Abstract
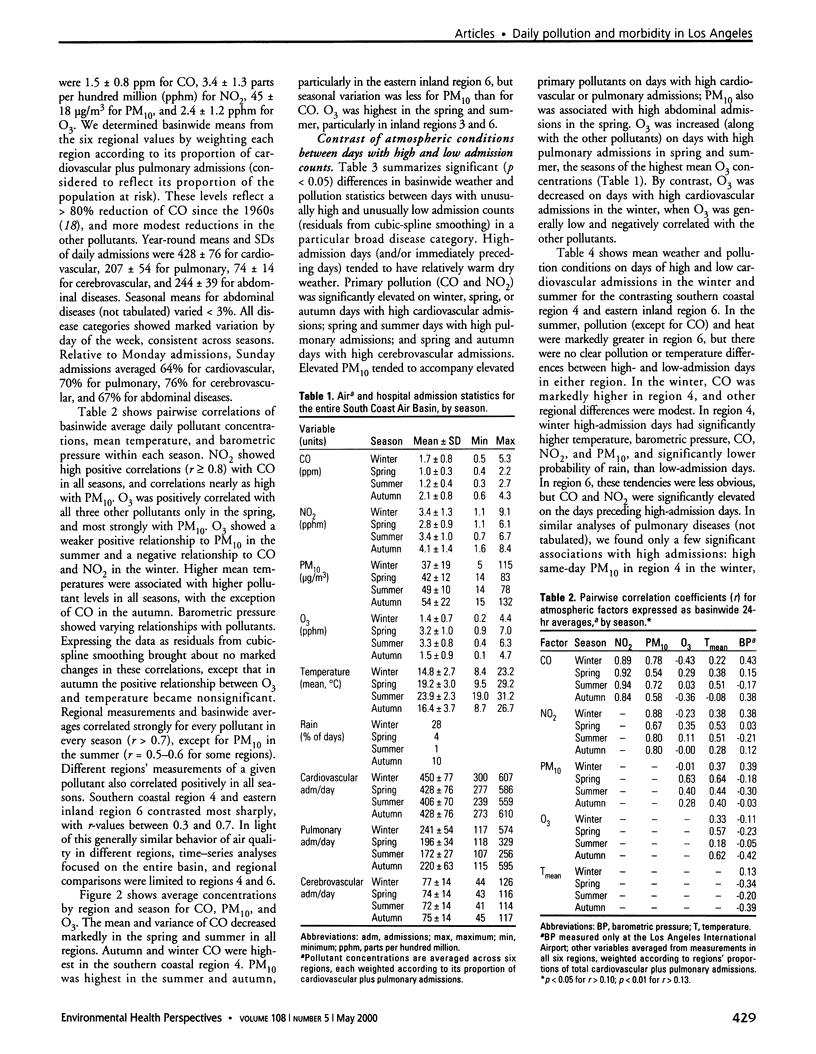
We used daily time-series analysis to evaluate associations between ambient carbon monoxide, nitrogen dioxide, particulate matter [less than and equal to] 10 microm in aerodynamic diameter (PM(10)), or ozone concentrations, and hospital admissions for cardiopulmonary illnesses in metropolitan Los Angeles during 1992-1995. We performed Poisson regressions for the entire patient population and for subgroups defined by season, region, or personal characteristics, allowing for effects of temporal variation, weather, and autocorrelation. CO showed the most consistently significant (p<0.05) relationships to cardiovascular admissions. A wintertime 25th-75th percentile increase in CO (1.1-2.2 ppm) predicted an increase of 4% in cardiovascular admissions. NO(2), and, to a lesser extent, PM(10) tracked CO and showed similar associations with cardiovascular disease, but O(3) was negatively or nonsignificantly associated. No significant demographic differences were found, although increased cardiovascular effects were suggested in diabetics, in whites and blacks (relative to Hispanics and Asians), and in persons older than 65 years of age. Pulmonary disease admissions associated more with NO(2) and PM(10) than with CO. Pulmonary effects were generally smaller than cardiovascular effects and were more sensitive to the choice of model. We conclude that in Los Angeles, atmospheric stagnation with high primary (CO/NO(2)/PM(10)) pollution, most common in autumn/winter, increases the risk of hospitalization for cardiopulmonary illness. Summer photochemical pollution (high O(3)) apparently presents less risk.
Full text
PDF






Images in this article
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Burnett R. T., Dales R. E., Brook J. R., Raizenne M. E., Krewski D. Association between ambient carbon monoxide levels and hospitalizations for congestive heart failure in the elderly in 10 Canadian cities. Epidemiology. 1997 Mar;8(2):162–167. doi: 10.1097/00001648-199703000-00007. [DOI] [PubMed] [Google Scholar]
- Burnett R. T., Smith-Doiron M., Stieb D., Cakmak S., Brook J. R. Effects of particulate and gaseous air pollution on cardiorespiratory hospitalizations. Arch Environ Health. 1999 Mar-Apr;54(2):130–139. doi: 10.1080/00039899909602248. [DOI] [PubMed] [Google Scholar]
- Dockery D. W., Pope C. A., 3rd Acute respiratory effects of particulate air pollution. Annu Rev Public Health. 1994;15:107–132. doi: 10.1146/annurev.pu.15.050194.000543. [DOI] [PubMed] [Google Scholar]
- Fisher E. S., Whaley F. S., Krushat W. M., Malenka D. J., Fleming C., Baron J. A., Hsia D. C. The accuracy of Medicare's hospital claims data: progress has been made, but problems remain. Am J Public Health. 1992 Feb;82(2):243–248. doi: 10.2105/ajph.82.2.243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayes S. R. Use of an indoor air quality model (IAQM) to estimate indoor ozone levels. J Air Waste Manage Assoc. 1991 Feb;41(2):161–170. doi: 10.1080/10473289.1991.10466833. [DOI] [PubMed] [Google Scholar]
- Hsia D. C., Ahern C. A., Ritchie B. P., Moscoe L. M., Krushat W. M. Medicare reimbursement accuracy under the prospective payment system, 1985 to 1988. JAMA. 1992 Aug 19;268(7):896–899. [PubMed] [Google Scholar]
- Janssen N. A., Hoek G., Brunekreef B., Harssema H., Mensink I., Zuidhof A. Personal sampling of particles in adults: relation among personal, indoor, and outdoor air concentrations. Am J Epidemiol. 1998 Mar 15;147(6):537–547. doi: 10.1093/oxfordjournals.aje.a009485. [DOI] [PubMed] [Google Scholar]
- Janssen N. A., Hoek G., Harssema H., Brunekreef B. Personal exposure to fine particles in children correlates closely with ambient fine particles. Arch Environ Health. 1999 Mar-Apr;54(2):95–101. doi: 10.1080/00039899909602242. [DOI] [PubMed] [Google Scholar]
- Kinney P. L., Ozkaynak H. Associations of daily mortality and air pollution in Los Angeles County. Environ Res. 1991 Apr;54(2):99–120. doi: 10.1016/s0013-9351(05)80094-5. [DOI] [PubMed] [Google Scholar]
- Korc M. E. A socioeconomic assessment of human exposure to ozone in the South Coast Air Basin of California. J Air Waste Manag Assoc. 1996 Jun;46(6):547–557. doi: 10.1080/10473289.1996.10467490. [DOI] [PubMed] [Google Scholar]
- Lipfert F. W., Wyzga R. E. Air pollution and mortality: the implications of uncertainties in regression modeling and exposure measurement. J Air Waste Manag Assoc. 1997 Apr;47(4):517–523. doi: 10.1080/10473289.1997.10464417. [DOI] [PubMed] [Google Scholar]
- Morris R. D., Naumova E. N. Carbon monoxide and hospital admissions for congestive heart failure: evidence of an increased effect at low temperatures. Environ Health Perspect. 1998 Oct;106(10):649–653. doi: 10.1289/ehp.98106649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morris R. D., Naumova E. N., Munasinghe R. L. Ambient air pollution and hospitalization for congestive heart failure among elderly people in seven large US cities. Am J Public Health. 1995 Oct;85(10):1361–1365. doi: 10.2105/ajph.85.10.1361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nauenberg E., Basu K. Effect of insurance coverage on the relationship between asthma hospitalizations and exposure to air pollution. Public Health Rep. 1999 Mar-Apr;114(2):135–148. [PMC free article] [PubMed] [Google Scholar]
- Peters A., Döring A., Wichmann H. E., Koenig W. Increased plasma viscosity during an air pollution episode: a link to mortality? Lancet. 1997 May 31;349(9065):1582–1587. doi: 10.1016/S0140-6736(97)01211-7. [DOI] [PubMed] [Google Scholar]
- Pope C. A., 3rd, Bates D. V., Raizenne M. E. Health effects of particulate air pollution: time for reassessment? Environ Health Perspect. 1995 May;103(5):472–480. doi: 10.1289/ehp.95103472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pope C. A., 3rd, Schwartz J. Time series for the analysis of pulmonary health data. Am J Respir Crit Care Med. 1996 Dec;154(6 Pt 2):S229–S233. doi: 10.1164/ajrccm/154.6_Pt_2.S229. [DOI] [PubMed] [Google Scholar]
- Schwartz J. Air pollution and hospital admissions for cardiovascular disease in Tucson. Epidemiology. 1997 Jul;8(4):371–377. doi: 10.1097/00001648-199707000-00004. [DOI] [PubMed] [Google Scholar]
- Schwartz J. Air pollution and hospital admissions for heart disease in eight U.S. counties. Epidemiology. 1999 Jan;10(1):17–22. [PubMed] [Google Scholar]
- Seaton A., MacNee W., Donaldson K., Godden D. Particulate air pollution and acute health effects. Lancet. 1995 Jan 21;345(8943):176–178. doi: 10.1016/s0140-6736(95)90173-6. [DOI] [PubMed] [Google Scholar]
- Sexton K., Gong H., Jr, Bailar J. C., 3rd, Ford J. G., Gold D. R., Lambert W. E., Utell M. J. Air pollution health risks: do class and race matter? Toxicol Ind Health. 1993 Sep-Oct;9(5):843–878. doi: 10.1177/074823379300900509. [DOI] [PubMed] [Google Scholar]
- Vedal S. Ambient particles and health: lines that divide. J Air Waste Manag Assoc. 1997 May;47(5):551–581. doi: 10.1080/10473289.1997.10463922. [DOI] [PubMed] [Google Scholar]




