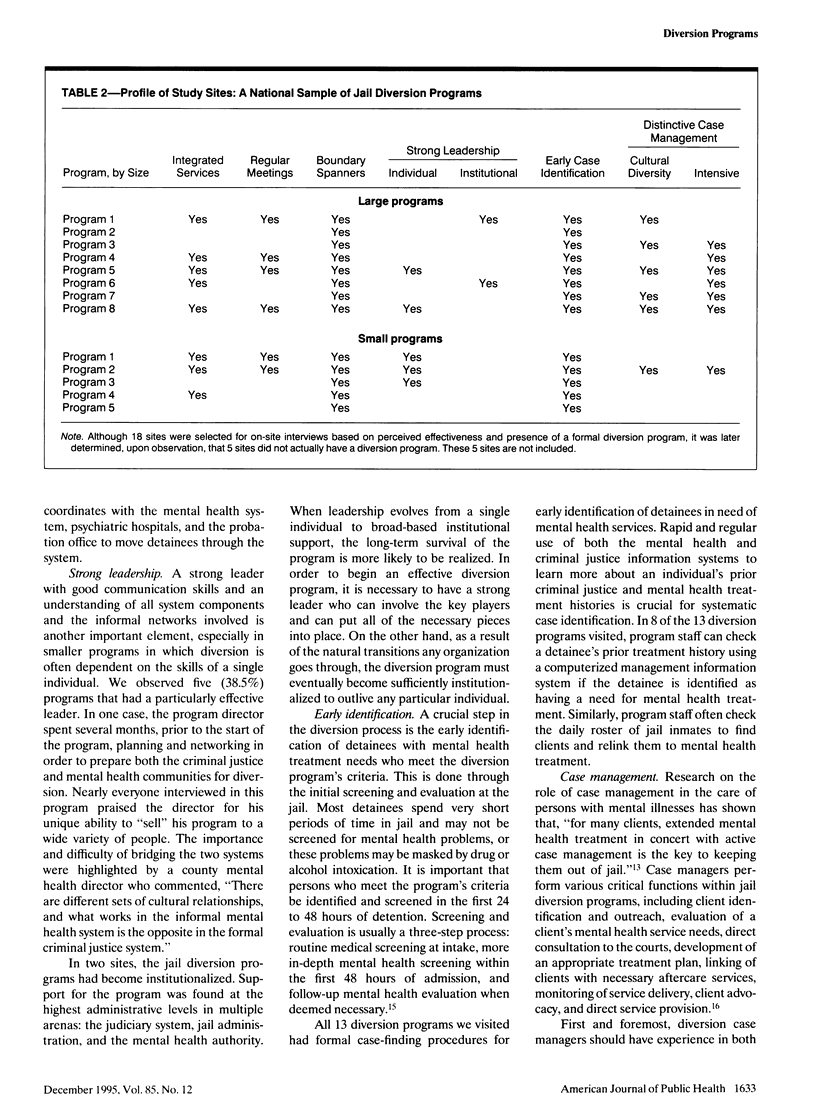
OBJECTIVES. A major proposal for appropriately treating persons with mental illnesses who have been arrested is to divert them from jail to community-based mental health programs. However, there are few available definitions, guidelines, and principles for developing effective diversion programs. The goal of this research was to determine the number and kinds of jail diversion programs that exist, how they are set up, and which types of programs are effective. METHODS. On the basis of information gathered during a national mail survey (n = 1263) and follow-up telephone survey of 115 responding jails, 18 sites were selected for on-site interviews based on perceived effectiveness and presence of a formal diversion program. RESULTS. Data are presented from a national sample of jail diversion programs (n = 18). Key factors for developing diversion programs and descriptors of effective programs are presented. CONCLUSIONS. It is clear that controlled, longitudinal studies of these programs' effectiveness, using client-based and organizational outcome measures, are badly needed.
Full text
PDF


Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Anthony W. A., Cohen M., Farkas M., Cohen B. F. The chronically mentally ill case management--more than a response to a dysfunctional system. Community Ment Health J. 1988 Fall;24(3):219–228. doi: 10.1007/BF00757139. [DOI] [PubMed] [Google Scholar]
- Dorwart R. A., Schlesinger M. Privatization of psychiatric services. Am J Psychiatry. 1988 May;145(5):543–553. doi: 10.1176/ajp.145.5.543. [DOI] [PubMed] [Google Scholar]
- Rogers R., Bagby R. M. Diversion of mentally disordered offenders: a legitimate role for clinicians? Behav Sci Law. 1992 Summer;10(3):407–418. doi: 10.1002/bsl.2370100310. [DOI] [PubMed] [Google Scholar]
- Steadman H. J., Barbera S. S., Dennis D. L. A national survey of jail diversion programs for mentally ill detainees. Hosp Community Psychiatry. 1994 Nov;45(11):1109–1113. doi: 10.1176/ps.45.11.1109. [DOI] [PubMed] [Google Scholar]
- Steadman H. J., Ribner S. A. Changing perceptions of the mental health needs of inmates in local jails. Am J Psychiatry. 1980 Sep;137(9):1115–1116. doi: 10.1176/ajp.137.9.1115. [DOI] [PubMed] [Google Scholar]
- Teplin L. A. Psychiatric and substance abuse disorders among male urban jail detainees. Am J Public Health. 1994 Feb;84(2):290–293. doi: 10.2105/ajph.84.2.290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Teplin L. A. The criminalization of the mentally ill: speculation in search of data. Psychol Bull. 1983 Jul;94(1):54–67. doi: 10.1037/0033-2909.94.1.54. [DOI] [PubMed] [Google Scholar]
- Teplin L. A. The prevalence of severe mental disorder among male urban jail detainees: comparison with the Epidemiologic Catchment Area Program. Am J Public Health. 1990 Jun;80(6):663–669. doi: 10.2105/ajph.80.6.663. [DOI] [PMC free article] [PubMed] [Google Scholar]


